Evaluation of the Equality of Medial Rectus Advancement to Medial Rectus Resection for Consecutive Exotropia
Abstract
Objective: To analyse the amount of medial rectus advancement in the treatment of consecutive exotropia by comparing with the amount of medial rectus resection in a sample of patients with constant exotropia and evaluate the effectiveness of medial rectus advancement with lateral rectus recession in the management of consecutive exotropia.
Materials and Methods: A retrospective chart review of patients who underwent unilateral medial rectus strengthening with lateral rectus weakening due to consecutive or constant exotropia was performed. Patients with consecutive exotropia underwent medial rectus advancement with lateral rectus recession and patients with constant exotropia underwent medial rectus resection with lateral rectus recession. Surgical dosages were determined according to a standard table. Successful result was defined as an alignment within 10 prism diopters of orthotropia.
Results: A total of 36 patients fulfilled the inclusion criteria, 18 had consecutive exotropia and 18 had constant exotropia. Successful alignment was obtained in 83.3% of the patients with consecutive exotropia and 88.9% of the patients with constant exotropia. There was no difference between the amount of medial rectus advancement performed in consecutive exotropia patients and the amount of medial rectus resection performed in constant exotropia patients (P = 0.38). Postoperatively, while consecutive exotropes with a poor result showed overcorrection, constant exotropes with a poor result showed under correction.
Conclusion: This study suggested that there is no difference between the amount of previously recessed medial rectus advancement and the amount of untouched medial rectus resection. Also, it showed that medial rectus advancement with lateral rectus recession is an effective means for correcting secondary exotropia.
Keywords
Advancement, Lateral, Medial, Recession, Rectus
Introduction
Consecutive exotropia is an outward ocular deviation that appears either spontaneously or after surgical or optical treatment in a previously esotropic patient [1,2]. The reported prevalence rates are between 2% and 29% [3,4]. The probable risk factors for consecutive exotropia are multiple previous surgeries, excessive bimedial recessions, postoperative limited adduction, amblyopia, high hyperopia, A or V pattern, dissociated vertical deviation, poor binocularity, nystagmus and growth retardation [5-9].
Although many surgical procedures have been described for surgical treatment of consecutive exotropia, there is still no consensus on the best surgical procedure. Surgical options include bilateral lateral rectus recession, bilateral medial rectus advancement, medial rectus advancement with or without lateral rectus recession, unilateral lateral rectus recession and medial rectus resection with or without advancement, and medial rectus advancement alone or combined with resection or lateral rectus recession [9-13].
The surgical dosage of medial rectus advancement for correcting consecutive exotropia is not available in standard surgical dosing tables. In most of the previous studies which performed medial rectus advancement for treating consecutive exotropia, the amount of medial rectus advancement was assumed to be equivalent to the amount of this muscle resection advised from standard tables for that angle of deviation. The aim of the current study is to verify this assumption by performing a comparison between the amount of previously recessed medial rectus advancement and the amount of untouched medial rectus resection and to evaluate the effectiveness of unilateral medial rectus advancement with lateral rectus recession in the surgical management of consecutive exotropia.
Materials and Methods
The clinical records of patients who underwent unilateral surgery due to consecutive or constant exotropia during the period from 2011 to 2018 were reviewed retrospectively. A written informed consent form had been obtained from all of the patients or the parents of children before the surgery. Institutional review board approval was obtained for the procedures used in this study and the rules of Helsinki Declaration were followed at every stage of the study. Patients with inferior oblique muscle overaction, dissociated vertical deviation, corneal and lens pathologies preventing posterior segment examination, retinal pathologies, a history of ocular trauma and systemic or neurological diseases were excluded from the study. In addition, patients with a follow-up time less than 6 months were not included in the study. The consecutive exotropia was defined as an exodeviation of 10 PD (prism diopters) or more in the primary position at near (1/3 meter) and distance (6 meters) with appropriate refractive correction in patients who had esotropia surgery. The constant exotropia was defined as an exodeviation with a constant angle in different directions of gaze at both near and distance fixation.
