The 4-Snip Ampullotomy: A New Surgical Technique for Managing Acquired Punctal Stenosis
Abstract
Background/objectives: To report on a new technique for treating acquired punctal stenosis in the outpatient clinic setting. We present outcomes from a case series of 25 eyes who underwent a 4-snip ampullotomy procedure (4 cuts to the lacrimal papilla-ampulla junction) to widen the lacrimal punctum.
Subjects/methods: Retrospective case note review was completed for all eyes undergoing the new 4-snip ampullotomy procedure from September 2014 - February 2017. Anatomical success was defined as patency of the lacrimal punctum on slit-lamp biomicroscopy with ability to pass a 27-gauge cannula at follow-up and functional success on symptomatic improvement as reported by the patient. A patient-based subjective questionnaire on symptom improvement and procedural experience was posted to each patient anonymously.
Results: 25 eyes were included from 18 individuals. There was an anatomical success rate of 96% and functional success rate of 83%. Follow-up to discharge ranged from 2-12 months. Median average cohort age was 63, range 26-81 years. A quarter of patients also suffered from blepharitis ± meibomian gland dysfunction. There were no reported complications. Patient survey revealed the procedure was well-tolerated by the majority of patients.
Conclusions: The 4-snip ampullotomy procedure provides a safe, quick and efficacious treatment for punctual stenosis. Success rates are comparable to those published in the literature for the 3-snip punctoplasty. This procedure could increase the capacity of oculoplastic surgical lists and reduce the surgical waiting-list times as it may be performed in the outpatients' setting.
Introduction
Punctal stenosis is defined as the inability to pass a 26-gauge lacrimal cannula into the punctum prior to punctal dilatation [1]. The one-snip punctoplasty, initially described in 1853 by Bowman, has now been superseded by variations on a three- or four-snip punctoplasty, owing to its superior outcomes [1-7]. All of the techniques remove a section of the proximal lacrimal apparatus, often including part of the horizontal canaliculus, resulting in irreversible changes the normal physiological architecture and altered function of complex active and passive processes required for lacrimal drainage. A minimally invasive approach for treating acquired punctual stenosis would be an ideal situation [7]. We report outcomes for a new tissue-preserving technique: The 4-snip ampullotomy (4 diagonal cuts to the lacrimal papilla-ampulla junction) to widen the lacrimal punctum. Outcomes of the 4-snip ampullotomy are compared with the three-snip punctoplasty (rectangular and triangular).
Materials and Methods
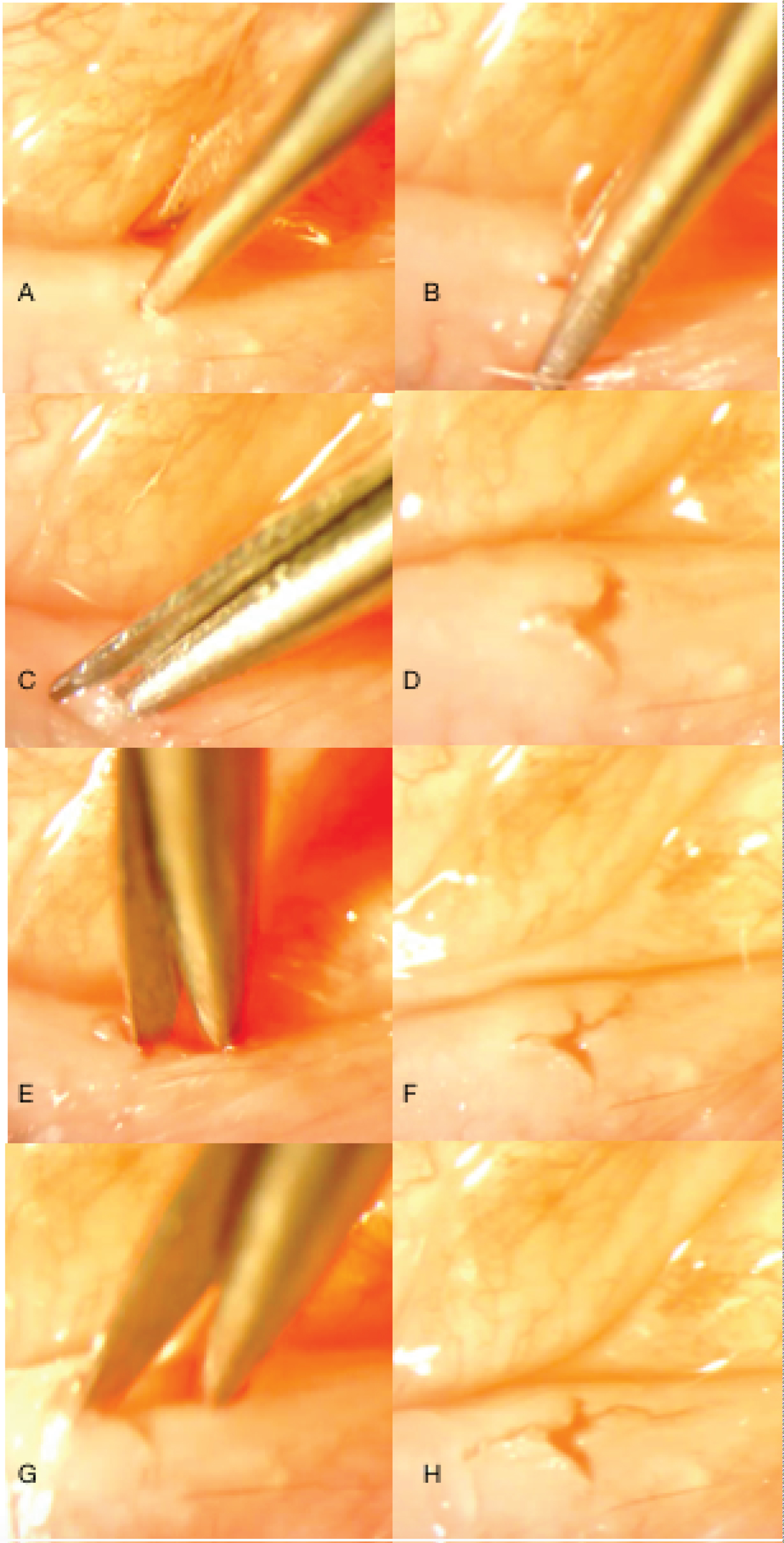
