The Use of the Minimally Invasive APTOS Thread Method for the Treatment of Female Stress Urinary Incontinence: 3-year Follow-up Results
Abstract
To assess the long-term (3-year) follow-up of female stress urinary incontinence treatment using minimally invasive Aptos Thread method. 124 women with stress urinary incontinence confirmed by clinical and urodynamic evaluation were treated surgically using Aptos Thread method. Totally favourable results, including improvement (1) and cure (123) were recorded in all 124 patients. The improvement of quality of life, as well as total relief from all symptoms and the restoration of all adjacent organs involved in urodynamic disorders were observed.
Keywords
Stress urinary incontinence, Aptos Thread method
Introduction
Related to bladder and/or pelvic floor muscles dysfunction and defined as an involuntary leakage of urine [1,2], urinary incontinence (UI) impairs different aspects of quality of life [3,4] and is observable in different periods of life [5]. Both conservative [5,7] and surgical methods are applied for treatment [8-10].
Both non-invasive and invasive methods of treatment of urinary incontinence are offered. First are widely used on an initial stage of development, among which behavioural modification, pelvic floor exercises and other types of accessory teaching aids should be mentioned [11]. Second combine approaches like Anterior repair (Kelly Plication, a middle incision in the anterior vaginal wall, when endopelvic fascia is plicated at the level of bladder neck) [12], a transabdominal approach to vesicourethropexy [2], MMK urethropexy [13], Burch colposuspension [12], Neuromodulation [14], an injection of a sclerosing agents [15-18], and Tension-free vaginal tape (TVT-method) providing support for a sagging urethra by placing a mesh tape under it like a sling to keep it in its normal position (the common risks of TVT-surgery are injury to the bladder or urethra and difficulty urinating after surgery) [19,20].
In the mid-90s, the methods of minimally invasive aesthetic surgery were developed and applied successfully over last 25 years. Their main basis is formed by special threads with microscopic protections at an angle, as well as elastic spring threads. Original technologies of subcutaneous stitching and lifting of soft tissues have been proposed, allowing obtaining of high-quality, long-term lifting of face, neck, and body without incisions. During the last decade, the modifications of such threads are widely used in gynecology and urology.
Among modern approaches of minimally invasive techniques, the slings and periurethral injection of bulking agents should me mentioned. The use of local anesthesia and a low invasive nature, together with avoiding large incision and prolonged hospital stay, no risk of osteitis pubis and urethral obstruction, voiding difficulty, de novo detrusor over activity and genitourinary prolapse and the minimization of invasiveness determine the wide acceptance of newly developed technics, among which is the use of the minimally invasive APTOS thread method [21-23] for stress urinary incontinence (SUI). Being minimally invasive and done without incision, cicatrices and scares, vaginal lifting is a safe procedure followed by a short period of rehabilitation. With no risk of vaginal rupture and with active proliferation of connective tissue in the zone of correction, the successful use of the mentioned method in any age both in parous and nulliparous women is demonstrated.
We conducted a study of women with SUI to determine the long-term results and relief from symptoms together with the restoration of normal anatomical relationship of all adjacent organs in order to reach a favourable outcome - the lowest possible number of relapses and the significant improvement of quality of life.
Patients
One hundred twenty four women diagnosed with SUI and possessing diverse obstetric and gynaecological history - hysterectomy in the presence of concomitant uterine pathology (multiple uterine myoma, recurrent adenomyosis - 10 patients), cervical amputation (in the presence of concomitant pathology of the cervix - 11 patients), obesity (in the presence of concomitant pathology (hypertension, hypothyroidism - 8 patients), post-menopausal period - 35 patients, burdened obstetric history (I-II degree perineal tear, rapid labour, large foetus - 45 patients), and cysto-rectocele degree 1-2-15 patients - were selected for the study (Table 1).
