Actinomyces Canaliculitis Complicated by Orbital Pyogenic Granuloma
Abstract
A 92 year-old woman with no significant past ocular history presented with a one-year history of bloody tears, pruritus, and an enlarging supero-medial orbital mass with extension through the right upper eyelid punctum. Magnetic resonance imaging of the orbits demonstrated a well-circumscribed, ring enhancing mass of the right anterior supero-medial orbit. Medial orbitotomy and removal of the orbital mass was performed, and histopathology revealed lymphoid proliferation surrounding a microbial infiltrate staining for gram-positive filamentous bacteria with sulfur granules. Overall, the findings were consistent with chronic canaliculitis secondary to Actinomyces species complicated by formation of an orbital pyogenic granuloma. She has had no recurrence of disease at five months of follow-up. To the authors' knowledge, this case is only the second report of pyogenic granuloma as a complication of Actinomyces canaliculitis and the first associated with an orbital mass.
Keywords
Canaliculitis, Actinomyces, Pyogenic granuloma, Orbital mass
Introduction
Actinomyces israelii, a filamentous, branching, gram-positive, and predominantly anaerobic bacterium, is a common cause of canaliculitis. It is characterized by its propensity to cause chronic mucopurulent discharge, thick concretions, and dacryoliths with sulfur granules on histological examination, which are pathognomonic for the infection [1-4]. Pyogenic granulomas of the nasolacrimal system are rare, with data mostly limited to case reports and series [5-7], which suggest an association with prior placement of silicone punctal plugs [8]. The correlation between Actinomyces canaliculitis and pyogenic granuloma formation remains poorly documented. To the authors' knowledge, there has only been one reported case in the literature of a canalicular pyogenic granuloma attributed to Actinomyces infection [7]. Here we present the case of a patient who developed a canalicular pyogenic granuloma with orbital extension in association with chronic Actinomyces canaliculitis. The collection and evaluation of protected patient health information were compliant with the Health Insurance Portability and Accountability Act, and an informed consent for publication of identifiable photographs was archived in the patient's medical record.
Case Presentation
A 92 year-old woman with a past medical history of hypertension and hyperlipidemia was initially referred for evaluation of an eyelid mass that had been enlarging with periods of waxing and waning over the prior year. She endorsed persistent blurry vision, pain, bloody tears, pruritus, and erythema, all of which had been refractory to oral cephalexin and topical erythromycin, moxifloxacin, ofloxacin, and azestaline.
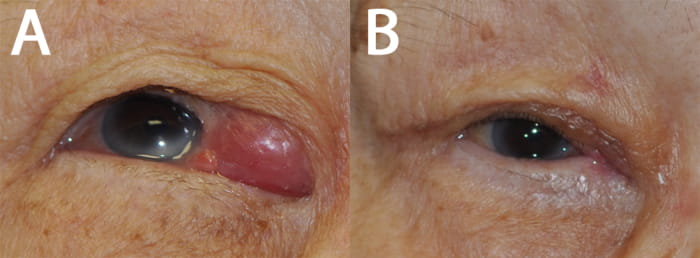
On examination, she was afebrile with no palpable preauricular, submandibular, or cervical lymphadenopathy. Visual acuity was 20/50 in both eyes, and intraocular pressure was 15 and 13 mmHg in the right and left eye, respectively. External examination revealed a large well-circumscribed mass along the right medial upper eyelid with papillomatous extension from the upper punctum, appearing pink with fronds of vessels (Figure 1A). There was no obvious obliteration of the surrounding punctal architecture, and no purulent or bloody discharge could be manually expressed. On attempted probing and irrigation, the right upper eyelid punctum was found to be completely obstructed by the mass.
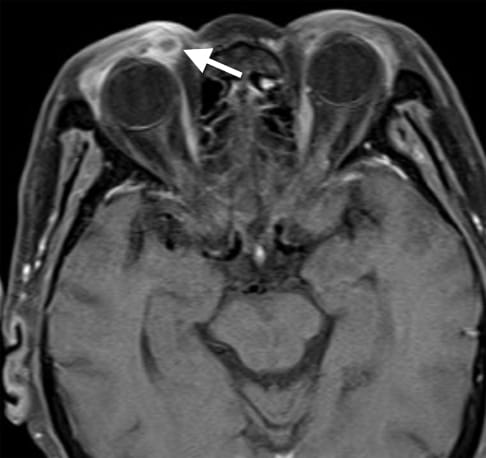
Due to concern for an infiltrative process, a same-day biopsy of the anterior portion of the mass extruding from the punctum was performed. The histopathology revealed a benign pyogenic granuloma. Magnetic resonance imaging of the orbits demonstrated a peripherally contrast-enhancing, well-circumscribed lesion of the right anterior supero-medial orbit measuring 6 x 9 x 8 millimeters (Figure 2).