All patients underwent a detailed ocular examination including cycloplegic refraction, best spectacle-corrected visual acuity by the Snellen chart, careful observations with a slit-lamp microscope, dilated fundus evaluation, ocular motility and measurements of the ocular misalignment at near and distance by the alternate prism cover test. All patients were examined preoperatively, 1 day and 1 month postoperatively, and at the last visit. The following data were collected: gender, age at the time of diagnosis, age at the time of the exotropia surgery, refractive error, the results of visual acuity testing, presence of ambliyopia and pattern strabismus, detection of adduction deficiency, the angles of deviation at preoperative and postoperative examinations, the amount of lateral rectus muscle recession, the amount of improvement in exotropia and the follow-up time.
Patients with consecutive exotropia underwent medial rectus advancement with lateral rectus recession surgery. In these patients, the amount of lateral rectus recession was determined based on the amount of medial rectus advancement and degree of preoperative exodeviation by using a standard surgical dosing table developed by Santiago and Rosenbaum [14], and also adjusted based on our clinical experience. In patients with constant exotropia, the amount of both medial rectus resection and lateral rectus recession was determined on the basis of preoperative exodeviation's angle by using the same table. All of the surgeries were performed under general anesthesia by a single surgeon on the non-fixing eyes of participants. Successful outcome was defined as a distance ocular alignment within 10 PD of orthotropia at 6 months postoperatively.
Medial rectus muscle advancement: In the patients with consecutive exotropia, initially a limbal conjunctival incision was made in the nasal quadrant to expose the nasal aspect of the sclera. After a careful dissection, the previously recessed medial rectus muscle was separated from surrounding connective tissue and postsurgical adhesions. The muscle was then isolated with a muscle hook. The original insertion location of the medial rectus muscle was assumed as a point 5.5 mm behind the limbus and measured with a curved scleral ruler. Later, the muscle was detached from the sclera, advanced to the original insertion site, and sutured to the sclera with a 6-0 double-armed Vicryl suture (Ethicon, Inc.,Somerville, NJ, USA). Finally, the conjunctival wound was closed using interrupted 8-0 polyglactin sutures.
Statistical analysis: SSPS for Windows statistical software (ver. 22.0; IBM Corp., Armonk, NY, USA) was used for the analysis. The results are expressed as means ± standard deviation (SD) or median (min-max). Shapiro-Wilk test was used to determine the consistency of continuous variables to normal distribution. In order to investigate the differences between the two groups, Mann-Whitney U test was used for quantitative data, and Chi-Square test was used for the qualitative data. A value of P < 0.05 was considered statistically significant.
Results
The records of 39 patients were reviewed. Of these, 2 patients were excluded because of an intervening of lateral rectus muscle at the initial surgery for esotropia and one patient because of the inability to participate in postoperative follow-up. Finally, a total of 36 patients were identified, 18 with consecutive exotropia and 18 with constant exotropia. All of the patients with consecutive exotropia had previously undergone bilateral medial rectus recessions for esotropia at the first surgery. None of the patients with consecutive exotropia had undergone more than one operation, and none of the patients with constant exotropia had undergone any operation before our corrective surgery. Amblyopia was found in 11 patients with consecutive exotropia and 8 patients with constant exotropia. V pattern was diagnosed in 2 patients with consecutive exotropia and 3 patients with constant exotropia. Four patients with consecutive exotropia had a limited adduction. The demografic and ocular examination findings, the mean amount of lateral rectus recession, the mean improvement of exotropia, and the mean follow-up time of the surgical groups are presented in (Table 1). Preoperative and postoperative exodeviation angles, and milimeters of surgery performed in the patients are listed in (Table 2).
