Improving Glasgow Coma Scale (GCS) Competency of Nurses in One Acute Stroke Unit - A Nursing Initiative Project
Abstract
Deterioration is common during acute phase of stroke. Early identification and detection of stroke is important monitoring role of a nurse. The Glasgow coma scale (GCS) has been used predominantly by healthcare professionals including nurses to assess any changes of patient's level of consciousness. The aim of the article is to discuss the importance of GCS in clinical practice, explore the nurse's understanding and practical application of GCS in an acute stroke setting and highlight the strategies of improving GCS competencies of nurses.
Keywords
Glasgow coma scale, Stroke, Competency, Education, Nurses
Introduction
Glasgow coma scale (GCS) is used to assess patient's level of consciousness. The healthcare professionals including nurses have been used it over the past 4 decades to evaluate a neurological status of patients suffering from conditions like traumatic brain injuries or stroke. The GCS assessments also demonstrate the evolution of the injury which is central for decision making [1]. It is an also vital tool for research studies [1]. The GCS has 3 main components namely; eye opening (E), verbal response (V), and motor response (M). Table 1 shows the breakdown of the indicators.
The maximum score is 15 and the minimum is 3 [2]. The GCS score must be summarized into score of each component. For example, a patient is assessed by a nurse with a GCS score of 11; he opens his eyes spontaneously (E4), responds inappropriately to questions (V3), and withdraws to pain when applying central pain stimulus (M4). This result is recorded in patient's neurological vital signs and must be communicated with the physicians. Historically, the GCS is used with people who have sustained a traumatic brain injury (TBI). The GCS range (Table 2) is classified into three severity categories; mild (GCS 13-15), moderate (9-12) and severe (3-8) categories [3,4]. "These categories are valuable indicators of injury severity; in the initial stages of assessment the depth of impairment of consciousness along with more long‐term evaluations of duration of loss of consciousness can provide a useful measure of the brain injury [4]".
