Fracture-Avulsion of the Greater Tuberosity: Arthroscopic Transosseous Augmented Technique
Abstract
The fracture-avulsion of the greater tuberosity represents the 2% of all humerus fracture, but the true incidence is likely to be higher, being challenging the initial diagnosis on X-ray. The fracture-avulsion of the greater tuberosity could have different treatment: Non-displaced or minimal displaced fractures are treated conservatively, while for the displaced or comminuted ones the surgical treatment is preferred. The most important finding of this study is the employment of an all arthroscopic transosseous augmented technique for the treatment of a displaced humeral greater tuberosity fracture-avulsion. This technique showed all its advantages due to the transosseous fixation and arthroscopic approach.
Keywords
Greater tuberosity, Fracture, Avulsion, Shoulder arthroscopy, Transosseous augmented
Introduction
Fractures of the proximal humerus represent approximately 5% of all fractures and almost half of all humeral fractures [1]. The 20% of the latter are represented by isolated fractures of the greater tuberosity (GT) [2]. These fractures may be more challenging to identify on initial plain radiographs because of osseous overlap when the glenohumeral joint is internally rotated. Additionally, small comminuted fragments may simply be overlooked or misinterpreted as calcific deposition within the rotator cuff or intra-articular loose bodies [1]. Recently, Ogawa [3] found that 59% of isolated GT fractures were missed on initial evaluation [3], so that its true incidence may, therefore, be higher [1].
The demographics of patients who sustain isolated GT fractures have been more extensively reviewed, and their occurrence is predominantly in young male [2]. The treatment of this kind of fractures is controversial. Generally non-displaced or minimal displaced fractures are treated conservatively. If the displacement is more than 5 mm or if the fractures are comminuted a surgical treatment is preferred [4]. Although open procedures are preferred for