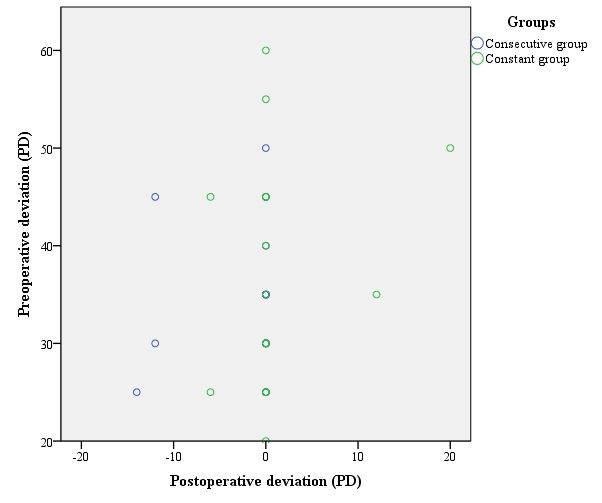
There was no statistically significant difference for gender distribution, age at the time of diagnosis, age at the time of exotropia surgery, visual acuity of the right and left eye, and the follow-up time between the two surgical groups (P = 0.31, P = 0.58, P = 0.84, P = 0.81, P = 0.37,P = 0,58, respectively). Also, no significant difference was determined in the preoperative and postoperative deviation, the amount of improvement in exotropia, and the amount of lateral rectus recession between our study groups (P = 0.52, P = 0.40, P = 0.92, P = 0.74, respectively). The scatterplot of preoperative and postoperative deviations in the surgical groups is shown in (Figure 1). We only found a significant difference for spherical equivalent in both the right eye and left eye (P = 0.019, P = 0.006, respectively).
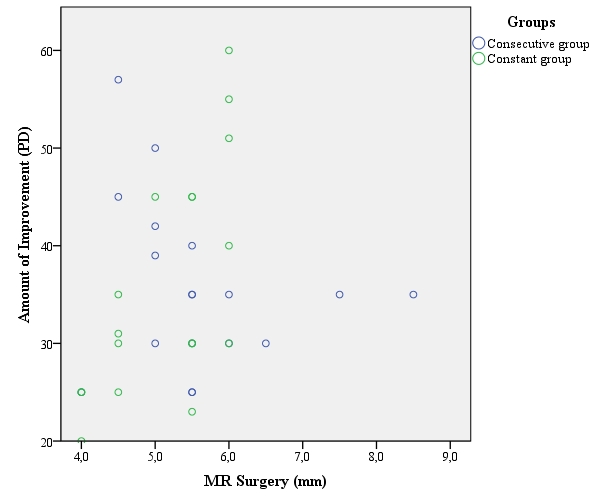
We performed a mean 5.58 ± 1.07 mm of medial rectus advancement in consecutive exotropic patient group and a mean 5.13 ± 0.76 mm of medial rectus resection in constant exotropic patient group. There was no statistically significant difference between the amount of medial rectus advancement performed in consecutive exotropia patients and the amount of medial rectus resection performed in constant exotropia patients (P = 0.38). (Figure 2) represents the scatterplot of improvement in the exodeviation resulting from medial rectus surgery performed in the two surgical groups.
In the consecutive group, surgical success was achieved in 15 of 18 patients (83.3%). In this group, 2 patients was diagnosed with an esotropia of 12 PD and one with 14 PD at 6 months postoperatively. In 13 of 18 patients with consecutive exotropia the insertion site of the medial rectus was found at a diatance of 11 mm or more behind the limbus at the time of surgery, in 5 patients at a distance less than 11 mm. In the constant group, surgical success was achieved in 16 of 18 patients (88.9%). Two patients had residual exotropia, the surgery was able to reduce exotropia from 50 to 20 PD in one patient and 35 to 12 PD in another. The patient with a residual exotropia of 20 PD required additional surgery.
Discussion
Several surgical procedures have been described for treatment of consecutive exotropia that is a challenging complication following esotropia surgery. A standard dose-effect relationship of horizontal muscles surgery has not been determined until now. To the best of our knowledge, all previous studies for correcting consecutive exotropia was performed in patients who previously underwent surgery. The present study evaluated the effectiveness of medial rectus advancement with lateral rectus recession for the correction of consecutive exotropia by comparing with medial rectus resection plus lateral rectus recession in constant exotropia patients who had no history of strabismus surgery.
Chang and Lin [11] performed unilateral medial rectus advancement with lateral rectus recession in 14 patients with consecutive exotropia following medial rectus recession and reported a success rate of 71.4%. They advanced the medial rectus to its original insertion point and recessed the lateral rectus according to a standard table based on the measured preoperative angle of deviation and intraoperative findings. They reported that combined surgery could be a more effective surgical approach in the surgical treatment of larger consecutive exotropia.