Clinical Evaluation
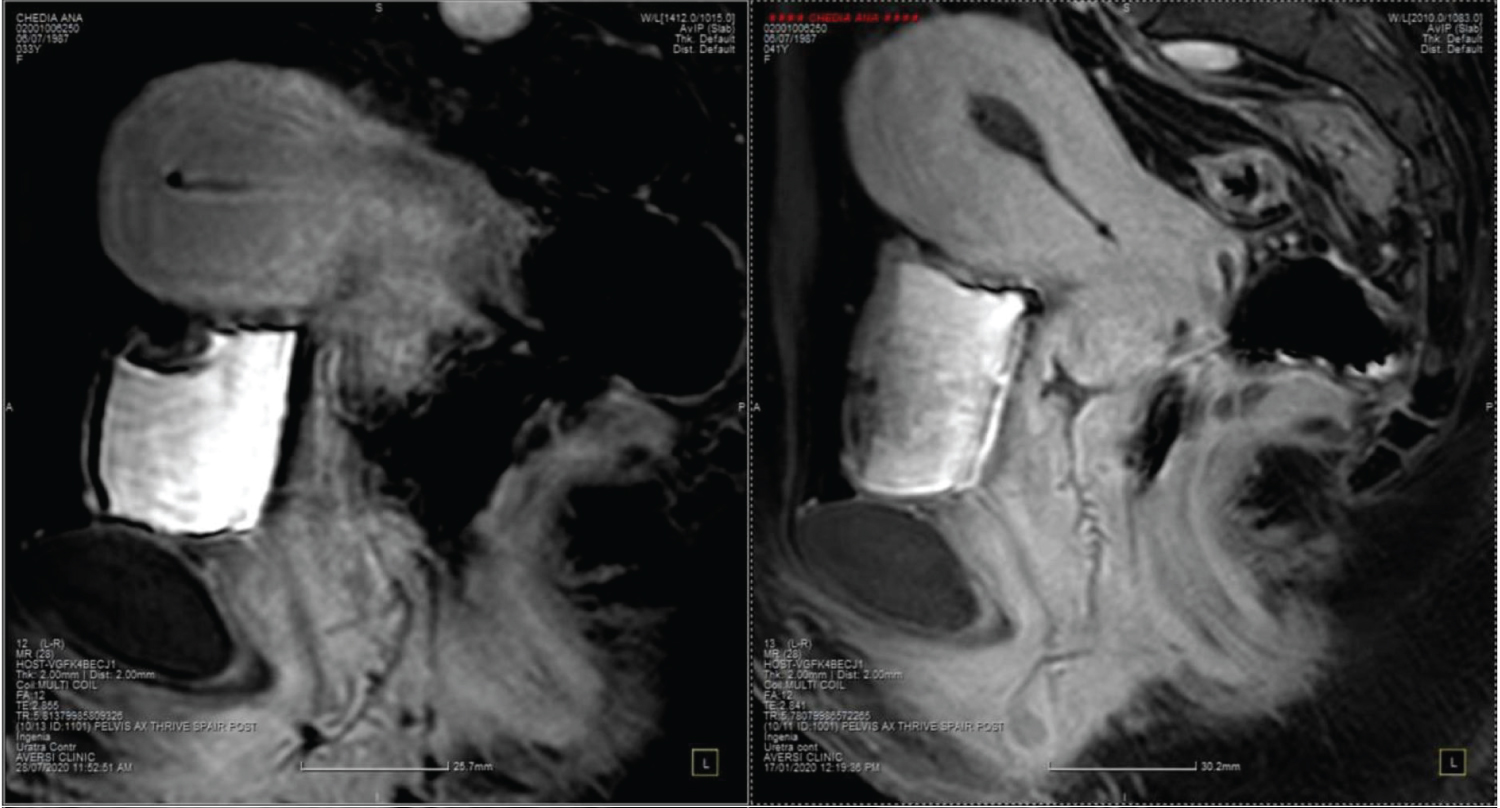
Both questionnaires and instrumental methods were used. Questions reflected different aspects of delivery, the presence of trauma during the childbirth, symptoms of SUI, and others (Table 2). Modern diagnostic methods, such as combined urodynamic examination and outpatient urodynamic monitoring, together with ultrasound examination with three-dimensional image reconstruction, MRI of small pelvis with contrast medium injection (Figure 1), common urine test, urine bacterial culture, speculum examination for assessing the vaginal walls condition, POPQ classification, PAD test - Q TIP test were performed.
All patients were socially active. Their majority complained of heaviness and discomfort in the perineal region - 25 patients, together with signs of SUI during physical activities such as fitness exercises, aerobics, running, jumping, and coughing - 40 patients. Less often, the patients were disturbed by colpoptosis - 33 patients, defecatory disorder - 5 patients, foreign body sensation in vagina - 3 patients, dyspareunia - 8 patients and frequent vaginal infections -10 patients (Table 3).