comminuted, widely displaced fractures, arthroscopic procedures can be used for multi fragment bony avulsion of the supraspinatus tendon and isolated one-part GT fractures with minimal displacement [1]. The displacement of the fracture is determined by the rotator cuff attachments on the superior margin of the greater tuberosity that is marked by three distinct flat impressions: The superior, middle, and inferior facets [5]. The arthroscopic technique, even if could appear more demanding allows a more complete evaluation of the shoulder (i.e. associated lesions) and reduces the soft tissue damage [6]. To treat the GT fracture-avulsion different techniques were proposed, such as the tension band wire suture, transosseous braided-tape (BT) and double row suture bridge with anchor [7,8]. The last two options may be considered superior in terms of mechanical proprieties, strength and stability. Especially in comminuted or eggshell fractures when rigid fixation is not feasible only with anchors, with the aim to prevent GT fracture displacement has been recently proposed to use the sub acromial spacer (In Space balloon, Stryker, USA) to better compress and stabilize the fracture [9].
The present technical note describes an original all arthroscopic transosseous augmented (ATA) technique as a fixation method for the avulsion-type greater tuberosity fractures.
Surgical Technique
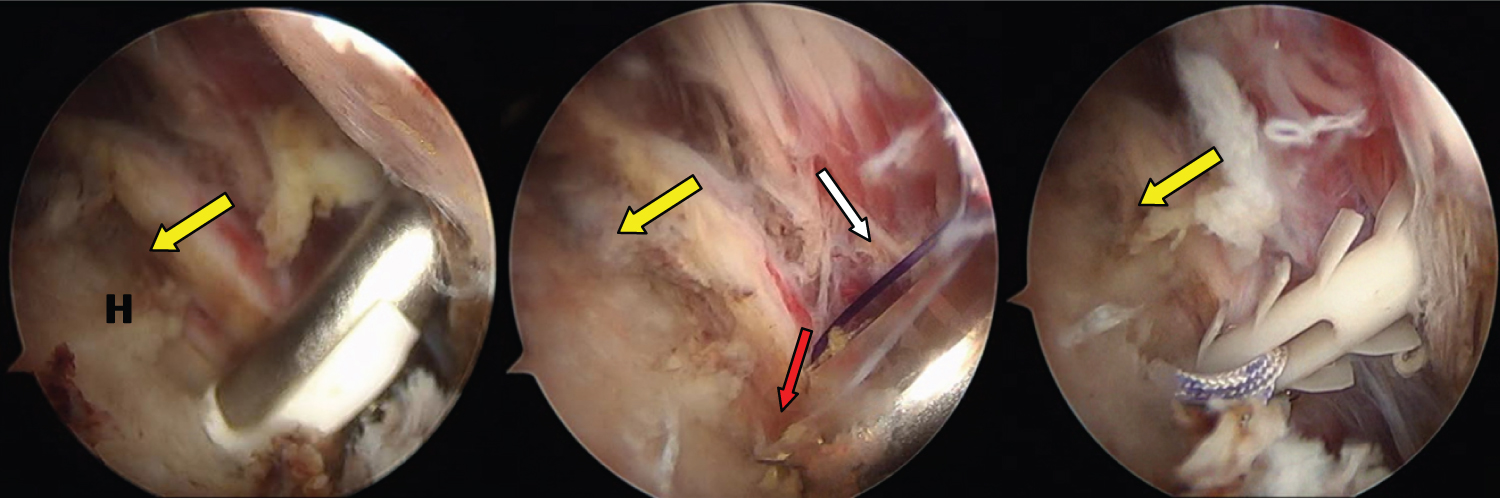
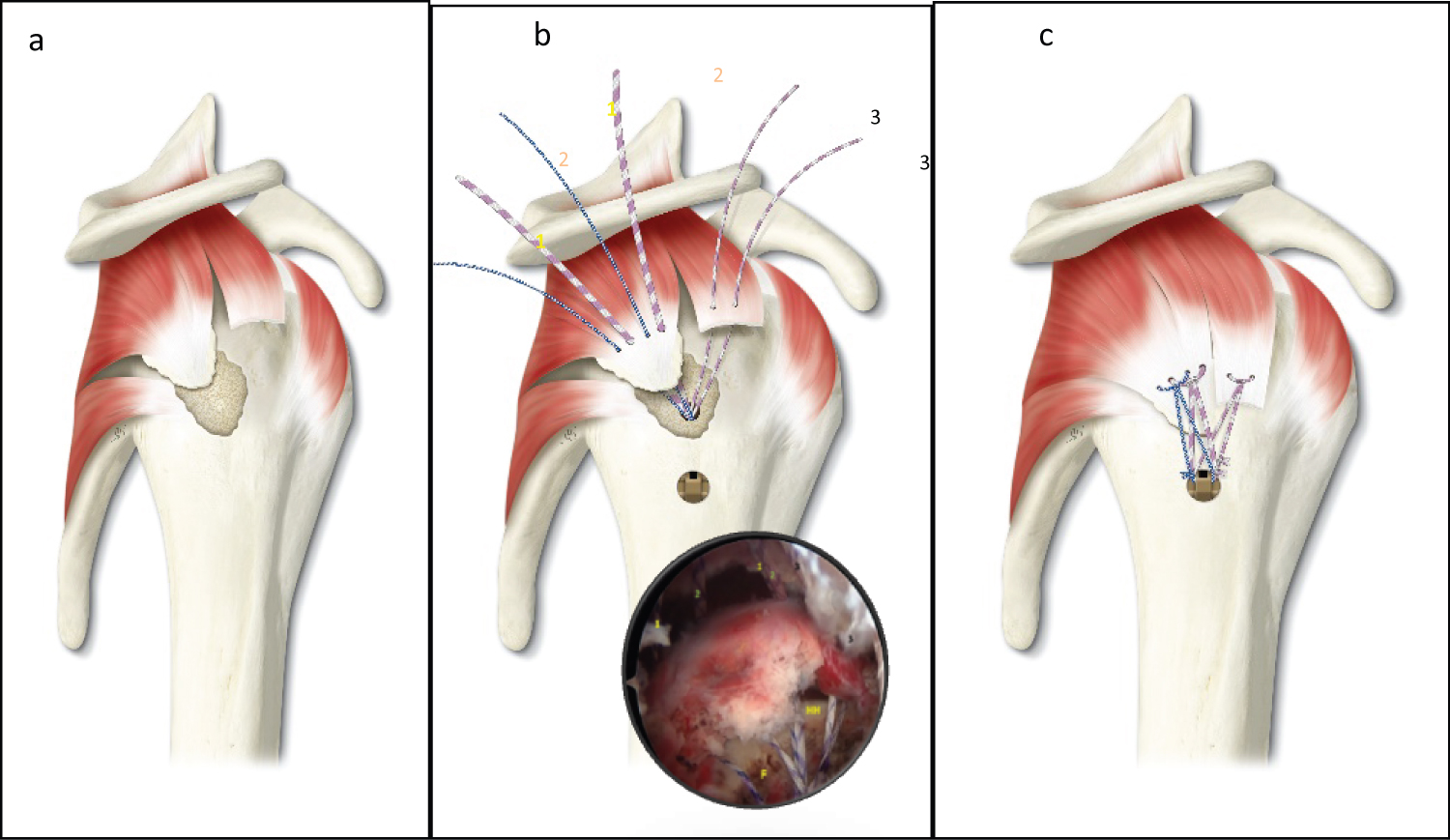
The procedure was performed by the first author with the patient in lateral decubitus with an interscalene cervical plexus block. Four portals were needed for the surgery. With the scope into the intra-articular space from the standard posterior portal, after haematoma removal-from an anterior portal, the fracture-avulsion of the GT mainly located in the middle facet [3] was confirmed. The scope was then moved into the sub-acromial space al mostly totally occupied by a hematoma. With the use of a spinal needle, centered to the lesion and tangent to the fractured area, the supero-lateral portal (SLP) was created. The edge of the bony fragment and the crater of the fracture were debrided. An associated antero-superior rotator cuff tear was identified. Through an additional infero-lateral portal (ILP), performed 2 cm below the SLP, the lateral aspect of the humerus was prepared so to perform the transosseous tunnel with a dedicated instrument: The Superelastic Transosseus Needle® connected with the Taylor Stitcher® Evo (NCS Lab s.r.l. - Medical Devices Factory, Italy) [10]. The lateral entry point is established 2 cm below the lateral fracture margin so to prevent cracking the cortex. Once the tunnel is performed a 1 polydioxanone monofilament (PDS #1, Ethicon, Somerville, NJ) is passed as a shuttle wire. To avoid any peak stress on the healthy bone below the margin of the fracture a cortical lateral augmentation named Elite-SPK® (NCS Lab s.r.l. - Medical Devices Factory, Italy) was employed (Figure 1).
Three different sutures (1 of #1.2 mm and 1 of # 2.2 mm of XBraid TT - non-absorbable, smooth, low-profile UHMWP suture tape, Stryker, USA; 1 HS-Fiber non-absorbable braided UHMWP suture, River point Medical, USA), initially loaded into the eyelet of this PEEK implant, were passed. Both ends of the HS-Fiber suture and of the XBraid TT tape #2.2 mm were medially passed (from posterior to anterior) into the inserted tendon on the bony fragment. Later, the XBraid TT tape #1.2 mm was employed to repair the supraspinatus tendon tear (Figure 2). The sutures were closed in a mattress type, then one limb of each sutures was shuttled from anterior to posterior in the external eyelet of the Elite SPK®, and were laterally tied respectively with their remaining free ends (Figure 2).
Postoperative care
Immediately after surgery and for the first 4 post-operative weeks the patient wore a 15°-20° abduction pillow. Immediately after surgery passive exercises were permitted. From the 4th until the 12th week assisted/active exercises at a minimum load were introduced while the abduction pillow was removed. Around the third month toning exercises were started.
