Mandibular Postirradiation Osteosarcoma: Clinical Case Report
Abstract
Osteosarcoma is a malignant tumor of mesenchymall cells capable of producing osteoid tissue. Its age distribution is wide, being more common between the third and fourth decades of life. Mandibular tumors affect more the posterior region. Radiographic findings range from dense sclerosis to radiolucent lesions. More than 10% of osteosarcoma cases have etiology associated with previous radiotherapy. Female patient, 56-years-old, brown, complained of tingling and shock in the chin and fast growing swelling of the left mandible. Patient reported treatment with radiation and chemotherapy for Hodgkin's disease in the left parotid thirteen years ago. On clinical examination, facial asymmetry was observed, with vestibular rubbery normochromic swelling in the mandible and bottom of the left vestibule, symptomatic on palpation and extending from the canine to the molars, with dental marks on its surface. Panoramic radiography revealed radiolucency at the apex of the root of the first lower left premolar and two radiolucent images, one in each mandibular hemi-arch, extending from the molar region to the angle of the mandible. Computed tomography showed an axial section similar to sunrays. An intraosseous incision biopsy was performed with histopathological report of osteosarcoma. The patient was referred for treatment. Clinical and histopathological characteristics of the lesion influence the prognosis. Because it appeared in a region previously irradiated due to a primary tumor of non-bone origin, the long latency period and histopathological confirmation of osteosarcoma, this case fulfills the criteria for the diagnosis of postirradiation osteosarcoma.
Keywords
Neoplasm, Osteosarcoma, Mandible, Radiotherapy
Introduction
Osteosarcoma is a malignant tumor of primitive bone cells, capable of directly forming bone or osteoid tissue from malignant tumor cells [1]. It is the most prevalent bone neoplasia in children and adolescents, with a peak incidence between the second and third decades of life. It most frequently affects the metaphysis of long bones, in particular the distal portion of the femur, in addition to the proximal portion of the tibia and humerus [2]. The involvement of the head and neck region occurs in approximately 7% of cases. Most of the cases are located in the mandible and, less frequently, in the maxilla, in patients in the third and fourth decades of life [3].
The incidence is similar between female and male until the end of adolescence, when it becomes predominant in male [4]. The etiology is still unknown, with no specific predisposing factor. However, in some situations, such as in the presence of genetic syndromes (mainly Li-Fraumeni Syndrome) and in cases of bilateral retinoblastoma, there is a greater chance of development of the disease due to the association with abnormalities in the RB1 gene [4].
Sarcoma arises in the bone previously submitted to radiotherapy. It is unusual, but a well-recognized phenomenon. Gnathic and skull bones are among the most common sites for these sarcomas. Bone sarcomas have been reported to develop three to 55 years after exposure to radiation, with an average frequency of about four to 17 years. Studies estimate that 0.03% to 0.2% of patients develop postirradiation or soft tissue sarcomas. The risk apparently increases when the radiation dose increases. Average and median reported doses of irradiation in postirradiation bone sarcomas range from 43 to 64 Gy. Some researchers have suggested that the risk is neglected with doses less than 10 Gy; however, a recent prospective study of atomic bomb survivors in Japan, suggests an increased risk of bone sarcomas with a radiation dose below 0.85 Gy [5].
Osteosarcoma is the most common type of postirradiation sarcoma, accounting for 49% to 85% of all cases. Other types reported include undifferentiated pleomorphic sarcomas (malignant fibrous histiocytoma), fibrosarcoma and chondrosarcoma. Postirradiation bone sarcomas do not have distinct histopathological characteristics that allow them to be differentiated from other bone sarcomas of the same type that arise again. The lesions tend to be poorly differentiated, and the prognosis is generally poor [5]. The purpose of this article is to report a case of postirradiation osteosarcoma involving the mandible, and to describe its clinical, radiography and histopathological features.
Case Presentation
Female patient, 56-years-old, brown, attended the Stomatology Clinic of the Army Dental Service complaining of tingling, shock in the chin region and swelling in the left jaw, with rapid growth. She reported having been treated with radiotherapy and chemotherapy for Hodgkin's disease in the left parotid thirteen years ago.
On clinical examination, facial asymmetry was observed, with vestibular swelling in the left mandible and bottom of the vestibule, symptomatic on palpation and extending from the canine to the molars, with dental marks on its surface (Figure 1).
