Prevalence of Ultrasound Biomicroscopic Features in a Select Group of Recurrent Angle Closure Subjects
Keywords
Ultrasound biomicroscopy, Ciliary block, Angle closure
In most cases of angle closure, there is an element of pupil block, and Neodymium-doped ytrrium aluminium garnet (ND:YAG) peripheral laser iridotomy is commonly performed as first line treatment with phacoemulsification as an alternative [1]. However, both these procedures are not always curative and patients may relapse into angle closure. Therefore, monitoring of angles post-treatment is recommended [2].
Recurrence of angle closure following peripheral iridotomy or cataract surgery can be caused by plateau iris syndrome, lens disproportion or ciliary block [2]. In this group of patients, high rates of anatomical abnormalities between the ciliary body and lens can be found. These include reduced cilio-lenticular gap, ciliary body-lens apposition, irido-ciliary cysts and Soemmering's ring [2].
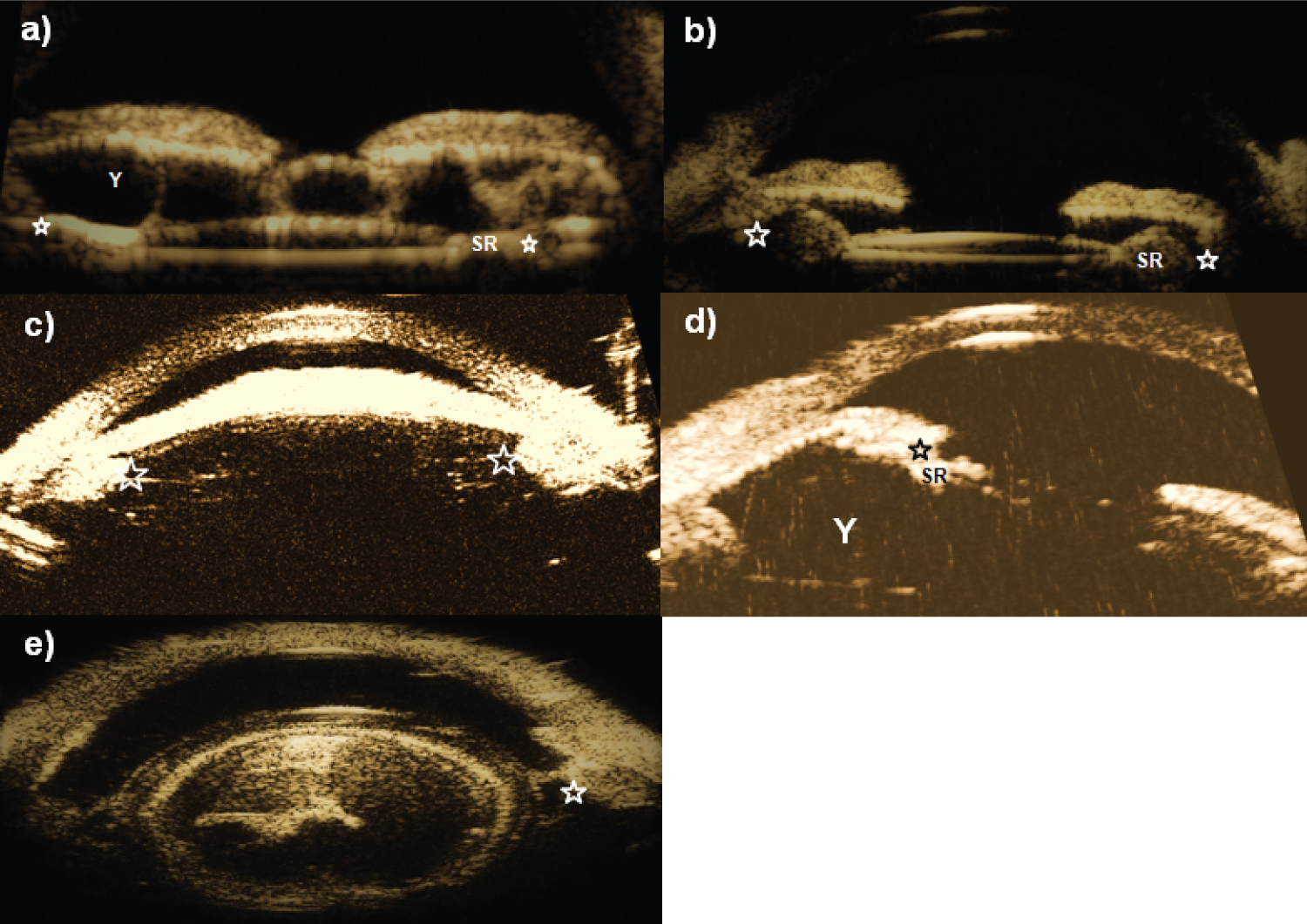
Lenticular-ciliary body apposition can lead to increased hydraulic resistance of aqueous humour passing from the vitreal space to the posterior chamber with an increase pressure differential leading to ciliary block [1,2]. The 'volcano sign' can be an early indication on examination for this condition [2]. Irido-ciliary cysts can push the peripheral iris towards the trabecular meshwork anteriorly and ciliary body towards the lens equator [2]. Soemmering's ring can stretch the lens capsule and appose the ciliary body. Ultrasound biomicroscopy (UBM) is a useful tool to identify the above mentioned less distinct anterior segment entities causing angle closure and guide future therapy options [2-5].