Given the associated discomfort, progressive increase in size of the mass, visual obstruction, and possibility of an underlying tumor or infection suggested by radiographic findings, the decision was made to proceed with a right medial orbitotomy with removal of the mass. On gross examination, the mass was well-encapsulated with a fibrous appearance. It exhibited extension with a cicatricial process into the anterior medial orbit, tarsus, superior conjunctival fornix, and additionally through the superior punctum. A nasolacrimal stent was placed concurrently to minimize the risk of post-operative obstruction in light of chronic inflammation with distortion of normal canalicular architecture. The patient was incidentally found to have spontaneous discharge from the left lower punctum intraoperatively, which prompted culture and analysis.
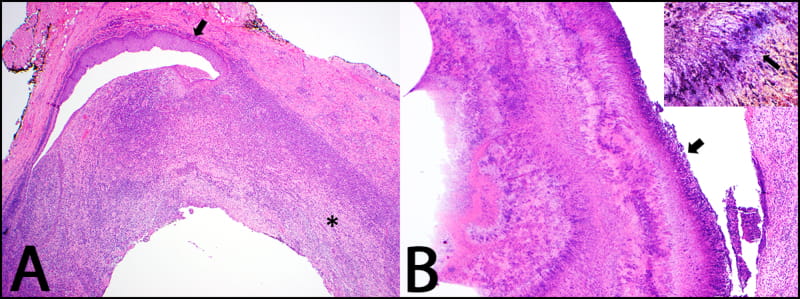
Histopathologically, a cystic inflammatory lesion was identified involving the wall of the canaliculus and extending into the punctum and adjacent conjunctiva (Figure 3A). The lesion demonstrated a zonal pattern of granulomatous inflammation encasing granulation tissue and basophilic tangles of filamentous microorganisms admixed with cellular debris and clusters of neutrophils consistent with "sulfur granules" (Figure 3B). Histochemical studies highlighted a conglomeration of gram-positive filamentous bacteria which were also positive for Gomori methenamine silver staining and negative for acid-fast bacilli and Fite-Faraco stains (Figure 3B, inset). The overall findings were consistent with chronic canaliculitis secondary to Actinomyces species with an overlying pyogenic granuloma. Culture from the left lower punctum yielded viridans group Streptococci.
The patient's post-operative course was uncomplicated with routine healing (Figure 1B). She completed a 10-day course of oral levofloxacin and two-week course of topical ofloxacin drops twice daily in both eyes. She has had no recurrence at five months of post-operative follow-up.
Discussion
While Actinomyces species are some of the most common pathogens responsible for acute and chronic canaliculitis, other common pathogens include Staphylococcus and Streptococcus species [1-4]. Patients frequently present with chronic epiphora, mucopurulent discharge, medial canthal swelling or pain, or a pouting punctum. Dacryoliths can occasionally be expressed manually on clinical examination. These stones often stain for gram-positive branching filamentous rods, a classic sign of Actinomyces infection. Most patients do not have resolution with medical management alone and require surgical intervention, such as canaliculotomy with curettage, punctoplasty, antibiotic irrigation, and/or stenting, for definitive treatment [3,4]. Similarly, our patient's case was refractory to medical management and was uniquely complicated by the formation of a large pyogenic granuloma extending into the anterior orbit.
Also known as lobular capillary hemangioma, the term pyogenic granuloma is a misnomer, as the lesion contains neither a pyogenic nor granulomatous component. As seen in this case, the masses typically present as pedunculated or wide-based nodules with a lobular arrangement of capillaries at their base [9]. The authors found only one prior reported case of canalicular pyogenic granuloma attributed to Actinomyces infection [7]. Pyogenic granulomas commonly form in areas of prior trauma or chronic inflammation, such as surgical sites, chronic chalazia, and encasing silicone punctal plugs or nasolacrimal stents [8]; however, it remains important to rule out an underlying malignancy. Specifically, when a pyogenic granuloma is associated with a discrete mass, it is imperative to determine whether the mass itself is malignant and disturbing the underlying tissue architecture thereby leading to chronic inflammation and pyogenic granuloma formation. In our patient, imaging revealed a ring-enhancing component, which also raised suspicion for an infectious etiology, as the enhancement suggested edema and inflammation surrounding a uniform mass.