Illustrative Cases
Case 1
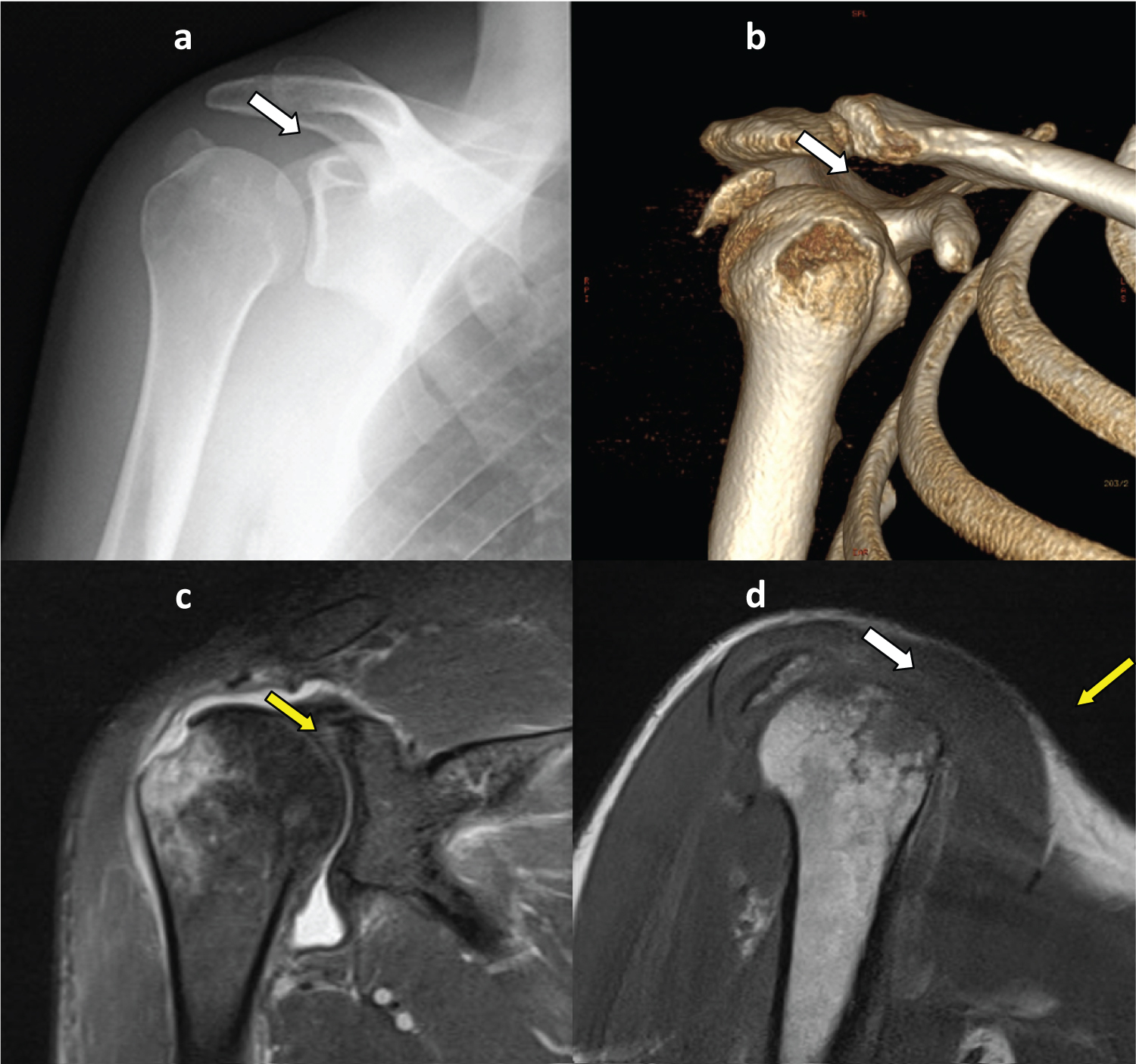
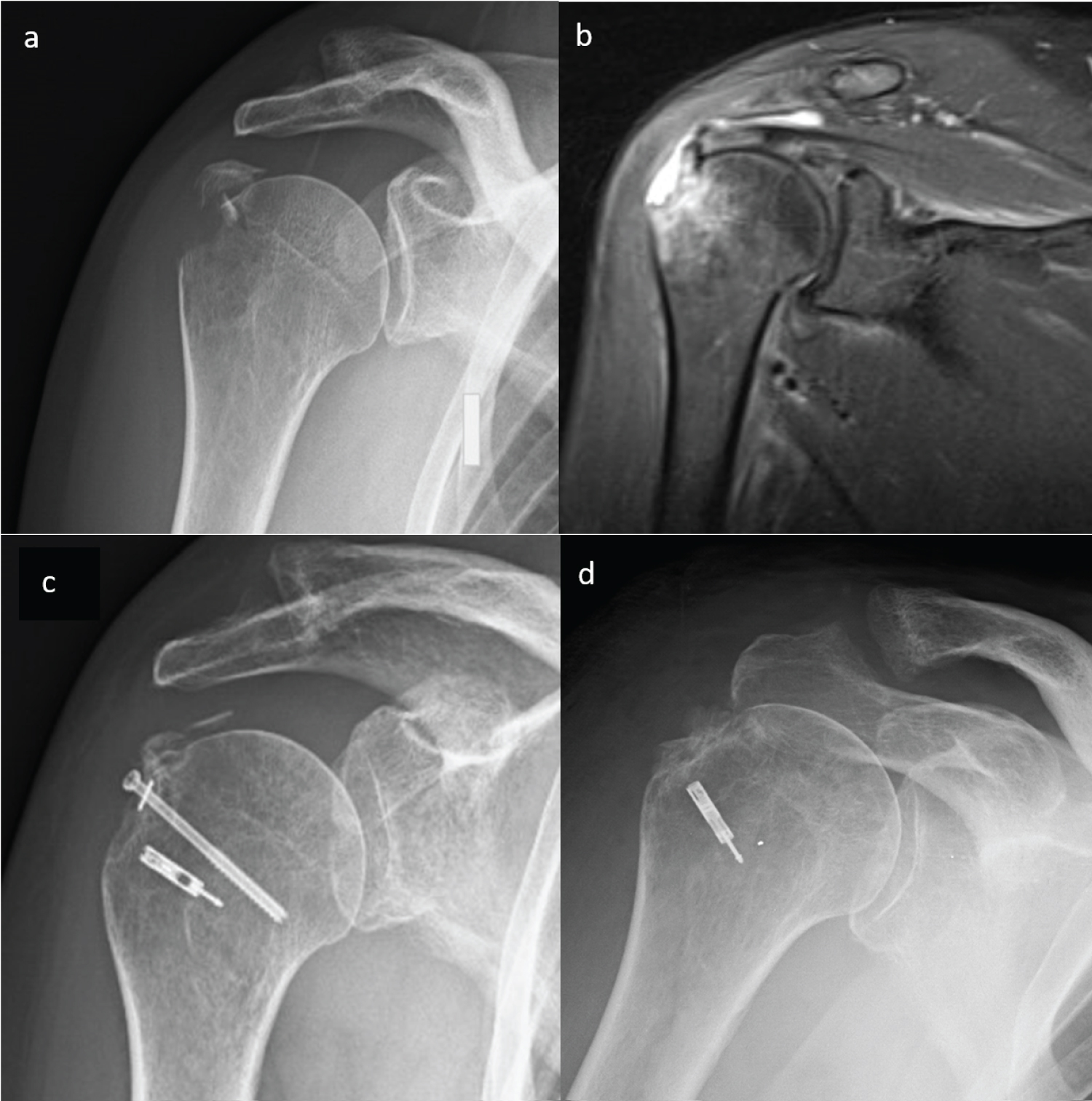
A 45-years-old male reported a direct trauma on his right shoulder following a fall on skis. X-ray performed at emergency room was not apparently of unique interpretation. The patient was discharged and immobilized in a sling for a shoulder contusion. Few days later symptoms (pain, limited range of motion and weakness) worsened and a hematoma appeared on the shoulder. After consulting an orthopedics shoulder surgeon, CT and MR scan were recommended to confirm the diagnosis of avulsion-type greater tuberosity (GT) fracture (Figure 3). The patient underwent surgery 13 days after the trauma.
Case 2
A 56-years-old woman reported an accident at work on her right shoulder. X-ray was performed at emergency room and showed an avulsion-type greater tuberosity fractures. She was immobilized in a sling for shoulder contusion. Once performed MR imaging, ten days after the trauma the patient underwent surgery (open reduction and fixation with a screw with a washer, reinforced with a knotless anchor) and was immobilized in a sling for 30 days. At this time X-ray showed the failure of reduction of the fracture with the screw. The patient was re-operated almost 3 months later the initial trauma (Figure 4).
Discussion
The most important finding of this study is the employment of an all ATA technique for the treatment of a displaced humeral GT fracture-avulsion. The ATA technique here illustrated showed all its advantages due to the transosseous fixation and arthroscopic approach (Table 1). The latter, with the daily advancements, still today seem the treatment of choice with the double-row (DR) suture anchor fixation technique, improving the initial repair strength and restoring the normal anatomy [11]. However, the DR technique presents some concerns regarding the surgical time (longer), the feasibility (high-demanding) and the safety (iatrogenic damage to the intact rotator cuff). In this study the use of ATA technique seems to almost completely overcome all the concerns above reported. Moreover, the ATA technique presented additional valuable aspects, related to 1) The use of the tape instead of conventional high-strength sutures and 2) The use of a lateral cortical augmentation. Regarding the former, from a biomechanical point of view, the tape increases the pressure at the footprint and the construct strength compared with the conventional sutures [12].