Donaldson et al. [15] performed medial rectus advancement and lateral rectus recession with additional adjustable sutures whenever indicated in 42 consecutive exotropia patients who had previously undergone esotropia surgery, and reported that this surgery is an effective procedure in the surgical management of consecutive exotropia with a success rate of 69%. In their study, the amount of advancement was presumed to be equal nearly to the amount of resection advised from a standard table for that degree of exodeviation.
Chatzistefanou et al. [16] advanced the previously recessed medial rectus muscle and recessed the previously resected lateral rectus muscle by an amount corresponding to a reversal of initial surgery in one eye of 52 consecutive exotropia patients who had formerly undergone surgery due to esotropia. They reported that a standard reversal of unilateral medial rectus recession and lateral rectus resection is an effcetive treatment for correcting consecutive exotropia with a success rate of 78.8%. In their study, the amount of advancement of the medial rectus was assumed to be equivalent to the amount of resection of this muscle advised from a standard table.
In a study on the nondominant eye of patients with consecutive exotropia performed by Mohan et al. [12], lateral rectus recession with medial rectus resection was performed in 17 patients, and lateral rectus recession and medial rectus partial resection combined with advancement was performed in 14 patients according to a standard surgical dosing table, and the success rate was reported to be 64.7% and 71.4%, respectively. They advanced the medial rectus only if the desired amount of resection of the muscle was not possible because of a very posterior medial rectus attachment to the sclera as the result of a former large recession for esotropia surgery. In their study, a 1 mm advancement of the medial rectus was considered to be equal to a 1 mm resection of the muscle in the correction of the exodeviation.
In a study conducted by Nabie et al. [10], 14 patients with consecutive exotropia following bilateral medial rectus recession were randomly selected for either bilateral medial rectus advancement or bilateral lateral rectus recession surgery, and an overall success rate was reported to be 78.5%. They determined the amount of muscles advancement or recession according to a standard table and presumed that every 1 mm of advancement is equal to 1 mm of resection.
In the current study, we obtained a success rate of 83.3% with medial rectus advancement and lateral rectus recession in patients with consecutive exotropia, and obtained a success rate of 88.9% with medial rectus resection and lateral rectus recession in patients with constant exotropia when an ocular alignment within 10 PD of orthotropia at the postoperative sixth month is considered a successful outcome. The surgical success for 6 months follow-up after the surgery for consecutive exotropia appears to be comparable to that after correction of constant exotropia. In the two surgical groups, the surgical dosage was determined according to a standard surgical table and a 1 mm of advancement of medial rectus was considered to be equivalent to a 1mm of resection of this muscle. Our success rate on the medial rectus advancement with lateral rectus recession in patients with consecutive exotropia was higher than those reported from above-mentioned studies [10-12,15,16]. We believe that the differences in the success rate are related to the nonhomogeneity of primary surgery for esotropia or corrective surgery for consecutive exotropia in each study, as well as the differences in using surgical dosing table in each study. Like our study, all these previous studies assumed that the amount of advancement of the medial rectus is equal to the amount of resection of this muscle. The present study was also planned to verify this assumption and so the amount of medial rectus advancement in patients with consecutive exotropia was compared with the amount of medial rectus resection in constant exotropia patients who had an untouched medial rectus, and no significant difference was determined (P = 0.38). The major strengths of the present study were to study on intact medial rectus muscles and make a comparison between the amount of intact medial rectus resection and the amount of previously recessed medial rectus advancement.
In our study, adduction deficiency was improved by medial rectus advancement in 4 consecutive exotropia patients who had preoperative adduction deficiency. Three consecutive exotropia patients were diagnosed with an esotropia after surgery, 2 patients had an esotropia of 12 PD and one patient 14 PD. It is unclear whether these overcorrections result from improper surgery or poor binocularity, which may result in more variability in the predicted results of a surgical plan. The fact that unpredictability of a surgical dose-response remains a serious problem, especially in reoperations. Contrary to what we thought, in patients with overcorrection, the medial rectus had not been excessively recessed in the initial surgery for correction of esotropia. In these three patients, the medial rectus attachment to the sclera was found at a distance less than 11 mm from the limbus with a range of 10-10.5. The patient showed an esotropia of 14 PD after surgery required additional surgical intervention.
