Complications of Gynecologic Surgery: Vaginal Cuff Dehiscence after Total Laparoscopic Radical Hysterectomy
Introduction
A 34-year-old woman G = 2 P = 2 completed parity was diagnosed with an abnormal PAP smear definite as AGC (Atypical Glandular Cells), seen in our center for a second opinion. The Bethesda system classifies atypical glandular cells (AGC) as glandular cells that demonstrate nuclear atypia appearing to exceed reactive or reparative changes but lacking certain features of adenocarcinoma. AGC occurs in approximately 0.18 to 0.74 percent of all cervical smears and AGC on cervical cytology is associated with premalignant or malignant disease in approximately 30 percent of cases [1,2].
On P/E a 3 cm exophytic tumor was seen on the anterior cervix; the biopsy was mandatory and evidenced an adenocarcinoma (adenosquamous type). This type represents 25 percent of all cervical cancers; this incidence of invasive cervical adenocarcinoma and its variants has increased dramatically over the past few decades [2,3]. The deepest invasion was more than 5 mm. The size of the cervical tumor was 3 cm; according to the American Joint Committee on Cancer (AJCC) tumor, node, metastasis (TNM) staging this case report fits IB1; > 5 mm in depth and ≤ 2 cm in greatest dimension; Consequently, the AJCC TNM staging update, AJCC version 9 TNM staging. The first chapter of version 9 AJCC TNM staging is the updated cervical cancer staging recently published; This article highlights the changes to the AJCC TNM cervical cancer staging; these changes align with the International Federation of Gynecology and Obstetrics staging; those changes are below:
T Category Changes
T1a, which previously depended on both the extent of horizontal spread and the depth of disease invasion, is now solely based on the depth of invasion. Unlike the depth of