Massive Pulmonary Thromboembolism with Clot-in Transit in a Patient with Acute Aortic Dissection and Hemothorax- a Clinician's Dilemma
Abstract
Background: Acute aortic dissection with hemothorax is an uncommon presentation associated with high mortality and morbidity. They are at increased risk of venous thromboembolism. Massive pulmonary embolism with large clot-in transit has not been previously reported, and its management is not clear. We are reporting a case of massive PTE occurring after endovascular repair in a patient with acute aortic dissection and hemothorax.
Methods and results: We deployed a Valiant endovascular graft in descending thoracic aorta covering the origin of the left subclavian artery. Two days later, the patient developed sudden onset dyspnea and hypotension. Bedside echocardiography revealed large clot-in transit. We thrombolysed with streptokinase in view of massive PTE and large clot-in transit. The patient was discharged and doing well at three months follow up.
Conclusion: Management of massive pulmonary embolism after aortic dissection is challenging. However, systemic thrombolysis can be performed successfully after TEVAR. Appropriate anticoagulation and antiplatelet therapy are not clear in this setting.
Keywords
Pulmonary thromboembolism, Clot-in transit, Aortic dissection, Endovascular stent graft, Hemothorax
Introduction
Acute aortic dissection with hemothorax is an uncommon presentation associated with high morbidity and mortality [1]. These patients are also at increased risk of venous thromboembolism [2]. Massive pulmonary embolism (PTE) with large clot-in transit post-TEVAR was not reported previously, and it may be associated with life-threatening consequences and clinical dilemma [3]. Here, we describe a case of acute aortic dissection with hemothorax who developed massive pulmonary embolism with clot-in transit after successful thoracic endovascular repair (TEVAR). He was successfully managed by emergency thrombolysis. To the best of our knowledge, this is the first case to be reported with a similar presentation.
