A Case Report of Juvenile Aggressive Fibromatosis of the Lower Jaw in an 8-Year-Old Male
Abstract
Aggressive fibromatosis is a rare, localized, and aggressive intra-bony soft tissue tumor of spindle cells with a high tendency to recur if not treated properly. Here we report on a case of juvenile aggressive fibromatosis in an 8-years-old Male who presented with 3 weeks' history of a mass in the mandible associated with loose teeth due to alveolar and cortical bones resorption. Bundles of oval cells with fibro-collagenous connective tissue were shown microscopically. After eight months of follow up, no evidence of recurrence was found following conservative surgery to preserve the permanent teeth.
Keywords
Juvenile fibromatosis, Aggressive fibromatosis, Desmoplastic fibromatosis
Introduction
Aggressive fibromatosis arises from musculoaponeurotic structures and is locally aggressive and invasive, showing high recurrence after local resection without metastatic spread, it is presentation similar to fibro sarcoma that why it is called grade 1 fibrosarcoma, and it is also known as desmoplastic fibromatosis [1-3]. Although it is rare in head and neck, it mainly occurs in children under 8-years-old [4]. Histopathological, aggressive fibromatosis exhibits well-differentiated fibroblastic proliferation and collagen production. Radical surgical resection with wide margins is usually the treatment of choice, and patients are usually followed up for up to 3 years if margins are negative. In rare cases, the tumor regresses spontaneously [5].
Case Review
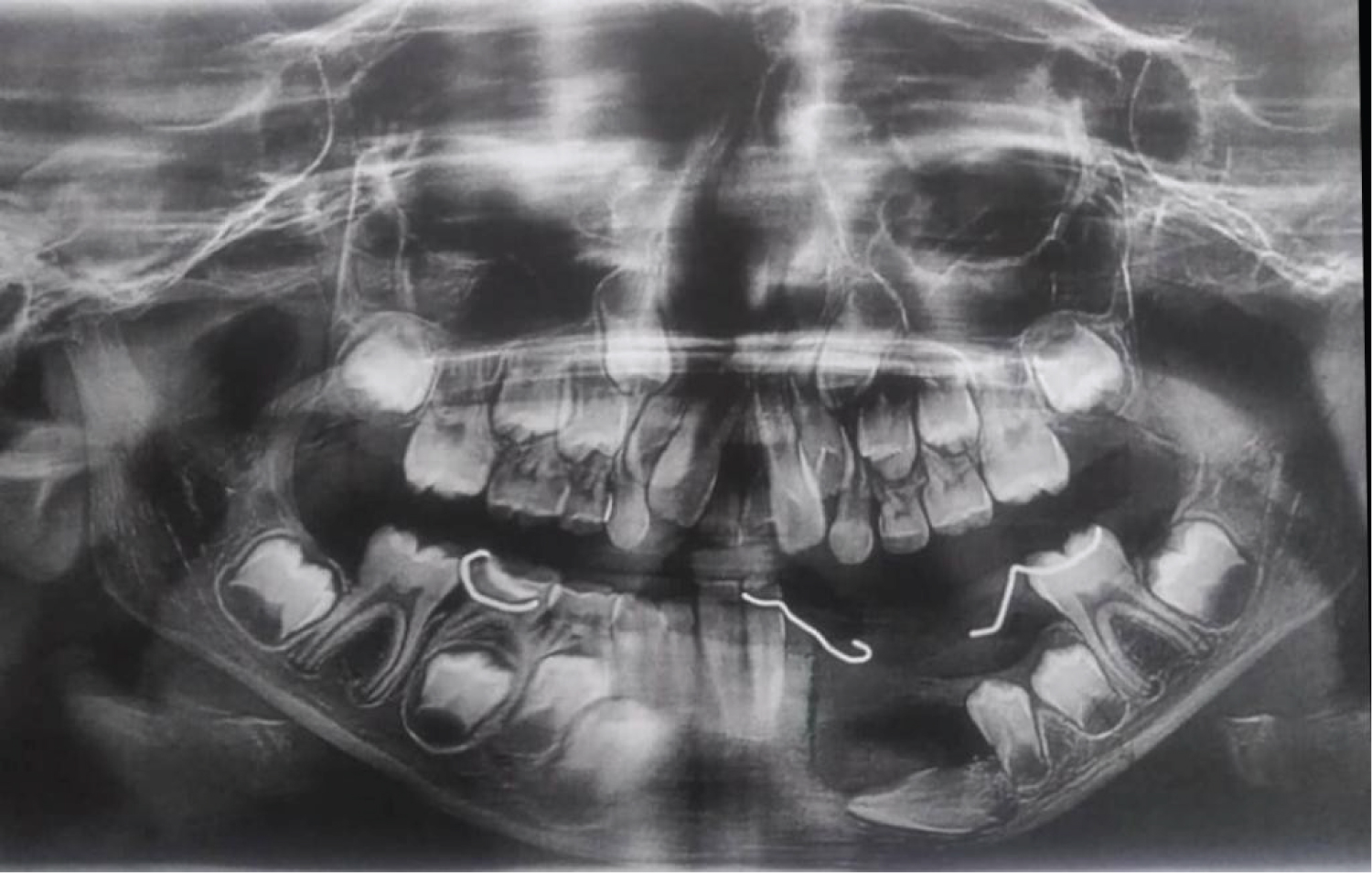
An 8-year-old African descent boy presented to the department of oral and maxillofacial surgery at Sharque Alnil Hospital complaining of swelling and lost teeth on the left side of the lower jaw for three weeks. No history of pain fever, loss of weight or night sweats. On examination, the face was symmetrical and no palpable lymph nodes. Intraorally, expansion of buccal and lingual cortices was seen on the left side of the lower jaw at the area of A, B, C, D, and E deciduous teeth with grade 2 motilities of A, B, C and D teeth and loss of tooth number D. no occlusal interference, no ulceration on the overlying mucosa. On the radiographic image (Figure 1 and Figure 2) Ill-defined radiolucency in the lower left side of the jaw extending from the first deciduous incisor to the second deciduous molar was evidence, permanent successors were within the tumor and were pushed downward and the lower border of the mandible was intact. In differential diagnosis, dentigerous or periapical cysts were thought. A biopsy was taken which microscopically showed interlacing bundles of oval cells with adjoining fibro-collagenous connective tissues and reactive bone trabeculae with no epithelial lining or granuloma or malignancy and that is revealed a benign spindle