invasion, the extent of lateral spread is a less accurate measurement, can be recorded but would not count toward staging. Along the same lines, designating a microscopic disease as T1b is also based on a depth of invasion > 5 mm.
T1b has been divided into three subcategories, T1b1, T1b2, and T1b3, based on size (maximum diameter), which are ≤ 2 cm, > 2 to ≤ 4 cm, and > 4 cm, respectively. This division was informed by the consistent contribution of tumor size to prognosis. In this case, the diagnosis was T1b2 according to the AJCC TNM staging for cervical cancer (August 2021) [4].
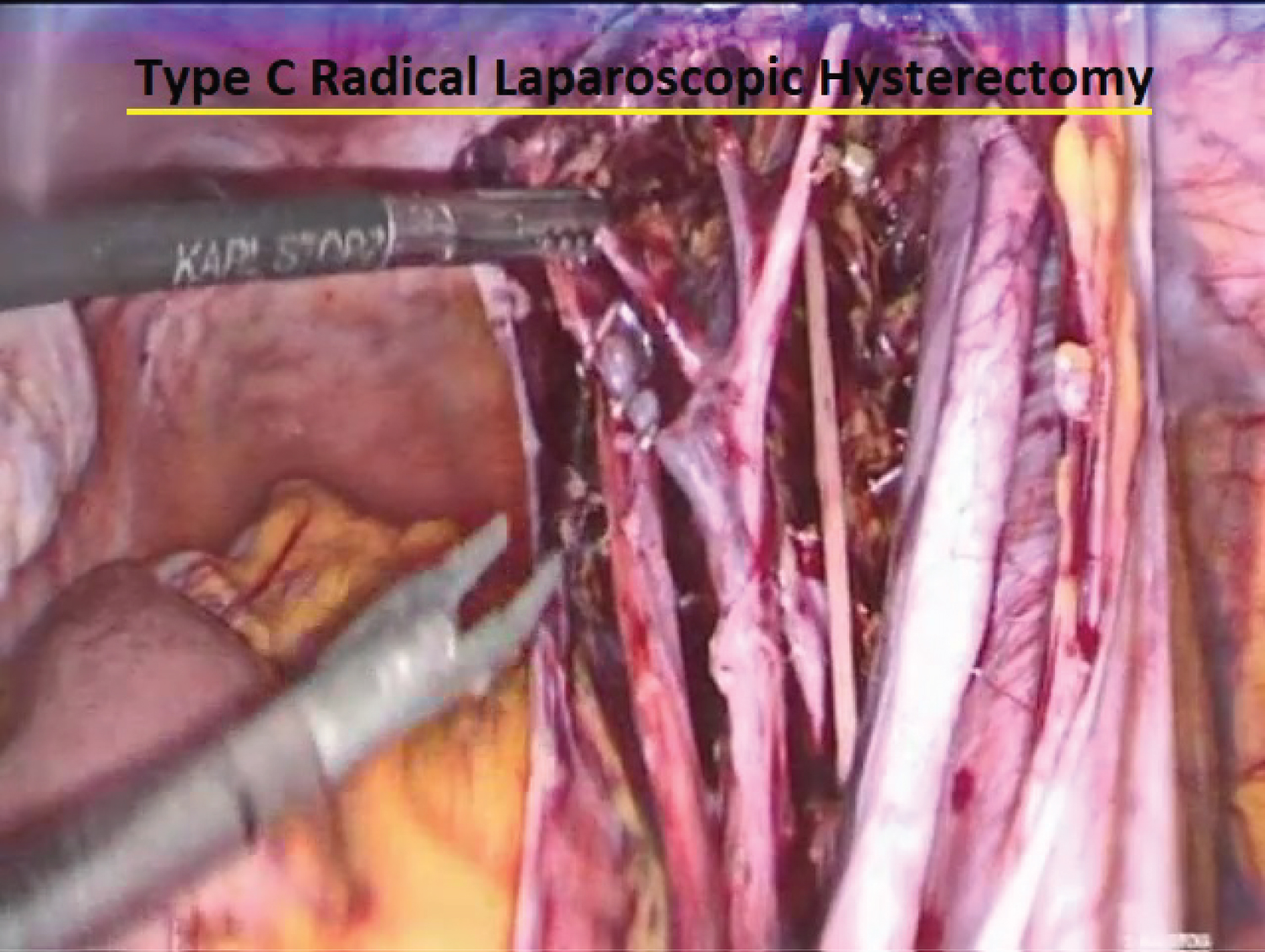
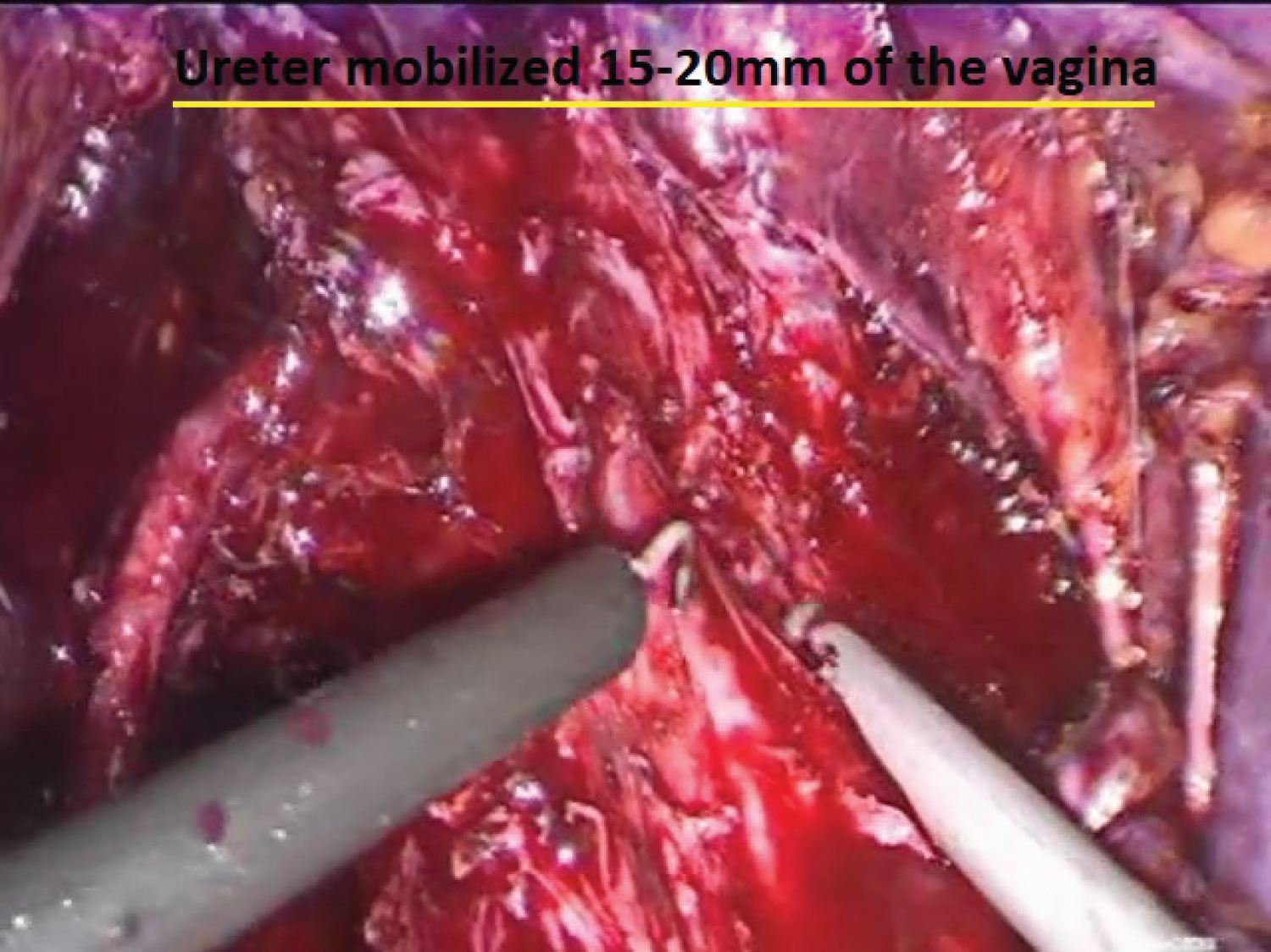
Given the information at this point, the patient was scheduled for a Total Radical Laparoscopic Hysterectomy (TRLH) for cervical cancer stage T1b2 with a total and radical pelvic lymphadenectomy. A Type C surgery was performed with a complete pelvic