Distal Femoral Extension Osteotomy with a Retrograde Nail for Treatment of pediatric Crouch Gait
Abstract
Correction of persistent crouch gait in pediatric cerebral palsy patients is difficult. A combined distal femoral extension osteotomy (DFEO) along with patellar tendon advancement provides pain relief and improves ambulation. This procedure is commonly performed using fixed angle constructs. Disadvantages of using this technique in cerebral palsy patients include the inability to bear weight postoperatively and delayed rehabilitation. This manuscript describes a familiar approach for DFEO using a retrograde nail and compares the benefits and disadvantages of nail versus plate fixation. The use of a retrograde nail presents an alternative technique for DFEO in cases where the patient's co morbidities, postoperative mobility status, and likelihood of locking plate complications warrant alternative means of fixation.
Key Words
Distal Femoral Extension Osteotomy, Cerebral Palsy, Technique, Crouch Gait, Pediatrics
Introduction
Distal femoral extension osteotomy (DFEO) for the treatment of patients with fixed flexion deformities associated with arthritic conditions and neuromuscular disorders is a well-established procedure [1-3].The use of 90⁰ locking plates for the correction of persistent crouch gait in pediatric cerebral palsy patients has been described with favorable results, including improved mobility, decreased flexion deformity and extensor lag, and increased muscle strength [1-4] Reported complications with this technique in cerebral palsy patients vary with modern reports ranging from less than 5% to 19% [1,3,4]. Frequent complications with use of plate fixation in DFEO include delayed union or nonunion, fixation failure, loss of correction, and neurovascular injury [2,5]. Disadvantages of this technique include early-weight bearing restrictions and slowed rehabilitation, both of which are critical in patients with cerebral palsy. Standard rehabilitation protocols for 90⁰ condylar locking plates include graduated weight bearing beginning at six weeks, but partial weight bearing has been initiated as early as four weeks in pediatric cerebral palsy patients [4,5] Here we describe the technique of DFEO using a retrograde nail in pediatric patients with cerebral palsy and a crouch gait.