Retrospective case note review was completed for all eyes having undergone the 4-snip ampullotomy between September 2014 to September 2017. Full written consent was obtained from the patient prior to the procedure. The procedure was completed in outpatient clinic at the time of lacrimal syringing. On identification of punctual stenosis, the punctum was dilated to allow for passage of a 26-gauge lacrimal cannula and to determine patency of the nasolacrimal duct with a sodium chloride 0.5% flush. Topical G. proxymetacaine 0.5% preservative free was instilled into the lower fornix and over the lacrimal punctum. Vannas scissors with a 3 mm cutting edge were used to make 4 diagonal cuts to the lacrimal papilla-ampulla junction (Figure 1). Separation of the cut edges was achieved by gently opening the tips of the Vannas scissors whilst in the punctum.
Anatomical success was defined as patency of the lacrimal punctum on slit-lamp biomicroscopy and the ability to pass a 26-gauge lacrimal cannula at follow-up. Functional success describes symptomatic improvement as reported by the patient during the follow-up period. An optional follow-up questionnaire was posted with a stamped addressed return envelope to each patient to determine tolerability of procedure. If the questionnaire was not returned, a telephone call asking question 3 on procedure tolerability was completed. This study adhered to the ethical standards set out by the Declaration of Helsinki, 2013 and approval from the local Research, Innovation and Development (RID) institutional review board was obtained.
Results
In total, 25 eyes from 18 patients were included (Table 1 and Table 2). Follow-up to discharge ranged from 2-12 months. None of the discharged patients re-presented to outpatients clinic with a watery eye.
One patient underwent a formal rectangular 3-snip punctoplasty owing to a fine membrane having formed over the punctum at 3 months post-procedure, without re-apposition of the edges of the punctum. 4 patients reported no improvement to epiphora, all of whom were being treated for ocular surface disease such as blepharitis, dry eye disease and meibomian gland dysfunction. 10 of 18 patients returned the questionnaire which showed the procedure was well-tolerated by the majority of patients. The remaining 8 patients who did not return the questionnaire received a telephone consultation. 8 of 8 patients could not recall having had the procedure in clinic and therefore did not return the survey (Table 2).
Discussion
Functional and anatomical success rates of the 4-snip ampullotomy are comparable to those published in the literature, (Table 3) [1,5,7]. We have additionally demonstrated the 4-snip ampullotomy is well-tolerated through qualitative post-procedure survey.
Numerous studies have indicated the importance of preserving the structural integrity of the canaliculus for effective physiological tear drainage, in particular preservation of the 'lacrimal pump' [8,9]. The 4-snip ampullotomy, which we describe here, fulfils this requirement. It the first to be reported that involves no removal of tissue, maintains the physiological architecture of the punctum, ampulla and canaliculus.