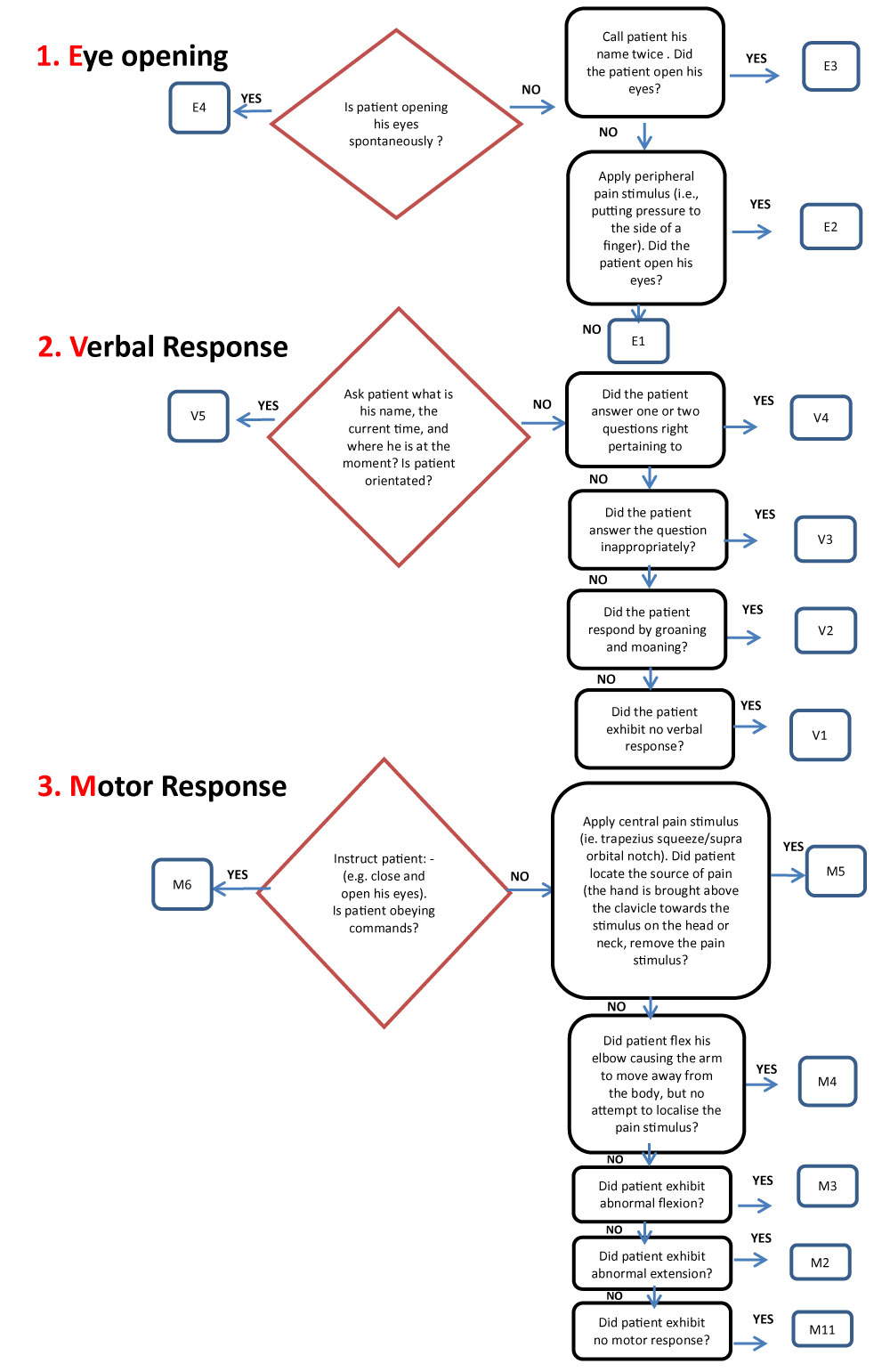
In order to understand the clinical application of GCS in practice, it is important how GCS is performed. De Sousa & Woodward [2] illuminated on how to perform the GCS in detail and highlighted the role of a nurse in accurate monitoring, recording and interpreting a GCS score. A simple algorithm (Figure 1) illustrates on how GCS is done properly. It guides healthcare professionals including nurses when assessing patients. In essence, nurses must consider some of the important points when doing a GCS to patient. Putting a non- numeric response such as "C" in eye opening component if a patient has condition that enforces closure of his eyes (e.g. periorbital oedema) [5]; "T" if patient is intubated or having tracheostomy [1,2,4,6].
Importance of GCS in Stroke Care
The use of GCS in stroke setting is essential for some reasons:
GCS establishes and provides a patient's baseline information
In stroke, GCS has been utilized by emergency room (ER) and ward nurses on patient's admission. The initial assessment of patient's GCS establishes a baseline information and an index of comparison of neurological status.
GCS is used to monitor post thrombolysis monitoring
A thrombolytic therapy is a treatment that dissolves a clot using an intravenous tissue plasminogen activator (tPA). It is given to eligible stroke patients. The monitoring role of a nurse is crucial whilst a patient is on this treatment. Hence, the application of GCS is fundamental in detecting a patient's deterioration following a thrombolytic therapy.
GCS is also used as an outcome measure
The use of GCS in strokes serves a tool to evaluate whether the patient is improving or deteriorating. A drop of GCS of 2 must be reported immediately to the physicians because it suggests a declining neurological status. A diagnostic examination like computerized tomography (CT) of brain is required to exclude any evolving stroke. The GCS is a core part of various clinical guidelines and has been used in trials and research as an outcome measure. In addition to being a guide for initial decision making, trends in responsiveness shown by changes in the Glasgow Coma Scale remain important [1,6].