Case Presentation
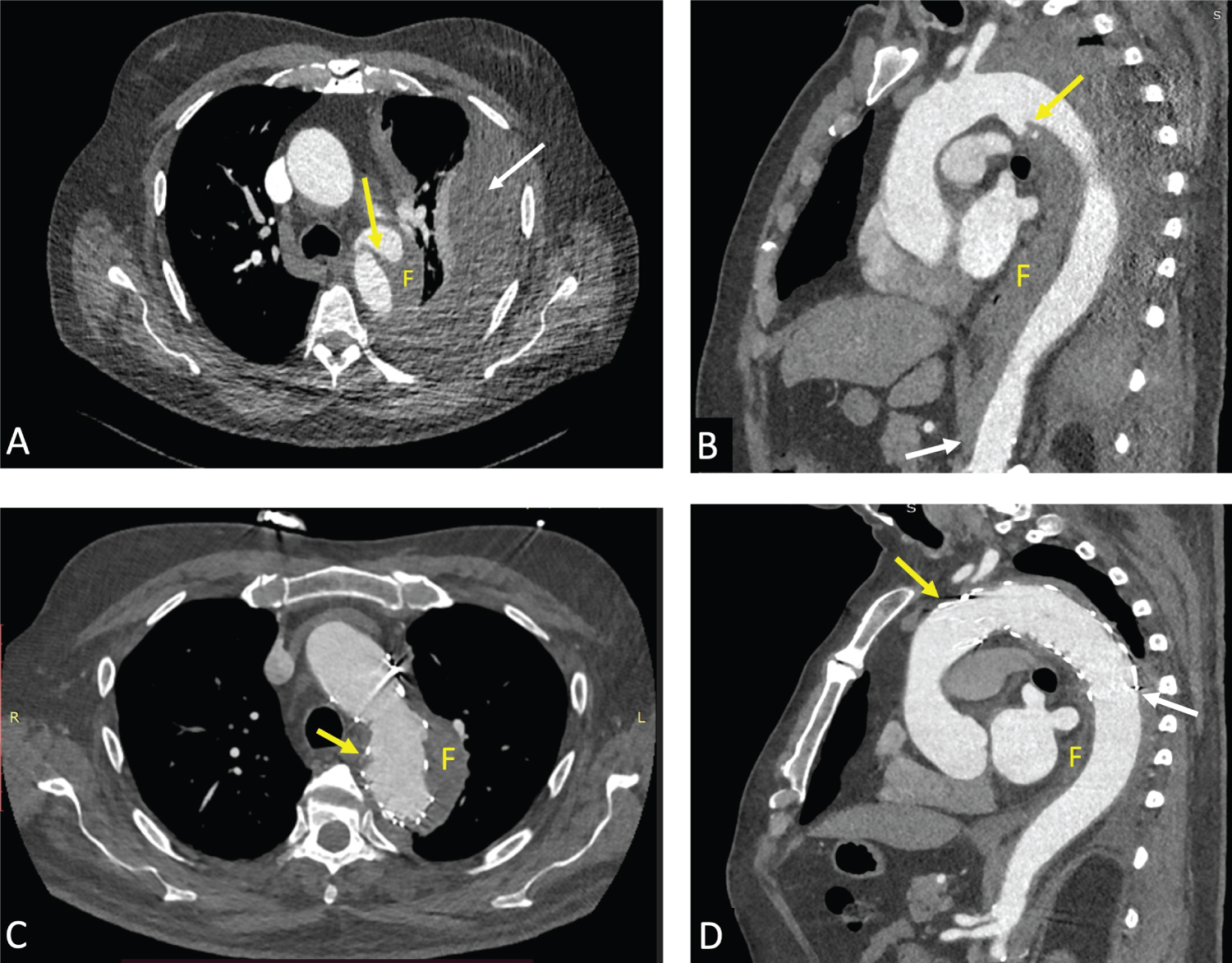
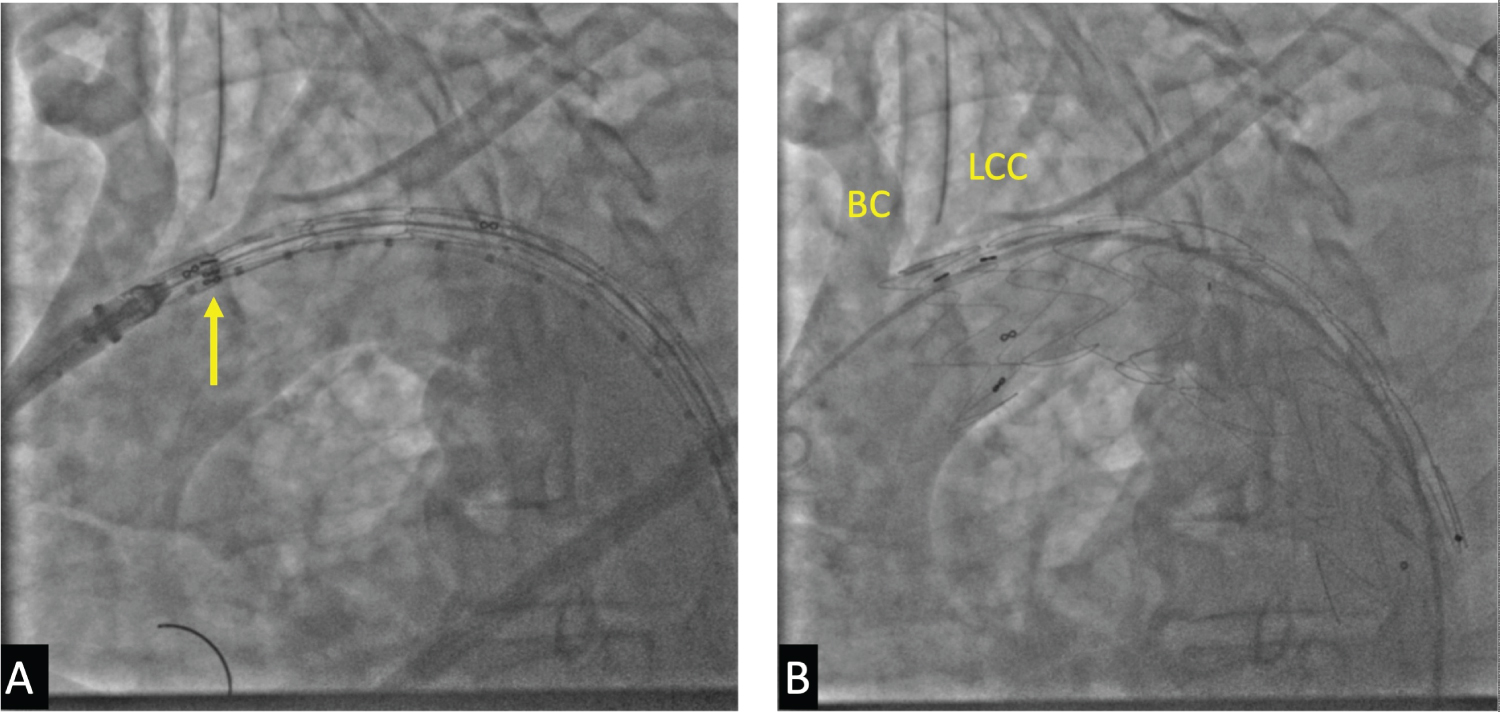
A 64-year-old gentleman with a history of hypertension presented to the emergency department with complaints of severe retrosternal chest pain radiating to the back along with dyspnea on exertion, which increased in the last ten days to modified medical research council class III. Respiratory system examination revealed decreased breath sounds in the left mammary, infra-axillary, scapular and infra-scapular region along with unilateral decreased chest expansion and dullness on percussion suggestive of large left pleural effusion. Cardiovascular system examination and rest of the systemic examination was normal. Chest X-ray confirmed large left-sided pleural effusion with ipsilateral lung collapse. Electrocardiogram and echocardiography were normal. Due to high suspicion of aortic dissection perforating into the left pleural cavity, computed tomography (CT) aortogram was performed. CT revealed Stanford type B aortic dissection starting just distal to left subclavian artery with dissection extending till just above the celiac artery. CT also revealed aneurysmal dilatation of the aorta of around 50 mm at the level of the false lumen and large left-sided hemothorax with underlying lung collapse (Figure 1A and Figure 1B). After the emergency heart team discussion, the patient was planned for thoracic endovascular aortic repair (TEVAR) under general anesthesia. The right femoral artery was accessed by cutdown for deploying endovascular graft, and the left femoral artery was used for pre and post-deployment aortic angiography. Aortic angiography revealed a dissection flap with entry point starting just distal to left subclavian artery extending till T11 vertebra. A 42 mm × 38 mm × 150 mm Valiant Captiva (MedtronicTM, Minnesota, USA) thoracic endograft was deployed with its proximal end positioned just distal to the left common carotid artery covering the origin of the left subclavian artery (Figure 2A). Post-deployment angiography revealed normal, brisk flow in the right brachiocephalic and left common carotid arteries with absent flow in the left subclavian artery (Figure 2B). The false lumen was sealed completely. After graft deployment, an intercostal drainage tube was inserted to drain the left hemothorax. The patient improved clinically and was extubated the following morning. He was doing fine and shifted to the step-down unit and mobilized. Two days later, he suddenly developed sudden onset dyspnea at rest, with hypotension and tachycardia. Possibility of graft failure versus acute pulmonary embolism was kept, and bedside echocardiography was performed, which revealed a highly mobile clot-in transit in the right atrium and right ventricle along with dilated and hypokinetic right ventricle (Video 1). Pulmonary thromboembolism occurred despite being on prophylactic anticoagulation. As the patient had massive PTE with hypotension, emergency rapid thrombolysis was performed with streptokinase 1.5 million units over 120 minutes and was then started on anticoagulation with enoxaparin at 1 mg/kg (80 mg every 12 hrly) after 6 hours. The patient's dyspnea and hemodynamics improved significantly over the next 24 hours. A repeat echo revealed the disappearance of RA and RV clots with mild right ventricular dysfunction and normal left ventricular function. Duplex ultrasonography of bilateral lower limbs was performed the next day, which didn't reveal any evidence of deep venous thrombosis. The drain from the left pleural cavity increased transiently, which decreased over the next 7 days, and ICTD was subsequently removed. After 5 days of enoxaparin, anticoagulation was changed to oral rivaroxaban 20 mg once daily along with 75 mg of clopidogrel. At 60 days follow up, echocardiography showed normal right ventricular pressures with no regional wall motion abnormalities and CT revealed thrombosed false lumen and no endoleak (Figure 1C and Figure 1D). The patient continues to do well at three months of follow up.