Exploration of the mechanisms employed in lacrimal tear drainage, highlights the importance of preserving the physiological architecture of the lacrimal tear drainage system. For instance, tear drainage through the lacrimal system is facilitated by passive and active components [9]. The passive components are gravity, capillary action forces, absorption and evaporation from the ocular surface. The active 'lacrimal pump' mechanism remains incompletely defined. One theory is that structural changes to the elastic muscular lacrimal drainage apparatus induced by the action of blinking form a key aspect of the active phase of tear drainage: the 'lacrimal pump' [10,11].
How does our study compare to other studies? Our study design mitigated complete data capture and minimised exclusion biases. Caesar, et al. excluded over half of the initial sample of patients owing to a strict eligibility study criteria that included additional surgery, electing for non-surgical management, unavailability of notes, notes without a comment on success. This may have resulted in biases and furthermore could be one of the reasons for the disparity between our functional success rate of 83.3% compared to 92% [1].
The absence of improvement to epiphora in 4 individuals from our cohort may be explained by the presence of concurrent eyelid and ocular surface disease. Kashkouli, et al. reported on factors associated with acquired punctual stenosis and found over 45% of eyes with punctual stenosis also exhibited signs of chronic blepharitis [4]. Therefore, the suggestion is that inflammatory eyelid disease may be a cause of punctual stenosis, however it is likely to also perpetuate epiphora symptoms depending on severity of the disease. Alternatively, Ali, et al. reported functional epiphora in 10.3% of their cohort. However 4 of 9 individuals classified as functional epiphora also had existing lid laxity which may have contributed to poor punctal apposition to the globe and ineffective passive processes required for lacrimal drainage.
Conclusion
The ampullotomy can be considered a first-line procedure for management of punctal stenosis. Because it is significantly less destructive than alternative surgical approaches, it preserves the complex lacrimal pump mechanism essential for physiological tear drainage. Importantly, there were no complications encountered in this observed cohort which had no excluded cases. Common side-effects from subcutaneous infiltrated local anaesthesia such as bruising, pain, bleeding and hypersensitivity are avoided.
This novel procedure has potential to reduce surgical waiting lists times for oculoplastic procedures and provide immediate intervention for individuals with acquired punctual stenosis. It is of particular advantage to individuals with multiple co-morbidities who may have difficulty attending multiple appointments.
Acknowledgements
None.
Conflict of Interest
There are no financial declarations for either authors and no conflicts of interest for both authors.
Funding
No financial support was received for this project.
Precis
The ampullotomy is a safe, efficacious, tissue-preserving, outpatient procedure for acquired punctual stenosis with comparative success rates to the 3-snip rectangular and triangular punctoplasty.
References
- Caesar RH, McNab AA (2005) A brief history of punctoplasty: The 3-snip revisited. Eye 19: 16-18.
- Graves B (1926) Making a new lacrimal punctum. Am J Ophthalmol 9: 675-677.
- Thomas JBT (1951) A modification to Graves' operation for epiphoria due to stenosis of the lacrimal punctum. Br J Ophthalmol 35: 306.
- Kashkouli M, Beigi B, Astbury N (2005) Acuired external punctual stenosis: Surgical management and long-term follow-up. Orbit 24: 73-78.
- Chak M, Irvine F (2009) Rectangular 3-snip punctoplasty outcomes: Preservation of the lacrimal pump in punctoplasty surgery. Ophthalmic Plast Reconstr Surg 25: 134-135.
- Kim SE, Lee SY, Yoon JS (2012) Outcomes of 4-snip punctoplasty for severe punctual stenosis: Measurement of tear meniscus height with optical coherence tomography. Am J Ophthalmol 153: 769-773.
- Ali MJ, Ayyar A, Naik MN (2015) Outcomes of rectangular 3-snip punctoplasty in acquired punctual stenosis: Is there a need to be minimally invasive? Eye 29: 515-518.
- Lee MJ, Kyung HS, Han MH, et al. (2011) Evaluation of lacrimal tear drinagae mechanism using dynamic fluoroscopic dacryocystography. Ophthal Plast Reconstr Surg 27: 167-177.
- Detorakis E, Zissimopoulos A, Ioannakis K, et al. (2014) Lacrimal outflow mechanisms and the role of scintigraphy: Current trends.World J Nucl Med 13: 16-21.
- Kakizaki H, Zato M, Miyaishi O, et al. (2005) The lacrimal canaliculus and sac bordered by the Horner's muscle form the functional lacrimal drinage system. Ophthalmology 112: 710-716.
- Doane MG (1981) Blinking and the mechanics of the lacrimal drainage system. Ophthalmology 88: 844-851.
Corresponding Author
Selina Khan, MB ChB, BSc(Hons.), Bristol Eye Hospital, Lower Maudeli Street, Bristol. BS1 2LX, UK.
Copyright
© 2021 Khan S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.