GCS can also detect raised intracranial pressure
Changes in GCS accompanied by cushing signs (e.g. high blood pressure, low pulse rate headache and vomiting) may suggest signs and symptoms of raised intracranial pressure (ICP). The GCS and vital signs monitoring help nurses to detect, recognize and identify these early red flag signs of raised ICP. And early recognition of raised ICP can saves patient's lives and prevent further complications following a stroke.
The aim of the article is to discuss the role of GCS in clinical practice, explore the nurse's understanding and practical application of GCS in an acute stroke setting and highlight the strategies of improving GCS competencies of nurses. The project was initiated in one acute hospital in Riyadh Kingdom Saudi Arabia among nurses working in stroke unit. These nurses use GCS routinely in nursing practice but their knowledge and practical application of GCS have not been assessed and validated.
Method
Phases
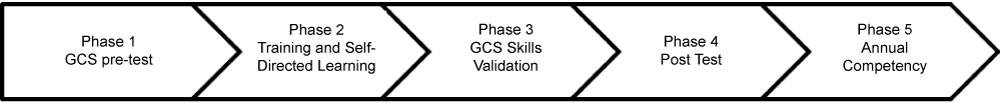
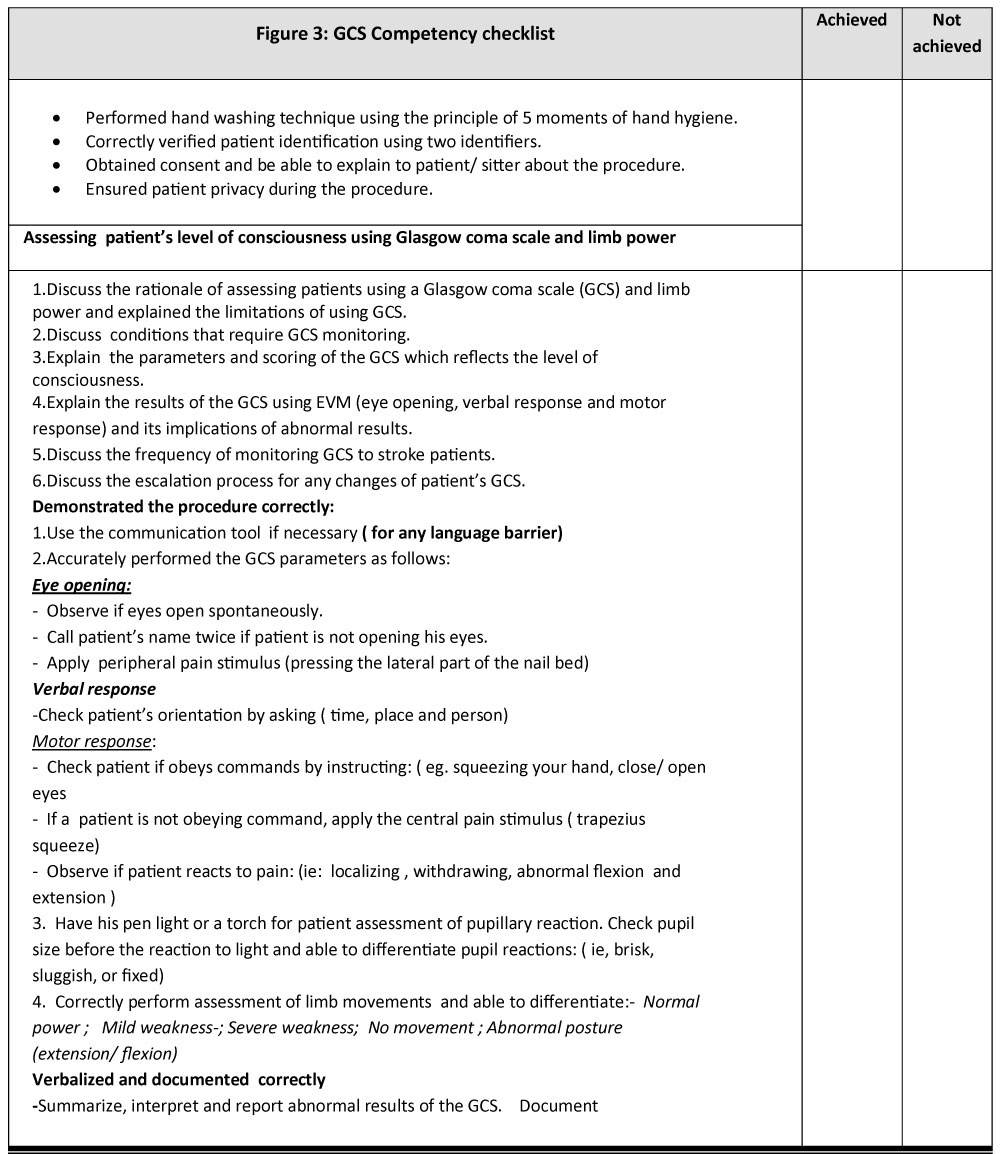
Five (5) phases were involved in in the development of GCS competencies of nurses (Figure 2). The first phase is to gauge the level of understanding of nurses on the use of GCS in practice using a GCS pre-test- questionnaire. A pre-test is a validated 20- item multiple choice question relevant to the GCS. A pre-test was administered to nurses working in acute stroke unit. They were given 20-minute to complete the test and checked independently by the clinical resource nurses (CRN) or a clinical practice facilitator with no discussion of results. The second phase is to develop a GCS competency checklist and implement it with the stroke nurses (Figure 3). The CRN assessed the nurses individually. The CRN observed and recorded the missed points and debrief the nurses on improvement areas. The third phase is to mandate all nurses to read and visit and study the link on GCS: http://www.glasgowcomascale.org/. This link provides a structured approach on how to use GCS. It is a self-directed e-learning tool to teach nurses how to perform GCS accurately to patients. It is supported with evidence-based