Discussion
Aortic dissection is an uncommon disease associated with hemothorax in less than 10% of cases and can be life-threatening [1]. Left-sided hemothorax is much more common than right-sided hemothorax [4]. Rupture of the false lumen into the pleural or pericardial cavity is a frequent cause of hypotension in aortic dissection and is associated with high mortality (> 50%) [1]. Our patient had dissecting aneurysm rupturing into the left pleural cavity and was temporarily closed by the tamponade effect of the large effusion. Management of hemothorax in acute aortic dissection is still debatable and is generally advised to drain after TEVAR [5]. For these reasons, we performed TEVAR followed by ICTD insertion. The procedure went successful, and the patient was given prophylactic anticoagulation, despite which he developed massive pulmonary thromboembolism with large clot-in transit. There is an increased risk of symptomatic pulmonary embolism after endovascular aortic repair, reported in up to 4% of patients [2,6]. In a retrospective analysis of 73 patients with endovascular aortic repair of aortic aneurysm, pulmonary embolism (asymptomatic and symptomatic) occurred in 12% of patients, associated with a mortality of 22% compared to 1.5% in those patients without pulmonary embolism [2]. Predictors of pulmonary embolism included ICU admission and chronic obstructive pulmonary disease (COPD). In a nationwide cohort study from Taiwan, aortic aneurysms were associated with a hazard ratio 1.88 (CI 1.52-2.33 p < 0.001) and 1.9 (CI 1.43-2.51, p < 0.001) for deep venous thrombosis and pulmonary embolism, respectively [7]. The possible increased risk for venous thromboembolism (VTE) may be related to ongoing inflammation with release of procoagulant factors, endothelial dysfunction, immobilization and mass effect due to compression of inferior vena cava in abdominal aneurysms [8]. However, there was no large data on the incidence of DVT or pulmonary embolism in patients with acute aortic dissection. We treated this patient with rapid systemic thrombolysis with streptokinase as the patient had hypotension and large clot-in transit. The other management options include catheter-directed thrombolysis, surgical embolectomy and transcatheter removal of the clot. The guidelines recommend systemic thrombolysis as first-line treatment in massive pulmonary embolism. However, there was not enough data to recommend an optimal mode of treatment in patients of pulmonary embolism post-TEVAR [9]. In a case reported by Gouran, et al. a 60-year-old man presented with sub-massive pulmonary embolism along with concomitant aortic dissection and hemothorax. He was managed by urgent TEVAR followed by therapeutic anticoagulation [10]. Similar cases with therapeutic anticoagulation were reported previously, but none presented with massive embolism, and hence none were thrombolysed [11,12]. Clot-in transit in pulmonary embolism is associated with mortality as high as 44% irrespective of hemodynamic status compared to 11-16% in those without clot-in transit [3] and highlight the need for a rapid institution of treatment. However, the optimal management is not clear. In a pooled analysis by Ganesh, et al. thrombolysis was associated with the lowest mortality (13.9%) followed by surgical thrombo-embolectomy (18.3%) and anticoagulation alone (37.1%) [13]. In our patient, clot-in transit was also associated with massive pulmonary embolism and hypotension; hence systemic thrombolysis was performed.