cell lesion. Further immunohistochemistry was recommended for verification and rule out of other possibilities and results were negative for desman, SMA, CD68, CD34 and S100, and results consistent with fibromatosis. After having to discuss the treatment plan with parents, the treatment plan was formulated. In order to preserve the permanent teeth, the young patient underwent conservative surgical curettage and extraction of loose deciduous teeth. A prosthesis was constructed to replace the extracted teeth and to cover the bony defect and the patient was subjected to periodic follow-up clinically and radio graphically. After 8 months postoperatively, the panoramic image did not show any evidence of recurrence. Moreover, the permanent teeth in the area of the surgery appeared to erupt uneventfully except the left lower canine (Figure 3). The patient is and closely observed to assure no recurrence and normal eruption of the permanent teeth.
Discussion
Fibromatosis is a benign tumor, but it is presented as aggressive, and it is etiology and pathogenesis are unclear yet. As noted earlier, fibromatosis has been classified into two types, superficial and deep. The deep type can then be further classified into abdominal or extra-abdominal fibromatosis [6]. Similar to our patient; juvenile fibromatosis is more common in patients under 8 years of age [4]. The reported average age is 9 years (range 8 months to 63 years), 62% of head and neck cases occurred between 5 and 15-years-old, and 21% occurred under 5-years-old. The literature also showed a trend of male preference [7].
Although association of aggressive fibromatosis and Gardner syndrome and familial adenomatous polyposis has been postulated in literature, our case occurred as sporadic condition [8]. The deep variant of fibromatosis which is the most common in the head and neck, occurs in the mandible more common especially in the posterior region specifically the ramous and the angle [9] and similar to this occurrence the presented case had a Mandibular lesion but it occurred in a more anterior region involving the left anterior mandible and part of the left body.
Plain image of the affected bone shows well-defined radiolucent lesion which appears as unilocular or multilocular with partially sharp or diffuse border without sclerotic margins [10] which is in agree with our findings that exhibits a unilocular radiolucent lesion with ill-defined diffuse margins on the panoramic view, while the 3 D Con beam CT scan showed an obvious buccal and lingual cortexes defects. Floating teeth without alveolar bone support associated with root resorption is a common finding that agrees with our case. For precise assessment of the tumor which is mainly soft tissue, it is better to order MRI, to see the exact expansion of the tumor and it is also suitable for surgical planning [11].