learning materials and video presentation to demonstrate each component of the GCS. The fourth phase is to administer post -test questionnaire to all nurses in acute stroke unit and discuss and compare the result of the pretest. This was done 2 weeks after the GCS competency. A repeat GCS competency check was done if deemed necessary. Fifth phase is to do an annual GCS competency check as an update.
Data collection and analysis
The identified incorrect answers in the given theoretical and competency tests were summarized into emergent themes.
Results
Result 1: Participant's profile. The project was participated by 55 nurses working in acute stroke unit; 94.50% (n-52) were females and 5.50% (n-3) were males.
Result 2: GCS Pre and post test.
Result 3: Emergent themes of nurses' mistakes in performing GCS.
Summary of results
A total of 55 nurses working in acute stroke unit participated in the project and 94.50% (n-52) were females and 5.50% (n-3) were males . Majority of them took the GCS pre- and post-tests and had their GCS assessment by the unit clinical resource nurse (CRN) who takes the roles as a clinical practice facilitator.
Reflected in Table 3, some of the nurses had confusions on: (1) The difference between localizing and withdrawal to pain when assessing motor response; (2) Difference between abnormal flexion and abnormal extension and their indications; (3) Indications of GCS parameter such as GCS score below 8, GCS score between 9 to 12, and GCS score of 13 to 15.
From the GCS competency check, some of the inaccuracies of nurses (Table 4) assessing GCS include: (1) Using central pain stimulus when assessing for eye opening, (2) Use of hard instrument (e.g. pen) when applying pressure to nail beds; (3) Use "inappropriate words" and "confusion" interchangeably when assessing verbal response; (4) Checking eye pupil reaction first and followed by assessing the pupil size; (5) Asking only one or two questions to elicit orientation level; 6) Using a peripheral pain stimulus when assessing a motor response; (7) Differentiating between localizing and withdrawal to pain; and the (8) Use of sternal rub in applying a central pain stimulus.