This study has some limitations. First, a limited number of patients could be included in each group because of its retrospective design. Second, all the consecutive exotropia patients in our study had only been operated on medial rectus muscles for esotropia and the study had a lack of consecutive exotropia patients who had undergone lateral rectus resection in the initial surgery, so our results can not be generalized. Furthermore, considering the appearance of more exodrift over time, the postoperative follow-up period was short.
In conclusion, the results of present study suggested that there was no significant difference between the amount of previously recessed medial rectus advancement and the amount of untouched medial rectus resection advised from a standard surgical dosing table. Also, we demonstrated that unilateral medial rectus advancement with lateral rectus recession is an effective surgical procedure for treating consecutive exotropia with minimum side effects. Advacement of the previously recessed medial rectus back to the original insertion improved adduction deficits. However, our data need to be confirmed by prospective studies with more patients and longer follow-up.
Disclosure of interest
The authors report no conflict of interest
References
- Ganesh A, Pirouznia S, Ganguly SS, et al. (2011) Consecutive exotropia after surgical treatment of childhood esotropia: A 40-year follow-up study. Acta Ophthalmol 89: 691-695.
- Yurdakul NS, Ugurlu S (2013) Analysis of risk factors for consecutive exotropia and review of the literature. J Pediatr Ophthalmol Strabismus 50: 268-273.
- Oğuz V, Arvas S, Yolar M, et al. (2002) Consecutive exotropia following strabismus surgery. Ophthalmologica 216: 246-248.
- Han SY, Han J, Rhiu S, et al. (2016) Risk factors for consecutive exotropia after esotropia surgery. Jpn J Ophthalmol 60: 333-340.
- Gesite-de Leon B, Demer JL (2014) Consecutive exotropia: Why does it happen, and can medial rectus advancement correct it? J AAPOS 18: 554-558.
- Akbari MR, Hassanpoor N, Aghsaei Fard M, et al. (2018) Clinical and Histopathologic Features of Consecutive Exotropia. Strabismus 26: 84-89.
- Folk ER, Miller MT, Chapman L (1983) Consecutive exotropia following surgery. Br J Ophthalmol 67: 546-548.
- Gong Q, Wei H, Zhou X, et al. (2016) Risk factors analysis of consecutive exotropia: Oblique muscle overaction may play an important role. Medicine (Baltimore) 95: e5644.
- Patel AS, Simon JW, Lininger LL (2000) Bilateral lateral rectus recession for consecutive exotropia. J AAPOS 4: 291-294.
- Nabie R, Gharabaghi D, Rahimloo B (2008) Bilateral Medical Rectus Advancement versus Bilateral Lateral Rectus Recession for Consecutive Exotropia. J Ophthalmic Vis Res 3: 114-117.
- Chang CY, Lin MC (2017) Surgical results for consecutive exotropia. Taiwan J Ophthalmol 7: 100-103.
- Mohan K, Sharma A, Pandav SS (2006) Unilateral lateral rectus muscle recession and medial rectus muscle resection with or without advancement for postoperative consecutive exotropia. J AAPOS 10: 220-224.
- Kasi SK, Tamhankar MA, Pistilli M, et al. (2013) Effectiveness of medial rectus advancement alone or in combination with resection or lateral rectus recession in the management of consecutive exotropia. J AAPOS 17: 465-470.
- Santiago AP, Rosenbaum AL (1999) Surgical dose tables. In: Rosenbaum AL, Santiago AP, Clinical strabismus management, principles and surgical techniques. Philadelphia, PA, WB Saunders Company, 554.
- Donaldson MJ, Forrest MP, Gole GA (2004) The Surgical Management of Consecutive Exotropia. J AAPOS 8: 230-236.
- Chatzistefanou KI, Droutsas KD, Chimonidou E (2009) Reversal of unilateral medial rectus recession and lateral rectus resection for the correction of consecutive exotropia. Br J Ophthalmol 93: 742-746.
Corresponding Author
Dr. Ercan Ozsoy, MD, Department of Ophthalmology, University of Health Sciences, Haseki Training and Research Hospital, Aksaray Adnan Adıvar Street, Fatih, 34130, Istanbul, Turkey, Tel: 90-212 529 44 00, Fax: 90-212 589 62 29.
Copyright
© 2021 Gunduz A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.