Surgical Technique
Preoperative Planning
The degree of distal femoral extension is determined from lateral radiographs of the knee in full extension. Measurements of the tibio-femoral angle and re-creation of the neutral alignment mechanical axis is done by following the technique described by O'Malley et al, 2016 [6].
Patient Positioning
Position the patient in the supine position on a radiolucent table, exposing the entire limb. A Foley catheter should be inserted to aid in fluid resuscitation during the procedure. Draping up to the naval will allow access and mobility of the proximal femur. For bilateral cases, the urinary catheter can be taken up the midline and covered with ioban after appropriate padding is placed. This can then be prepped into the field. For unilateral cases, bumping the operative limb so that the patella is directly anterior will help with exposure. Confirm visualization of the hip, knee, and ankle prior to prepping and draping with c-arm imaging.
Surgical Technique
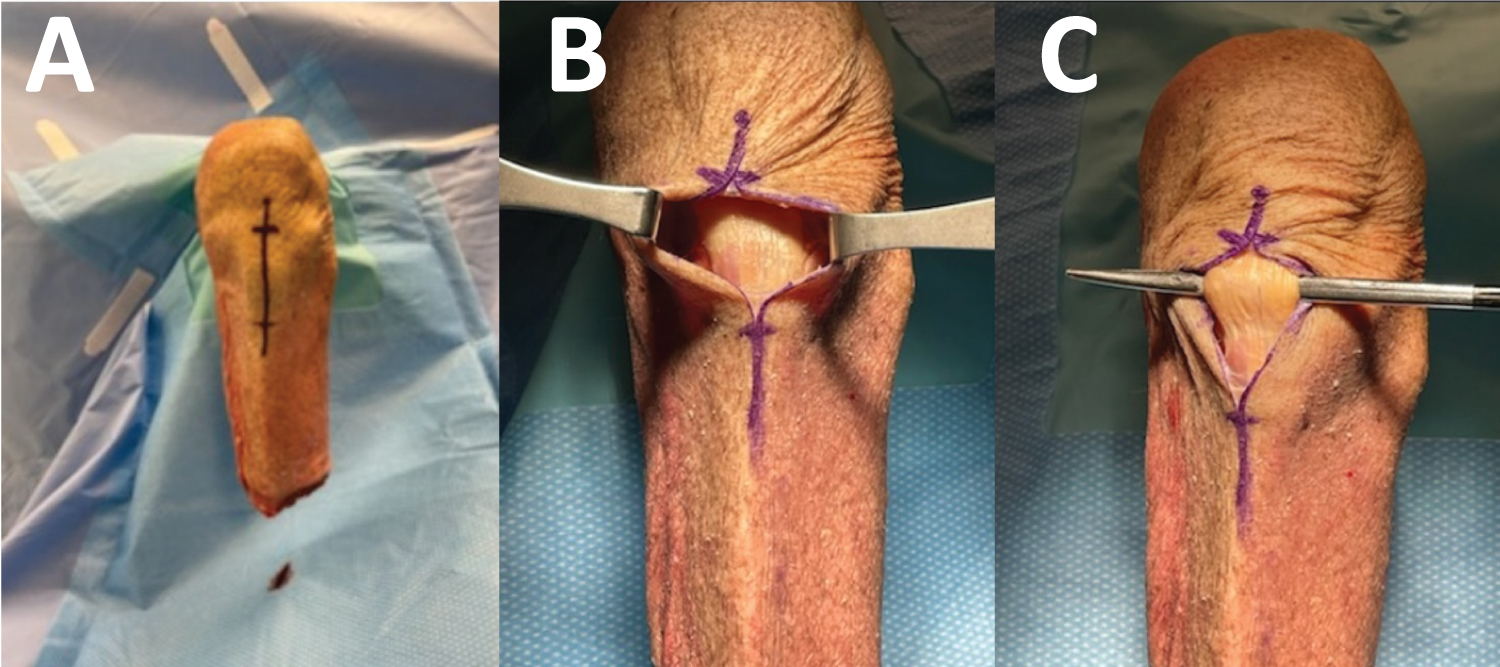
The DFEO and patellar advancement are performed through a midline incision under tourniquet control. To expose the patellar tendon, a midline incision through fascia from the inferior pole of the patella to 3-4 finger breadths past the tibia tubercle is made (Figure 1).
This incision can be made smaller should a patellar reefing be used rather than advancement. With the patellar tendon exposed, there are three options to mobilize the patella:
A. Split
B. Mobilization to the side (easier than normal because of patella alta)
C. Removal of the insertion for preparation of advancement