While masses of the nasolacrimal system are rare, the differential diagnosis encompasses a broad spectrum, including benign neoplasms (e.g., papillomas, nevi and apocrine cysts), malignant neoplasms (e.g., squamous cell carcinoma, adenocarcinoma, melanoma and adenoid cystic carcinoma), various other non-epithelial tumors (including lymphoproliferative processes), and inflammatory lesions [5]. Studies analyzing biopsies from patients presenting with primary acquired nasolacrimal duct obstruction reveal that most biopsies demonstrate non-specific inflammation or fibrosis [10,11]. Further, one study showed no lacrimal sac tumors in 202 biopsies from 166 patients with nasolacrimal duct obstruction, prompting the authors to suggest only performing biopsies in cases with high index of suspicion for malignancy [10].
Simple resection of pyogenic granulomas of the eye and ocular adnexa has a low recurrence rate of approximately 3% [12]. Specifically, reports of pyogenic granulomas of the nasolacrimal system note long recurrence-free windows [6,8]. However, in cases secondary to infectious processes, such as Actinomyces, it is important to establish source control, which is achieved definitively through canaliculotomy with curettage for decompression, punctoplasty, antibiotic irrigation, and possible canalicular stenting. Consideration should be made to treat concurrently with topical and/or systemic antibiotics.
Pyogenic granuloma formation is a rare complication of chronic Actinomyces canaliculitis. We describe a unique case of an orbital pyogenic granuloma secondary to chronic canalicular inflammation caused by an indolent course of atypical Actinomyces infection. In cases of a canalicular pyogenic granuloma, it is important to consider Actinomyces but also to rule out an underlying inflammatory or neoplastic process. Treatment with medical management alone will likely lead to incomplete response; thus, definitive mass resection, canaliculotomy, and possible stenting followed by a course of antibiotics is necessary to ensure prolonged response.
Disclosures
The authors report no conflicts of interest.
References
- Briscoe D, Edelstein E, Zacharopoulos I, et al. (2004) Actinomyces canaliculitis: Diagnosis of a masquerading disease. Graefe's Arch Clin Exp Ophthalmol 242: 682-686.
- Kaliki S, Ali MJ, Honavar SG, et al. (2012) Primary Canaliculitis. Ophthal Plast Reconstr Surg 28: 355-360.
- Yuksel D, Hazirolan D, Sungur G, et al. (2012) Actinomyces canaliculitis and its surgical treatment. Int Ophthalmol 32: 183-186.
- McKellar MJ, Aburn NS (1997) Cast-forming Actinomyces israelii canaliculitis. Aust N Z J Ophthalmol 25: 301-303.
- Heindl LM, Jünemann AGM, Kruse FE, et al. (2010) Tumors of the Lacrimal Drainage System. Orbit 29: 298-306.
- Bagheri A, Rafati N, Salim RE, et al. (2014) Free-floating Pyogenic Granuloma of the Lacrimal Sac. Orbit 33: 156-158.
- Singh CN, Thakker M, Sires BS (2006) Pyogenic Granuloma Associated With Chronic Actinomyces Canaliculitis. Ophthalmic Plast Reconstr Surg 22: 224-225.
- Joganathan V, Mehta P, Murray A, et al. (2010) Complications of intracanalicular plugs: A case series. Orbit 29: 271-273.
- Mills SE, Cooper PH, Fechner RE (1980) Lobular capillary hemangioma: The underlying lesion of pyogenic granuloma. A study of 73 cases from the oral and nasal mucous membranes. Am J Surg Pathol 4: 471-479.
- Lee-Wing MW, Ashenhurst ME (2001) Clinicopathologic analysis of 166 patients with primary acquired nasolacrimal duct obstruction. Ophthalmology 108: 2038-2040.
- Anderson NG, Wojno TH, Grossniklaus HE (2003) Clinicopathologic Findings From Lacrimal Sac Biopsy Specimens Obtained During Dacryocystorhinostomy. Ophthalmic Plast Reconstr Surg 19: 173-176.
- Ferry AP (1989) Pyogenic granulomas of the eye and ocular adnexa: A study of 100 cases. Trans Am Ophthalmol Soc 87: 327-347.
Corresponding Author
Sanja Cypen G, MD, Division of Oculofacial Plastic & Orbital Surgery, Department of Ophthalmology, Gavin Herbert Eye Institute, University of California, Irvine 850 Health Sciences Road, Irvine, California, 92697, USA.
Copyright
© 2021 Merriott DJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.