Conclusion
Massive pulmonary embolism has been rarely reported after acute aortic dissection, and its clinical management is challenging. However, massive PTE can be safely and successfully managed with emergency thrombolysis after TEVAR. Appropriate anticoagulant and antiplatelet regimen are still uncertain in this setting. Further are studies are needed to evaluate the optimal mode of treatment.
Author Contributions
Dinakar Bootla has contributed to the conception of the work, intervention, patient care, acquisition, and interpretation of data, drafting, reviewing, and editing the manuscript; Atit A Gawalkar has contributed to the conception of the work, intervention, patient care, acquisition, and interpretation of data, drafting, reviewing, and editing the manuscript; Pulkit Chhabra has contributed to the conception of the work, intervention, patient care, acquisition, and interpretation of data, drafting, reviewing, and editing the manuscript; Himanshu Gupta has contributed to the conception of the work, intervention, patient care, acquisition, and interpretation of data, drafting, reviewing, and editing the manuscript.
Acknowledgements
None.
Conflict of Interest
None to declare.
Funding
None.
Patient Consent
Written informed consent received by the patient for data and publication.
References
- Mccloy RM, Spittell JA, Mcgoon DC (1965) The prognosis in aortic dissection (dissecting aortic hematoma or aneurysm). Circulation 31: 665-669.
- Grobben RB, Frima C, Nathoe HM, et al. (2019) Pulmonary embolism after endovascular aortic repair, a retrospective cohort study. Eur J Vasc Endovasc Surg 57: 304-310.
- Torbicki A, Galié N, Covezzoli A, et al. (2003) Right heart thrombi in pulmonary embolism: Results from the international cooperative pulmonary embolism registry. J Am Coll Cardiol 41: 2245-2251.
- Chang JT, Lin YC (2019) Acute type B aortic dissection with right hemothorax. J Med Sci 39: 140-142.
- Piffaretti G, Menegolo M, Kahlberg A, et al. (2015) Hemothorax management after endovascular treatment for thoracic aortic rupture. Eur J Vasc Endovasc Surg 50: 608-613.
- Ramanan B, Gupta PK, Sundaram A, et al. (2013) In-hospital and postdischarge venous thromboembolism after vascular surgery. J Vasc Surg 57: 1589-1596.
- Lee FY, Chen WK, Chiu CH, et al. (2017) Increased risk of deep vein thrombosis and pulmonary thromboembolism in patients with aortic aneurysms: A nationwide cohort study. PLoS One 12: e0178587.
- Khashram M, Williman JA, Hider PN, et al. (2016) Systematic review and meta-analysis of factors influencing survival following abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg 51: 203-215.
- Konstantinides SV, Meyer G, Bueno H, et al. (2020) 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European respiratory society (ERS). Eur Heart J 41: 543-603.
- Gouran A, Safdari H, Pouraliakbar H, et al. (2020) Double Whammy: Concomitant acute type B aortic dissection and acute pulmonary embolism. Vasc Spec Int 36: 158-162.
- Al Zuabi S, Varkey AP, Abdalmaksoud SF, et al. (2013) A rare case of leaking thoracic aortic aneurysm in a patient with massive pulmonary embolism. Egypt J Intern Med 25: 47-50.
- Mitu O, Miftode R, Pintilie A, et al. (2019) Rare association of acute pulmonary embolism and type B aortic dissection: anticoagulant therapeutic dilemma. Romanian J Cardiol 29: 47-50.
- Athappan G, Sengodan P, Chacko P, et al. (2015) Comparative efficacy of different modalities for treatment of right heart thrombi in transit: A pooled analysis. Vasc Med (United Kingdom) 20: 131-138.
Corresponding Author
Himanshu Gupta, MD, DM, Department of Cardiology, Post Graduate Institute of Medical Education and Research, Chandigarh, Sector 12, 160 012, India, Tel: +91-172-275-6218
Copyright
© 2022 Bootla D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.