Discussion
Assessment of consciousness level is considered as an autonomous responsibility of nurses who care for the patients with neurological conditions [7]. From this project, stroke nurses demonstrate a good theoretical knowledge on clear indication of GCS and its importance, assessment of eye opening and verbal response, however, there were some critical points that need clarification on the aspect of examining a motor response from patients. Specifically, nurses must learn (a) how to differentiate localizing from withdrawal to pain stimulus; (b) differentiate abnormal flexion from extension; (c) and interpret the GCS score range.
Nurses have used GCS routinely in clinical practice in order to assess the level of consciousness for patients following a stroke, yet, there is a clear evidence of high level of confusions and inaccuracies of nurses' performance in GCS. These inaccuracies could compromise patient safety, lead to inability to recognize early signs of neurological deterioration, and affect patient's outcome. Reith, et al. [8] & Santos, et al. [9] explained that nurses should know and recognize changes that may occur with the patient in order to act promptly because nursing care is based on critical observation and right evaluation.
In assessing motor response, the literatures explained that (a) A score of M6 means patients are obeying commands; (b) A central pain stimulus must be applied (eg. trapezius squeeze) in order to elicit a response and observe if a patient localizes (M5) or withdraws to pain (V4); (c) Localizing to pain (M4) is observed when the patient moves a limb in an attempt to locate and remove the source of the painful stimulus; (d) Withdrawal to pain (M4) is demonstrated when the patient flexes at the elbow/knee but unable to locate and remove the source of the painful stimuli; (e) Abnormal flexion (M3) is when patient flexes the arm accompanied by shoulder adduction and wrist flexion; (f) Abnormal extension (M2) is described when the patient extends the arm by straightening the elbow accompanied by shoulder adduction and wrist flexion, and (g) None (M1) if no limb response as a result of pain stimulus.
Surprisingly, few nurses still used sternal rub and the applying hard instrument like pen or torch in patient's nail bed as pain stimuli. Braine & Cook [4] explained that the use of sternal rub can cause injury (bruising) to patients especially if it is done repeatedly and response can be difficult to interpret [5]. On the other hand, "applying pressure to the nail bed can easily be damaged especially when hard instruments such as pens are applied [4,10,11]".
From the study of Kaur, et al. [12] only 2.96% of nurses have good knowledge in GCS which raises concerns on the significance of knowledge and skill in assessing GCS. Moreover, Reith, et al. [8] support the finding that some professionals had poor knowledge about the scale which required the need of continuous training in order to promote standard and reliable use of GCS. Consequently, continuing education and practice on use of the GCS tool are vital. A robust training is paramount in achieving GCS competencies of nurses.
The phases (Figure 2) involved in improving competencies shows significant impact to increase awareness on theoretical and practical applications of GCS in clinical practice. The use of pre and post GCS test helped to gauge nurses' understanding and correct pre-conceived insights of GCS. In the past, there was no existing competency used by the stroke unit. A GCS competency checklist (Figure 3) was developed to guide the assessor to identify and discuss nurse's performance related to GCS assessment of patient. The on-line link http://www.glasgowcomascale.org/ offers nurses a learning opportunity to better understand standards and skills on how to do the GCS properly. This link is supported by a video presentation and evidence-based guidelines in the assessment of GCS [6]. And nurses were encouraged to visit and study the link as a self-directed learning module. The GCS training session had been amalgamated to the Stroke Workshop. The stroke workshop is regularly conducted once a week for nurses to intensify knowledge and skills on GCS. And nurses should have a mandatory annual update and competency on GCS. Moreover, it is imperative that nurses assessing their colleagues must be deemed competent first before taking the GCS skill validation. It illuminates consistency and standardization of the skill execution. The use of GCS algorithm (Figure 1) is simple guides that gives nurses a clarity of specific questions and instructions to elicit a patient response from assessment.