Intervention
Interventions were performed in the Department of Gynaecology of the private clinic Total Sharm in accordance with the modern standards of medical care of SUI.
Patients underwent minimally invasive treatment with Aptos threads between March 2018 and November 2021, in particular: 45 patients underwent vaginoplasty by minimally invasive thread lifting using Excellence intimate Method threads in combination with the Light lift spring Method - S (with strengthening of anterior vaginal wall and urethra). 39 patients underwent correction of only anterior wall (with urethra strengthening) via the combined Excellence intimate Method - Light Lift Spring Method - S, in 40 cases posterior and anterior vaginoplasty with perineoplasty by minimally invasive thread lifting via Excellence intimate Method - Light lift spring Method - S and light lift Needle 2G -S were performed.
Preparation of threads
The threads need to be prepared before implantation. Since the thread is pre-installed on the guide cannula and the spring is tightly wound around it, the thread winding is weakened on the guide cannula in the clockwise direction. After loosening the winding, it is necessary to check if the thread is loosened enough for the smooth implantation.
Implantation of threads
We use speculum examination to visualize the walls of the vagina, and we fix the anterior wall of the vagina with clamps. For the implantation of the thread, we make a puncture in previously made site under anaesthesia with an 18 G needle; we move down 0.5-1 cm from the external urethral orifice and begin to introduce the threads into the submucosal layer of the wall. The threads are implanted one at a time along the Light Lift Spring Soft- the combined Excellence intimate Method - first of all, a longer thread is implanted - secondly, a shorter one, and so, in turn, we fix and armour the urethra along the entire length along a straight trajectory to the bladder neck, capturing longitudinally and transversely located bundles of muscles. A tension vector is formed, and the urethra is fixed by armouring the layers of the vaginal wall. In the place prepared for the puncture, you will come out, release the end of the thread-spring from the guide cannula, remove it from the guide, pull the end of the thread from the puncture site by 2-3 spring rings and fix it. After the implantation, with the fingers of the second hand, fix the thread in the tissues, release the thread winding by moving it in reverse and in clockwise and counterclockwise directions and slowly withdraw the guide cannula from the tissues. Cut the ends of the implanted thread, burying the cut ends of the thread into the tissues. Implant the remaining number of thread-springs in the same way.
Comments
Vaginal threads Light Lift Spring Soft used in aesthetic gynaecology, literally create a framework against sagging tissues and tighten the vaginal walls, creating the additional support, due to it vaginal walls are tightened. Due to the fact that the correct position and the anatomical structure of the pelvic floor are reconstructed, the opening of the vaginal opening narrows; the walls of the vagina are tightened. The effect of rejuvenation of the intimate zone, the stimulation of the tissues’ own reserves are achieved through the formation of a fibrous capsule, the collagen fibres are formed in the places of implantation of the Light Lift Spring Soft threads, they literally envelop the threads, and a framework is created in the correction zone after the introduction of the vaginal threads Light Lift Spring Soft- the combined Excellence intimate Method - After the thread dissolves, the formed tissue scaffold will continue to maintain a lasting lifting effect. It is performed at any age, successfully applied to women who have given birth and who have not.
As it is demonstrated on Figure 1, before the operation, the walls of the urethra are vague, shapeless, the urethra is widened throughout and especially in its middle part, and the excretory opening is also widened, and has a form of triangle. The inter-urethra-vaginal space (wall) is of a loose consistency, the walls of the vagina are shapeless, the folds are less observed.
After the operation, the urethra has become narrower, with denser walls and a dense consistency of the inter-urethra-vaginal space, the walls of the vagina are dense, and the folds are clearly observed.
The picture (Picture 1) demonstrates the upper wall of the vagina, fixed with tools, a vaginal spectrum of the lower wall of the vagina is used for better visualization. To insert the threads into the upper wall of the vagina, 0.5 cm 1 cm below the external urethral hole, a single-entry point is made, through which a 5-6 cm long thread is implanted in the mucous layer of the upper wall of the vagina in combination with excellan intimate with light lift springs that allows the total volume and length of the vaginal wall to be fixed and raised.