If electing to proceed with either of the first two options, patellar redundancy should be addressed using the technique described by Hyer et al, [7] If proceeding with the third option, the patellar tendon can be carefully elevated from the tibia tubercle apophasis or the tibia tubercle can be osteotomized with the attached patellar tendon. To help with exposure we recommend partial resection of the patellar fat pad. Care must be taken to avoid injury to the intermeniscal ligament. This exposure also allows easy access to the entry site for a tibia nail should this be used for a concomitant tibia derotational osteotomy. The patellar tendon and patella can then be retracted to allow access to the distal femur (Figure 2).
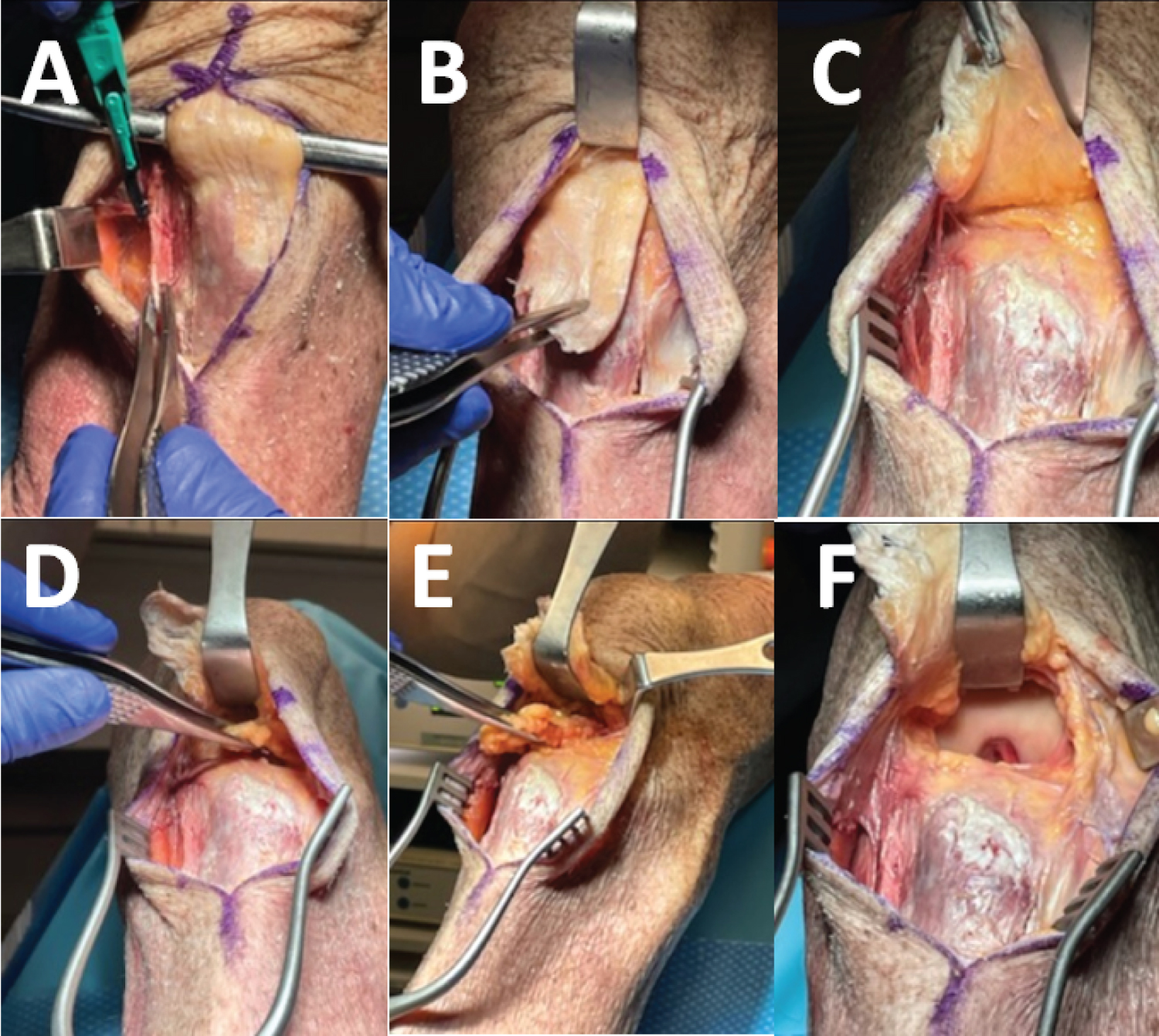
With exposure of the intercondylar notch, the location of the starting point can be selected. The starting point is slightly posterior to a traditional retrograde starting point to allow for more extension when performing the osteotomy (Figure 3). Biplane fluoroscopy is used to verify the appropriate position of the starting point. Insert the guide pin into the femoral canal in line with the anatomic axis of the femur to the desired distance. Following traditional trauma principles we would recommend the nail length be at or proximal to the lesser trochanter to minimize stress. One also needs to take in account whether or not the patient will potentially need proximal femoral work in the future. If so, you may want to end the nail distal to the lesser trochanter. Prior to reaming, make a 2-3 cm incision at the desired level of the metaphysic to perform the osteotomy (Figure 4).
Ideally, this incision will be at the level where the osteotomy site would be. Once the anticipated osteotomy site is marked, vent holes can be drilled and the osteotomy is started using a sagittal saw (Figure 3). A 1cm section of bone should be resected with the initial cut occurring perpendicular to the femur shaft and the second cut at the desired amount of extension (Figure 4). After the removal of bone, the osteotomy is closed down under direct visualization. The guide wire is placed through the previously reamed hole and reamed once more in the distal end of the fragment. To aid interrogation, we recommend over-reaming by two sizes over the desire nail diameter.