Overall, the use of pre and post-test, a robust training and self - directed learning module, a competency tool and an annual update, envisages a competency framework to improve nurses' performance in GCS. This framework serves as a cornerstone of professional development to enhance nurse's skill in clinical setting.
Limitations
Although the project is conducted in a small population of nurses working within a stroke setting, it still gives a clear cut of a skill-knowledge gap on the application of GCS in practice. The project did not investigate the correlation factors such as educational background of nurses, years of experience as a nurse, and other units such critical care, emergency, surgical and medical units which may or may not affect the theoretical and practical application of GCS in practice. Further studies are needed to examine these factors affecting the performance of nurses in application of GCS.
Keypoints
1. Education and developing competencies are central themes in this project.
2. Stroke nurses are frontlines in the provision of holistic care to acute stroke setting. Therefore, nurses looking after stroke must be adequately armed with specialized knowledge and skills on the use and application of GCS.
3. Confusion is high among nurses in integrating GCS to stroke setting. Inaccurate performance of GCS scoring may lead to delay detection of patient's deterioration and could affect patient's outcome following a stroke. Therefore, it is critical to ensure that GCS is done at the right manner.
Conclusion
The GCS is a simple tool, hence, nurses should be adept in applying this valuable assessment skill in clinical practice. Education, competencies and follow-up are key ingredients to ensure that nurses are up to date with the GCS practice.
Time Out - Reflective Practice
1. What is importance of GCS in stroke care?
2. What are the three components of GCS and explain how it is done?
3. Give three (3) key points that you learned after reading this article.
References
- Teasdale G, Allen D, Brennan P (2014a) The Glasgow Coma Scale: An update after 40 years. Nursing Times 110: 12-16.
- De Sousa I, Woodward S (2016) The Glasgow Coma Scale in adults: Doing it right. Emerg Nurse 24: 33-39.
- National Institution for Health and Care Excellence (NICE) (2014) Head injury: Assessment and early management.
- Braine ME, Cook N (2017) The Glasgow Coma Scale and evidence-informed practice: A critical review of where we are and where we need to be. J Clin Nurs 26: 280-293.
- Teasdale G (1975) Acute impairment of brain function-1. Assessing 'conscious level'. Nurs Times 71: 914-917.
- Teasdale G, Maas A, Lecky F, et al. (2014b) The Glasgow Coma Scale at 40 years: Standing the test of time. Lancet Neurol 13: 844-854.
- Thi Hien, M Chae S (2011) The Accuracy of Glasgow Coma Scale knowledge and performance among Vietnamese nurses. Perspectives in Nursing Science 8: 54-61.
- Reith FC, Brennan PM, Maas AI, et al. (2016) Lack of standardization in the use of the Glasgow Coma Scale: Results of International Surveys. J Neurotrauma 33: 89-94.
- Santos WC, Vancini-Campanhano CR, Lopes MC, et al. (2016) Assessment of nurse's knowledge about Glasgow Coma Scale at a university hospital. Einstein (Sao Paulo) 14: 213-218.
- McLernon S (2014) The Glasgow Coma Scale 40 years on: A review of its practice. British Journal of Neuroscience Nursing 10: 179-184.
- The Glasgow structured approach to assessment of the Glasgow Coma Scale. GCS - Eyes Verbal Motor.
- Basauhra Singh HK, Chong MC, Thambinayagam HC, et al. (2016) Assessing nurses knowledge of Glasgow Coma Scale in emergency and outpatient department. Nurs Res Pract 2016.
Corresponding Author
Elmer Catangui, RN, RM, MBA, MSN, PhD Student, Nursing Services, Ministry of National Guard Health Affairs, King Abdulaziz Medical City Riyadh, PO Box 22490, Riyadh 11426, Saudi Arabia; St. Paul University Philippines, Philippines.
Copyright
© 2019 Catangui E. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.