Radiographic differential diagnosis of aggressive fibromatosis includes multiple pathological entities which involve ameloblastoma, odontogenic fibroma, aneury small bone cyst, hemangioma, fibrosarcoma, and malignant histocytoma [12], due to these varieties we perfumed the excision biopsy which revealed the classical findings of extrabdominal and desmoid fibromatosis showing, proliferating fibroblast with little mitotic activity of oval cells in fibrocollagenous stromal, the term fibromatosis is indicating well-differentiated fibroblasts and my fibroblasts that develop in the soft tissue [1]. To confirm the diagnosis some studies adopted the concept of using B-catenin marker which is found to be positive in 90% of the histopathological specimen of the cases of fibromatosis. In our case we requested immunohistochemistry for verification and rule out of other possibilities and results were negative for desman, SMA, CD68, CD34, S100 and results consistent with fibromatosis, Those with aggressive fibromatosis usually undergo resection of the lesion with a free margin if it does not cause any impairment or morbidity, but if it causes any impairment or morbidity then the best treatment is curettage plus chemotherapy for patients under 18 years of age, and radiotherapy for above 18-years-old patient [13]. In the event of recurrence, some authors suggested undergoing 'segmental resection or additional curettage and peripheral osteotomy [14]. We decided to use curettage as a conservative approach in this case due to the young age of the patient and to preserve the permanent successor teeth and allow them to fully erupt. Therefore, we decided not to use adjuvant chemotherapy and instead to follow the patient meticulously.
A panoramic image taken eight months postoperatively revealed remarkable bone lay down and an improvement in the line of eruption for the two left lower premolars, however the left lower canine did not gain its proper path and we decided to extract it after confirming the control of the lesion.
Conclusion
Aggressive fibromatosis is a rare, localized and aggressive intra bony tumor that frequently affects young patients and presents as a painless mass that can cause facial disfigurement. Although some authors suggested the free margin resection of the lesion and adjuvant chemo or radiotherapy, we present here a case who treated by surgical curettage and flow up and after 8 months of operation no evidence of recurrence was seen.
Acknowledgement
Many thanks and deep gratitude to my supervisor for his guidance and encouragement to bring this work.
References
- Angiero F, Benedicenti S, Stefan M (2008) Fibromatosis of the head and neck: Morphological, immune histochemical and clinical features. Anticancer Res 28: 1725-3172.
- Shah S V, Girhe V J, Akole R A, et al. (2013) Well differentiated nonmetastasizing fibro sarcoma (aggressive fibromatosis) of mandible: A rare case report and a literature review. Oral Surg Oral Med Oral Pathol Oral Radiol 116: e98-e102.
- Neville BW, Damm DD, Allen CM, et al. (2009) Soft tissue tumors: In: Oral and Maxillofacial Pathology. (3rd edn), Reed Elsevier India Pvt.Ltd, 507-551.
- Kingston C A, Owens C M, Jeanes A, et al. (2002) Imaging of desmoid fibromatosis in pediatric patients. AJR Am J Roentgenol 178: 191-199.
- Bridge J A, Swarts S J, Buresh C, et al. (1999) Trisomies 8 and 20 charac- terize a subgroup of benign fibrous lesions arising in both soft tissue and bone. Am J Pathol 154: 729-733.
- Fowler CB, Hartman KS, Brannon RB (1994) Fibromatosis of the oral and Para oral region. Oral Surg Oral Med Oral Pathol 77: 373-386.
- Seper L, Burger H, Vormoor J, et al. (2005) Aggressive fibromatosis involving the mandible-case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99: 30-38.
- Hizawa K, Iida M, Mibu R, et al. (1997) Desmoid tumors in familial adenomatous polyposis/Gardner's syndrome. J Clin Gastroenterol 25: 334-337.
- Pena S, Brickman T, St Hilaire H, et al. (2014) Aggressive fibromatosis of the head and neck in the pediatric population. Int J Pediatr Otorhinolaryngol 78: 1-4.
- Fisker AV, Philipsen HP (1976) Desmoplastic fibroma of the jaw bones. Int J Oral Surg 5: 285-291.
- Bohm P, Krober S, Greschniok A, et al. (1996) Desmo- plastic fibroma of the bone. A report of two patients, review of the literature, and therapeutic implications. Cancer 78: 1011-1023.
- Inwards CY, Unni KK, Beabout JW, et al. (1991) Desmoplastic fibroma of bone. Cancer 68: 1978-1983.
- Wang W, Koirala U, Ma S, et al. (2014) Age-based treatment of aggressive fibromatosis in the head and neck region. J Oral Maxillofac Surg 72: 311-321.
- Tandon S, Garg RK (2012) Intraoral desmoplastic fibroma: A manifestation of tuberous sclerosis. Fetal Pediatr Pathol 31: 195-201.
Corresponding Author
Abdel Nasir Gafar Ahmad, Associate Professor and Consultant, Department of Oral and Maxillofacial Surgery Consultant, International University of Africa, Sudan.
Copyright
© 2021 Ahmed ME, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.