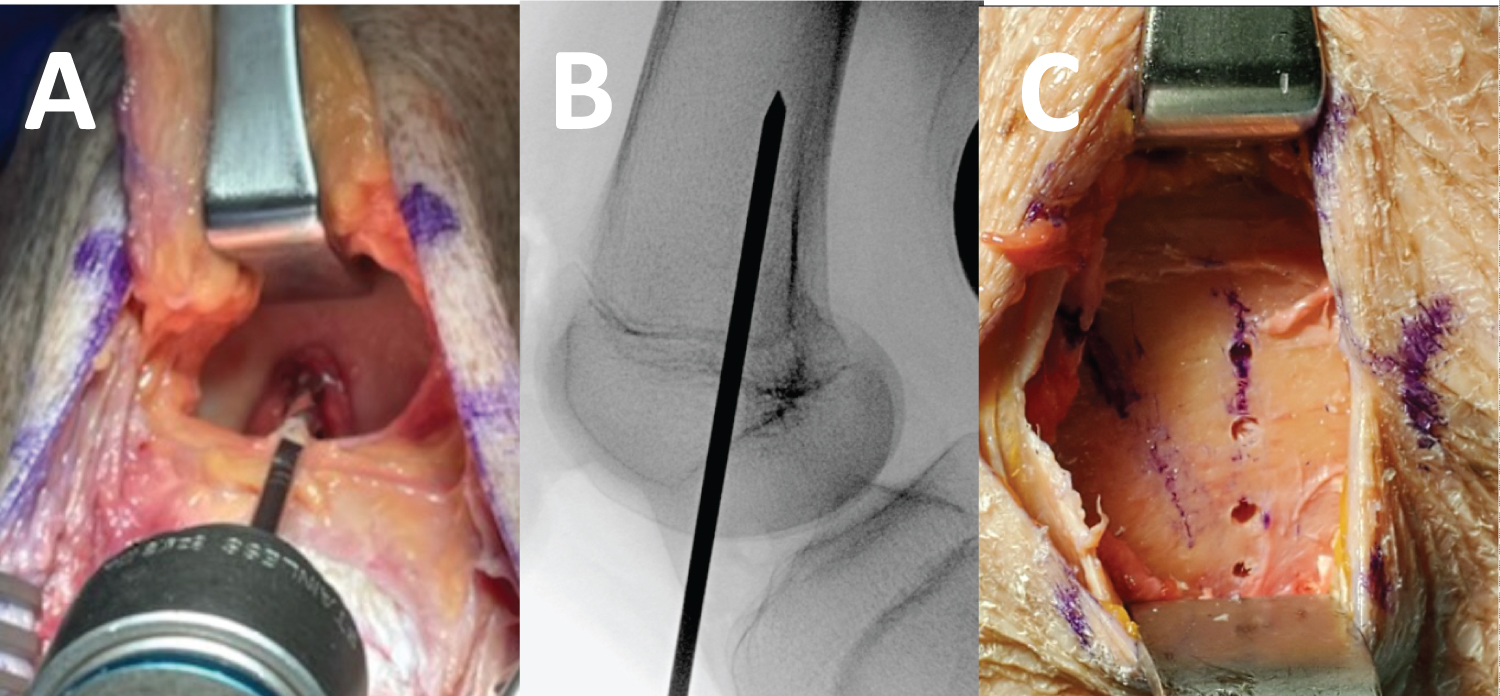
If introducing a larger degree of rotational correction, the nail must be bent straighter than normal using a table top bender. Visual confirmation of the appropriate position of the retrograde nail and reduction of the osteotomy site should be performed (Figure 5). Rotational correction can be introduced using marks through the lateral incision. Following satisfactory correction, the nail is fixed proximally using the oblong hole on the proximal aspect of the retrograde nail (Figure 5). The use of distal screws can then be used (Figure 5). After satisfactory osteotomy and placement of retrograde nail, proceed with patellar tendon advancement or tibia nailing if indicted. The procedure for tendon advancement follows the technique described by Nova check et al,. with securing of the tendon using sutures as shown in (Figure 6) [8].
Postoperative Management
Patients are weight bearing as tolerated for ambulation and mobilization immediately postoperatively. The leg is placed in a knee immobilizer in full extension. Knee exercises and range of motion are permitted postoperatively. Knee immobilizer can be unlocked to 0-60° after four weeks postoperatively. After sufficient quadriceps strength is achieved, the knee immobilizer is discontinued. Postoperative imaging should be obtained prior to discharge and during standard follow-up (Figures 7).
Discussion
This technique for DFEO using retrograde nails in pediatric cerebral palsy patients has not been previously described. The advantages of this technique include allowance for rapid mobilization and rehabilitation in the postoperative period as well as a more stable implant construct. Plate fixation in DFEO provides a familiar surgical technique, but is associated with the potential for hardware irritation, high rates of plate removal, and melanin or nonunion [1,2,6]. Additional concern arises with premature weight bearing, which may result in implant failure or osteotomy collapse. Through the use of a retrograde nail patients were permitted for weight bearing as tolerated postoperatively, providing weight bearing ability four to six weeks earlier than if a locking plate were used. The use of a retrograde nail provides increased stability over locking plates, allowing for early weight bearing and increased mobility with less concern of implant failure compared to locking plate fixation [9,10].
Plate and long nails are used frequently in trauma surgery for long bone fixation and their biomechanical benefits studied extensively. Biomechanical comparative studies with osteoporotic fractures demonstrated the very rigid construct obtained with plate fixation, creating a high-strain environment that may prevent bone healing in, cause stress risers, or peril-implant fractures [11-13]. Intramedullary nails have also been shown to be superior to plating with increased axial stability, rotational control, fatigue life, and load distribution along the femur [14-16]. Because of the desire and importance to mobilize early in cerebral palsy patients, the biomechanical advantages of intramedullary nails provide confidence in faster weight bearing and advanced rehabilitation. Additional benefits of the use of a retrograde nail include the ability to correct larger femoral malrotation deformities as well as mitigate additional surgery to remove hardware, a common procedure after locking plate DFEO [1]. Malrotation of >30º are difficult to correct with plates, but larger rotational deformities can be corrected using the technique described here and allow for easier rotational control without the need for pinning [8].