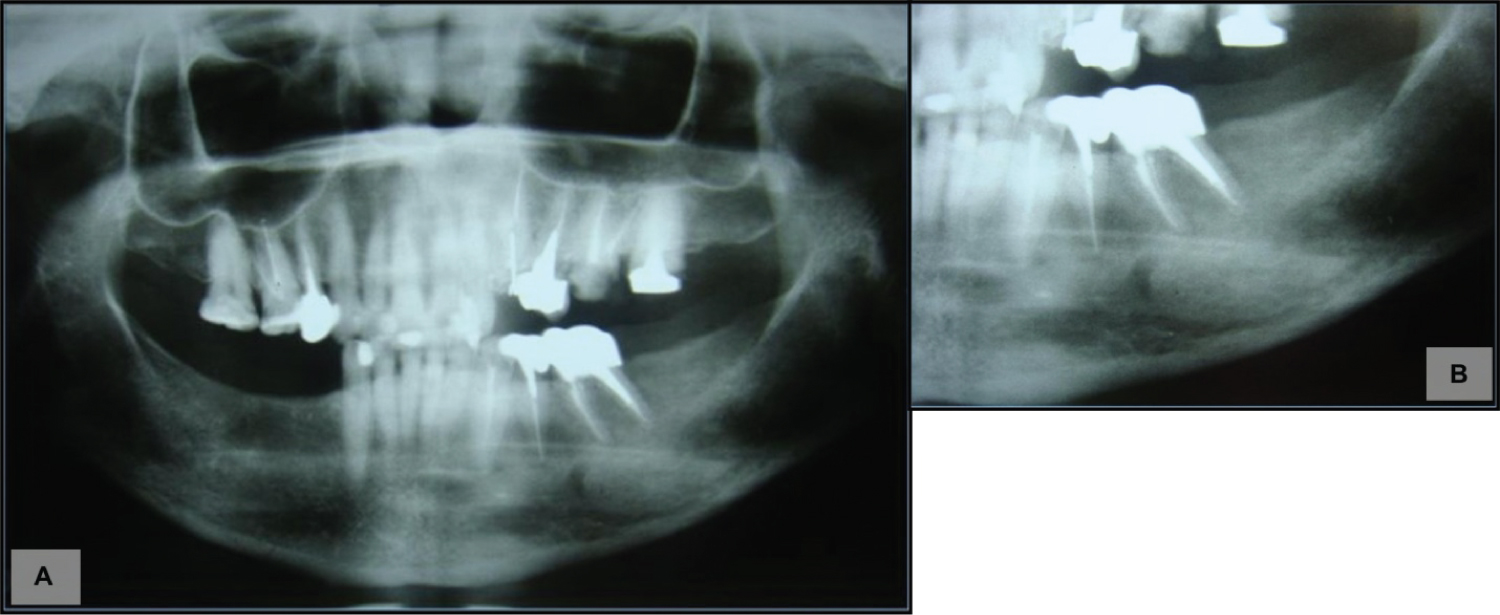
Panoramic radiography revealed radiolucency at the root apex of the lower left first premolar and two radiolucent images, one in each mandibular hemi-arch, extending from the molar region to the mandible angle (Figure 2).
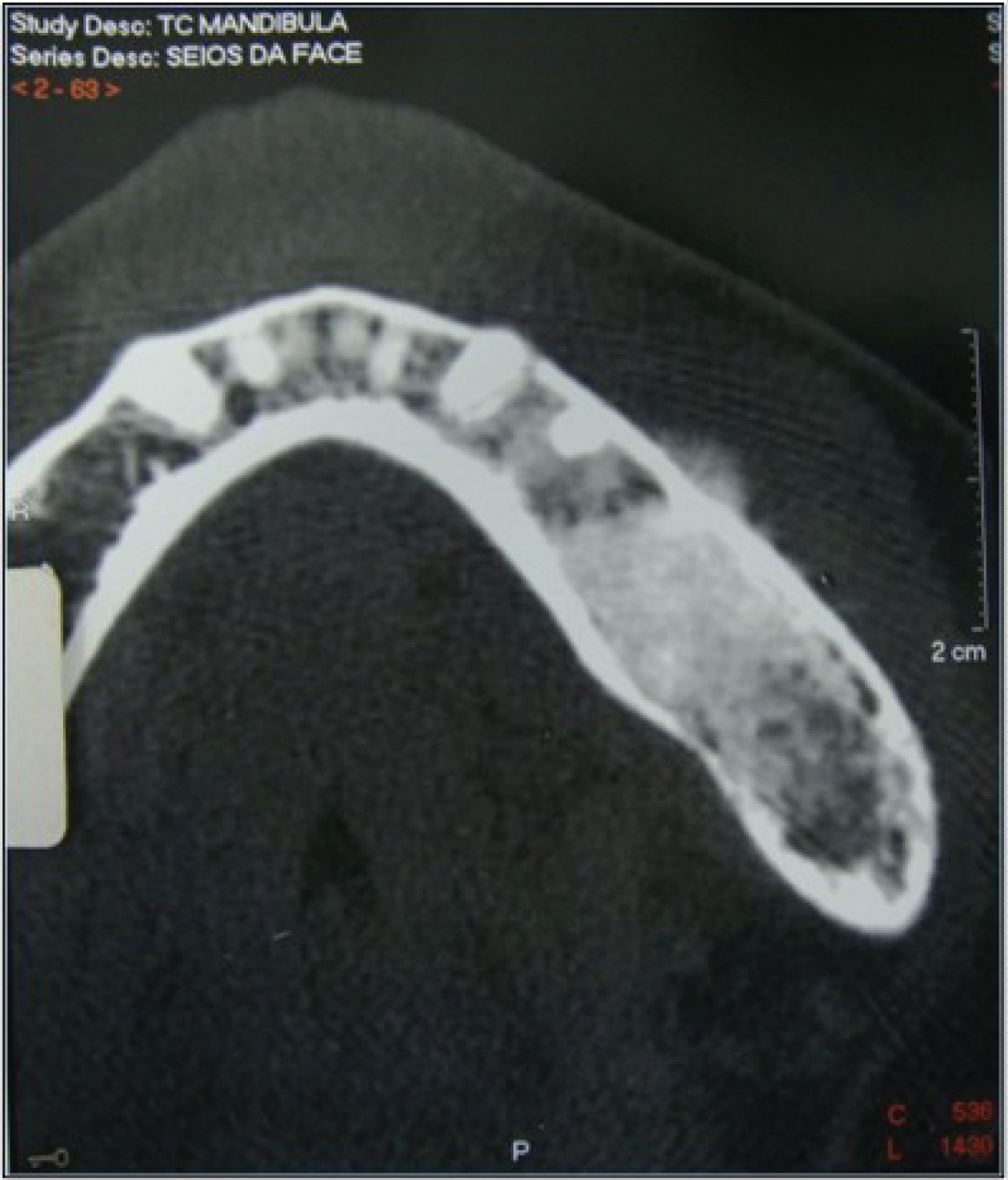
Computed tomography showed in axial section an image similar to sunrays (Figure 3).
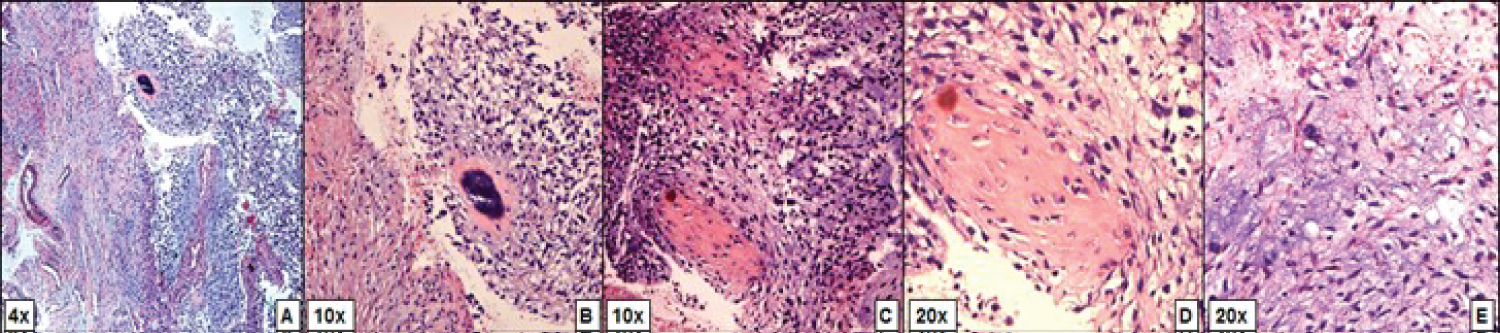
An Incisional biopsy of the lesion was performed, and the material sent to the Pathological Service. Histopathological analysis of 5-μm sections stained with hematoxylin and eosin (H&E) showed malignant mesenchymal cells interspersed with osteoid tissue, presence of osteoblastic differentiation, myxoid matrix, cellular pleomorphism and formation of chondroid tissue. The histopathological report was osteosarcoma (Figure 4).
The patient was referred for treatment with her oncologist, where she underwent rescue surgery with the head and neck surgeon, confirming the diagnosis of osteosarcoma. The patient is being followed up with no evidence of the disease.
Discussion
Tumors that affect the jaw can be primary or metastatic. Malignant tumors of the mandible include lymphomas, Ewing's sarcomas and osteosarcoma [3]. Osteosarcoma represents a group of malignant bone tumors being more frequent in long bones and with fewer incidences in the mandible [6]. Thus, the reported case is a rare manifestation of the tumor.