In this retrospective case series, we analysed UBM scans to measure the prevalence of abnormal anterior segment features in a select group of patients with recurrent angle closure. These patients had all undergone laser peripheral iridotomy for prior primary angle closure. The angle was considered closed when posterior trabecular meshwork could not be seen on gonioscopy. An immersion UBM scan was performed on patients presumed to have a component of ciliary block with a 'volcano sign' on examination. Images were analysed for ciliary body-lens apposition, irido-ciliary cysts and Soemmering's ring. Scans were obtained with an EyeCubed® (Ellex Medical Pty Ltd. E&OE. PB0012H, Adelaide, Australia) UBM scanner attached with a 40Mhx transducer.
A total of 59 eye scans from 38 patients were retrieved, with age ranging from 19 to 83 years (mean: 67.4 years). The scans were performed over a period of 5.5 years. Four distorted unclear scans were excluded. In our sample of 55 UBM scans, 35% were from pseudophakic and 65% were phakic eyes. Amongst the phakic eyes, 83% had cilio-lenticular contact, with 40% of these containing ciliary body cysts. Of the pseudophakic eyes, 84% had cilio-lenticular contact with large Soemmering's ring, with 4% of those having ciliary body cysts as well. Overall, ciliary body cysts were present in 33% of eyes. 16% of all eyes had no cilio-lenticular contact with 67% of them phakic and 33% pseudophakic. One patient with cilio-lenticular contact had microspherophakia. Complete results shown in Table 1. Anterior segment features shown in Figure 1.
Ultrasound biomicroscopy was useful to guide future therapy options, mainly surgical, and to identify anterior segment features in our group of subjects who relapsed into angle closure after having laser peripheral iridotomy. If the scan detected significant ciliary block (lenticular-ciliary body apposition), lens extraction surgery was considered as the next treatment option. In our sample of patients with cilio-lenticular contact, ciliary body cysts in phakic patients and Soemmering's ring in pseudophakic eyes are a prominent finding. Predisposing features to recurring angle closure were apposition between the ciliary body and lens equator or Soemmering's ring. Ciliary body cysts cause a mass effect, predisposing towards cilio-lenticular contact and directly pushing the iris anteriorly. In this study, Soemmering's ring were more common than previous reports, causing ciliary block in primary angle closure [1,2].
Conflicts of Interest
No conflicts of interest.
Funding
No funding was received.
References
- Kremer FZ, Chadha N, Tania Tai TY, et al. (2017) Secondary Angle Closure: Imaging, Diagnosis, Etiology, and Treatment. Adv Ophthalmol Optom 2: 301-319.
- Ng WT, Morgan W (2012) Mechanisms and treatment of primary angle closure: A review. Clin Exp Ophthalmol 40: e218-e28.
- Choy BNK, Chan JCH, Chien CPY, et al. (2016) Recurrent acute angle-closure attack due to plateau iris syndrome after cataract extraction with or without argon laser peripheral iridoplasty: A case report. BMC ophthalmology 16: 64.
- Dada T, Gadia R, Sharma A, et al. (2011) Ultrasound biomicroscopy in glaucoma. Surv Ophthalmol 56: 433-450.
- Mannino G, Abdolrahimzadeh B, Calafiore S, et al. (2016) A review of the role of ultrasound biomicroscopy in glaucoma associated with rare diseases of the anterior segment. Clin Ophthalmol 10: 1453-1459.
Corresponding Author
Sugapriyan Ravichandran, BMBS, Centre for Ophthalmology and Visual Science (incorporating Lions Eye Institute) 2, Verdun Street, Nedlands, Perth WA 6009, Western Australia, Australia, Tel: +64223332611.
Copyright
© 2021 Ravichandran S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.