The lateral cortical augmentation with its peculiar shape and features may be considered as a suture platform that overcome all the questions related to the bad bone quality of the greater tuberosity [13] that a shoulder surgeon can meet during an avulsion-type greater tuberosity fractures, providing a reliable fixation. In addition, the use of Elite-SPK® shows other beneficial surgical details, reducing the risk of suture cut and bone damage (because there is no sliding of the sutures into the TO tunnel) and generating a compression vector perpendicular to the fracture area. The latter effect results in a maximization of the contact area, with an optimal pressure distribution, while reducing sutures-bone tunnel impingement. Moreover, the transosseous BT presents additionally an economic advantage, being the cheaper [8].
In conclusion, ATA technique demonstrated as a valid surgical option in the treatment of displaced fracture-avulsion of the greater tuberosity of the humerus, and seems to be ideal in such cases with smaller fragment, avoiding the risk of its splitting when using the screw.
Conflicting Interests
The Authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not for-profit sectors.
Informed Consent
Written informed consent was obtained from all individual participants included in the study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Contributorship
All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Acknowledgements
A special thanks to Miss Ilaria Bondi, medical graphic designer (www.illustrazionianatomiche.com) for preparing all the illustrations of this paper.
References
- Gruson KI, Ruchelsman DE, Tejwani NC, et al. (2008) Isolated tuberosity fractures of the proximal humeral: Current Concepts. Injury 39: 284-298.
- Kim E, Shin HK, Kim CH, et al. (2005) Characteristics of an isolated greater tuberosity fracture of the humerus. J Orthop Sci Off J Jpn Orthop Assoc 10: 441-444.
- Ogawa K, Takahashi M (1997) Long-term outcome of isolated lesser tuberosity fractures of the humerus. J Trauma 42: 955-959.
- Godin JA, Katthagen JC, Fritz EM, et al. (2017) Arthroscopic treatment of greater tuberosity avulsion fractures. Arthrosc Tech 6: E777-E783.
- White EA, Skalski MR, Patel DB, et al (2018) Isolated greater tuberosity fractures of the proximal humerus: anatomy, injury patterns, multimodality imaging, and approach to management. Emerg Radiol 25: 235-246.
- Carrera EF, Matsumoto MH, Netto NA, et al. (2004) Fixation of greater tuberosity fractures. Arthroscopy 20: e109-111.
- Ji JH, Moon CY, Kim YY, et al. (2009) Arthroscopic fixation for a malunited greater tuberosity fracture using the suture-bridge technique: Technical report and literature review. Knee Surg Sports Traumatol Arthrosc 17: 1473-1476.
- Brais G, Ménard J, Mutch J, et al. (2015) Transosseous braided-tape and double-row fixations are better than tension band for avulsion-type greater tuberosity fractures. Injury 46: 1007-1012.
- Naggar L (2018) Surgical management of comminuted, displaced greater tuberosity fractures: A new technique of subacromial spacer on top of double-row suture anchor fixation. Joints 6: 211-214.
- Castagna A, Gumina S, Garofalo R, et al. (2019) Technique for a novel arthroscopic transosseous rotator cuff repair. Tech Shoulder Elb Surg 20: 12-18.
- Lee SU, Jeong C, Park IJ, et al. (2012) Arthroscopic fixation of displaced greater tuberosity fracture of the proximal humerus. Knee Surg Sports Traumatol Arthrosc 20: 378-380.
- Liu RW, Lam PH, Shepherd HM, et al. (2017) Tape versus suture in arthroscopic rotator cuff repair: Biomechanical analysis and assessment of failure rates at 6 months. Orthop J Sports Med 5.
- Chillemi C, Dei Giudici L, Mantovani M, et al. (2018) Rotator cuff failure after surgery: An all-arthroscopic transosseous approach. Musculoskelet Surg 102: 3-12.
Corresponding Author
Claudio Chillemi, MD, Department of Orthopaedic Surgery Istituto Chirurgico Ortopedico Traumatologico (I.C.O.T.), Latina, Italy, Tel: +3907736513213, Fax: +390773418261
Copyright
© 2020 Chillemi C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.