The etiological conditions that favor the development of osteosarcoma of the mandible are previous irradiation, Paget's bone disease, retinoblastoma, fibrous dysplasia and genetic predisposition [3,6]. In the reported case, the patient had previous exposure to radiation, which is one of the predisposing factors for the onset of this neoplasia. However, the literature shows that the incidence of sarcoma after radiotherapy ranges from 0.03% to 0.8%, and in the head and neck region, the incidence of radiation-induced carcinoma and sarcomas varies from 0.037% to 0.7%, showing the rarity of this manifestation [7].
Regarding the clinical findings, patients with primary mandible osteosarcoma present pain, edema, facial deformity, loss or mobility of the teeth, paresthesia or anesthesia of the affected area, nasal obstruction and epistaxis [3]. These findings were evidenced in the reported case.
The radiographic features found in this type of radiation-induced osteosarcoma vary from radiolucent lesions to areas of dense sclerosis or mixed pattern. Studies show that computed tomography made the diagnosis of radiation-induced sarcomas possible, since it allows the professional to visualize masses that are not expected from soft tissues [8-10]. In the reported case, computed tomography was performed and images like sunrays were found, an expected finding for mandibular osteosarcoma.
Regarding the prognosis, in most cases it is poor. In a study of six patients with osteosarcoma of the jaw, three died, two were alive, but with unrespectable tumor and only one was alive and without evidence of active disease [8,9]. In this case, the patient was referred to the oncology service and subsequently underwent surgery to treat the tumor, and so far, she has had no evidence of the disease.
Osteosarcoma in the jaw is uncommon, and in the case described, the patient reported treatment with previous radiotherapy for Hodgkin's disease thirteen years ago. More than 10% of osteosarcoma are associated with previous irradiation, and therefore, it is essential that a long-term monitoring of these patients by a multidisciplinary team is carried out correctly so that the detection of possible signs and symptoms occurs early, improving the prognosis.
In view of the exposed material, doctors and dentists must be attentive to the signs and symptoms of malignant diseases to proceed quickly with the biopsy and deliver a final diagnosis. It is known that the biopsy of the lesion is crucial for early diagnosis, since it allows the verification of the pathology, whenever it is well indicated.
After a detailed clinical examination, complementary tests were performed, such as panoramic radiography and computed tomography. However, the diagnosis of osteosarcoma was only possible with the histopathological exam based on the lesion biopsy. The patient was immediately referred for treatment with the oncologist and the head and neck surgeon.
Thus, it is essential to manage a multidisciplinary team, enabling the screening and monitoring of possible patients who are candidates for the development of osteosarcoma, so that diagnosis is given early and the prognosis can be better.
References
- Cassone AE , Barbi-Gonçalves JC, Silva AAM, et al. (1998) Tratamento multidisciplinar do osteossarcoma. Revista Brasileira de Ortopedia 33: 835-840.
- Chabner Ba, Longo DL (2015) Manual de Oncologia de Harrison. (2nd edn), Porto Alegre: Artmed.
- Pedruzzi PAG, Costa PB, De Oliveira BV, et al. (2006) Osteossarcoma da cabeça e pescoço. Revista Brasileira de Cirurgia de Cabeça e Pescoço 35: 255-259.
- Fletcher CDM, Bridge JA, Hogendoorn PCW, et al. (2013) World health organization classification tumours of soft tissue and bone. World Health Organization Classification of Tumours, (4th edn), Lyon: IARC Press.
- Neville BW, Damm DD, Allen CM, et al. (2016) Patologia oral & maxilofacial. (4th edn), Rio de Janeiro: Elsevier.
- De Lukschal LF, Barbosa RMLB, Alvarenga RL, et al. (2013) Osteossarcoma em maxila: Relato de caso. Rev Port Estomatol Med Dent Cir Maxilofac 54: 48-52.
- El-Naggar AK, Chan JKC, Grandis Jr, et al. (2017) World health organization classification of head and neck tumours. World health organization classification of tumours, (4th edn).
- Shao Z, He Y, Wang L, et al. (2010) Computed tomography findings in radiation-induced osteosarcoma of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109: 88-94.
- Chabchoub I, Gharbi O, Remadi S, et al. (2009) Postirradiation osteosarcoma of the maxilla: a case report and current review of literature. J Oncol 2009: 876138.
- Madrigal FM, Godoy LMR, Daboin KP, et al. (2002) Laryngeal osteosarcoma: A clinicpathologic analysis of four cases and comparison with a carcinosarcoma. Ann Diagn Pathol 6: 1-9.
Corresponding Author
Luisa Aguirre Buexm, Department of General Pathology and Pathological Anatomy, Medicine School, Faculdade de Medicina de Campos, Campos dos Goytacazes, Brazil.
Copyright
© 2020 Feriani GG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.