This technique is recommended for patients where there is a desire to mobilize early due to cognitive or functional indications, where concern of inactivity for 4-6 weeks may prove detrimental to recovery. In patients with poor bone quality or at high risk for nonunion due to co morbidities this technique may also prove beneficial. Intramedullary nailing requires crossing the growth plate centrally and should only be used in patients nearing growth completion. We would continue to recommend the use of plate fixation for the majority of patients, but provide an alternative technique for DFEO with the use of a retrograde nail in cases where locking plate complications present a greater risk. The patient's age, bone quality, ambulatory status, mental and cognitive status, and desire to mobilize should be weighed when considering the mechanical and biologic properties of DFEO with a plate or nail. Indications and contraindications are outlined in (Table 1).
Funding
No funding was received in support of this work.
Conflicts of Interest:
DSH reports no conflicts of interest.
MAS is a consultant for Orthopediatrics
References
- Stout JL, Gage JR, Schwartz MH, et al. (2008) Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy. J Bone Joint Surg Am 90: 2470-2484.
- Rosso F, Margheritini F (2014) Distal femoral osteotomy. Current reviews in musculoskeletal medicine 7: 302-311.
- Rutz E, Gaston MS, Camathias C, et al. (2012) Distal femoral osteotomy using the lap pediatric condylar 90-degree plate in patients with neuromuscular disorders. j pediatrorthop 32: 295-300.
- Aroojis A, Patel M, Shah A, et al. (2019) Distal femoral extension osteotomy with 90 pediatric condylar locking compression plate and patellar tendon advancement for the correction of crouch gait in cerebral palsy. Indian J Orthops 53: 45-52.
- Sherman SL, Thompson SF, Clohisy JC et al. (2018) Distal femoral varus osteotomy for the management of valgus deformity of the knee. J Am AcadOrthop Surg 26: 313-324.
- O'Malley MP, Pareek A, Reardon PJ, et al. (2016) Distal femoral osteotomy: Lateral opening wedge technique. authors tech 5: 725-730.
- Hyer LC, Carpenter AM, Saraswat P, et al. (2021) Outcomes of patellar tendon imbrications with distal femoral extension osteotomy for treatment of crouch gait. J PediatrOrthop 41: 356-366.
- Nova check TF, Stout JL, Gage JR, et al. (2009). Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy: Surgical technique. J Bone Joint Surg Am 91: 271-286.
- Ozkan K, Türkmen I, Sahin A, et al. (2015) A biomechanical comparison of proximal femoral nails and locking proximal anatomic femoral plates in femoral fracture fixation. Indian j Orthops 49: 347-351. sss
- Hoskins W, Sheehy R, Edwards ER, et al. (2016) Nails or plates for fracture of the distal femur? data from the Victoria orthopedics trauma outcomes registry. Bone Joint J 98: 846-850.
- Greiwe RM, Archdeacon MT (2007) Locking plate technology-current concepts. j knee surg. 20: 50-55.
- Rothberg DL, Lee MA (2015) Internal fixation of osteoporotic fractures. Current osteoporosis reports 13: 16-21.
- Aneja A, Teasdall RJ, Graves ML. et al. (2021) Biomechanics of osteoporotic fracture care: Advances in locking plate and intramedullary nail technology. J Orthops Trauma 35: 1-5.
- Pekmezci M, McDonald E, Buckley J, et al. (2014) Retrograde Intramedullary nails with distal screws locked to the nail have higher fatigue strength than locking plates in the treatment of supracondylar femoral fractures: A cadaver-based laboratory investigation. bone joint j 96: 114-121.
- Arvinius C, Parra JLC, Mateo LS, et al. (2014) Benefits of early Intramedullary nailing in femoral metastases. int orthop 38: 129-132.
- Magill H, Ponugoti N, Selim A, et al. (2021) Locked compression plating versus retrograde Intramedullary nailing in the treatment of per prosthetic supracondylar knee fractures: A systematic review and meta-analysis. J Orthops Surg Res 16: 1-9.
Corresponding Author
Daniel S. Hayes, Department of Orthopedic Surgery, Geisinger Medical Center, Danville, PA, USA, Tel: +1(570)939-9916, Fax: (57)214-6700.
Copyright
© 2022 Hayes DS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.