Discussion
After the interventions and the 3-year follow-up period, the total relief from all symptoms, as well as the restoration of all adjacent organs involved in urodynamic disorders, together with the improvement of pelvic organs’ functionalities were observed. Based on the received data, we strongly recommend the use of minimally invasive thread method due to its lowest possible number of relapses and best functional results which significantly improve the quality of life of patients.
References
- Adile B, Gigliotta G, Caputo A, et al. (1996) Macroplastique im- plant for the treatment of type 3 stress urinary incontinence: 2-year follow-up. Proceedings of the International Continenee Society.
- (1992) Clinical practice guideline: Urinary incontinence in adults. Rockville, Md: Agency for health care policy and research, US Dept of Health and Human Services. AHCPR publication 92-0038.
- Ebbesen MH, Hunskaar S, Rortveit G, et al. (2013) Prevalence, incidence and remission of urinary incontinence in women: Longitudinal data from the Norwegian HUNT study (EPINCONT). BMC Urol 13: 27.
- Haylen BT, de Ridder D, Freeman RM, et al. (2009) An international urogynecological association (iuga)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21: 5-26.
- Henalla SM, Hall V, Duckett JR, et al. (2000) A multicentre evaluation of a new surgical technique for urethral bulking in the treatment of genuine stress incontinence. BJOG 107: 1035.
- Hunskaar S (2008) A systematic review of overweight and obesity as risk factors and targets for clinical intervention for urinary incontinence in women. Neurourol Urodyn 27: 749-757.
- Kiilholma P, Makinen J (1991) Disappointing effect of endoscopic Teflon injection for female stress incontinence. Eur Urol 20: 197-199.
- Novara G, Artibani W, Barber MD, et al. (2010) Updated systematic review and meta-analysis of the comparative data on colposuspensions, pubovaginal slings, and midurethral tapes in the surgical treatment of female stress urinary incontinence. Eur Urol 58: 218-238.
- Nunes Tamanini JT, D’Ancona CA, Tadini V, et al. (2003) Macroplastique implantation system for the treatment of female stress urinary incontinence. J Urol 169: 2229-2233.
- Sheriff MK, Foley S, McFarlane J, et al. (1997) Endoscopic correction of intractable stress incontinence with silicone micro-implants. Eur Urol 32: 284-288.
- Tomadze T, Stress urinary incontinence in women: A review [Forthcoming].
- Abrams P, Cardozo L, Khoury S, et al. (2002) Incontinence. (2nd edn), Plymouth, UK: Health Publication Ltd.
- Leong RK, de Wachter SGG, Joore M A, et al. (2010) Cost-effectiveness analysis of sacral neuromodulation and botulinum toxin A treatment for patients with idiopathic overactive bladder. BJU Int 108: 558-564.
- Lightner D, Diokno A, Synder J, et al. (2000) Study of Duras-pheret in the treatment of stress urinary in continence: A multi-center, double blind randomized, comparative study. J Urol 163: 166.
- Myers DL (2014) Female mixed urinary incontinence: A clinical review. JAMA 311: 2007-2014.
- Politano VA, Small MP, Harper JM, et al. (1974) Periurethral Teflon injection for urinary incontinence. J Urol 111: 180.
- Quackles R (1955) Deux incontinences apre`s adenomectomie gueries par injection de paraffine dans le perinee. Acta Urol Belg 23: 259-262.
- Ruby CM, Hanlon JT, Boudreau RM, et al. (2010) The effect of medication use on urinary incontinence in community-dwelling elderly women. J Am Geriatr Soc 58: 1715-1720.
- Wobig M, Dickhut A, Maier R, et al. (1998) Visco supplementation with Hylan G-F20: A 26 week-controlled trial of efficacy and safety in the osteoarthritic knee. Clin Ther 20: 410-423.
- Ogah J, Cody JD, Rogerson L (2009) Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev 4: CD006375.
- Richter HE, Albo ME, Zyczynski HM, et al. (2010) Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med 362: 2066-2076.
- Sulamanidze MA, Fournier PF, Paikidze TG, et al. (2002) Removal of facial soft tissue phtosis with special threads. Dermatol Surg 28: 367-371.
- Sulamanidze M, Sulamanidze G (2005) APTOS SPRING - a new concept of lifting. Aesthetn Surg J 42: 183.
Corresponding Author
M Tsivtsivadze, Clinic of Plastic and Aesthetic Surgery TOTALCharm, Georgia
Copyright
© 2022 Tomadze T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.