lymphadenectomy bilaterally (Figure 1); This type is transection of the uterosacral ligament at the rectum and vesicouterine ligament at the bladder (Figure 2). The ureter is mobilized completely 15-20 mm of the vagina from the tumor or cervix, and the corresponding paracolpos is resected routinely, depending on vaginal and paracervical extend and on surgeon choice [5]. In this case, the surgery went uneventfully and was done totally laparoscopically. The radical surgical stage was done, the lymph node dissection was performed, and it came back to be negative on histopathology. The final surgical stage was T1b2N0, she received adjuvant chemotherapy and 22 sessions of pelvic radiation.
Six months after the pelvic radiation treatment finished, she started with a heavy foul-smelling vaginal discharge and spotty bleeding after intercourse.
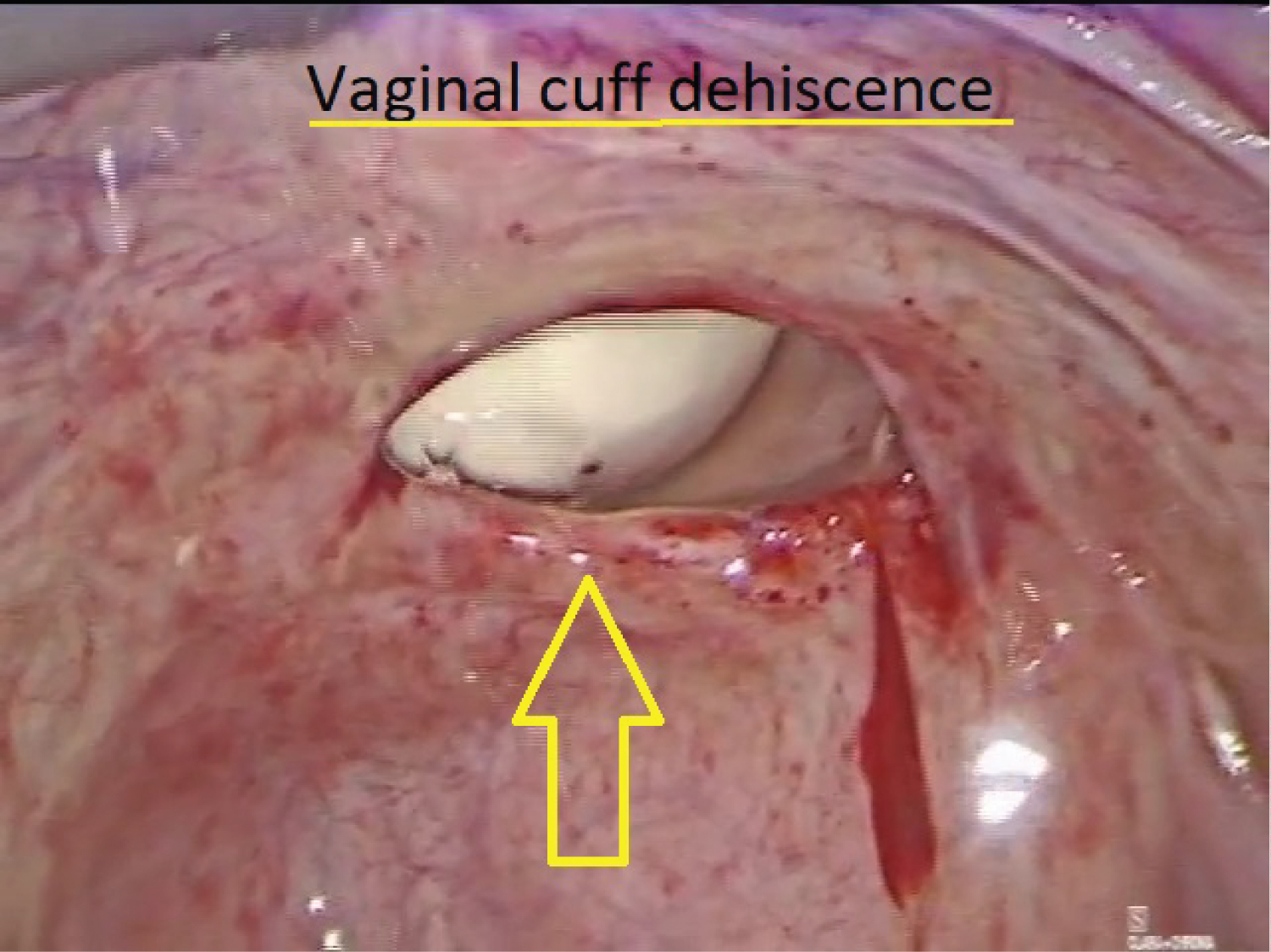
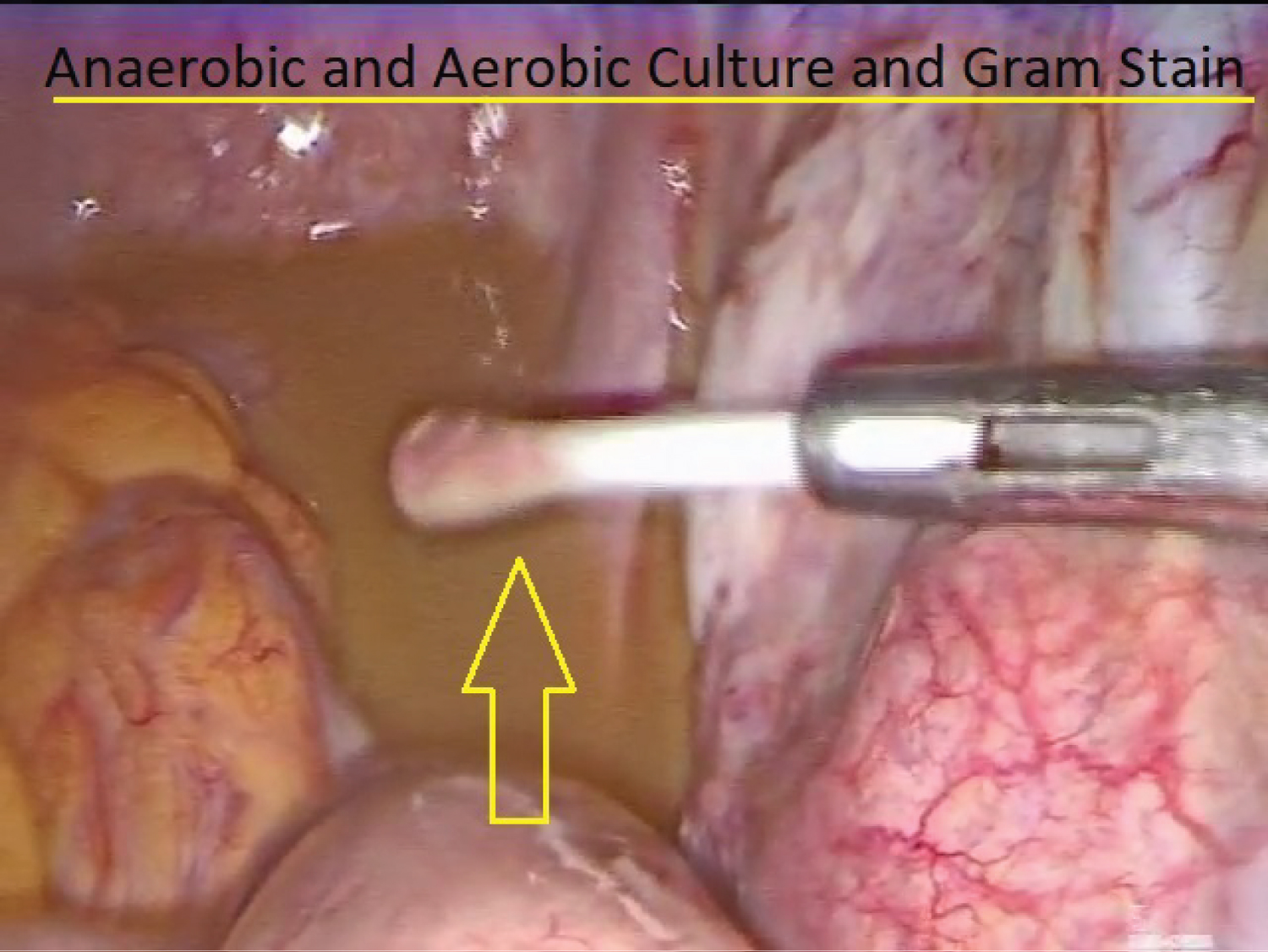
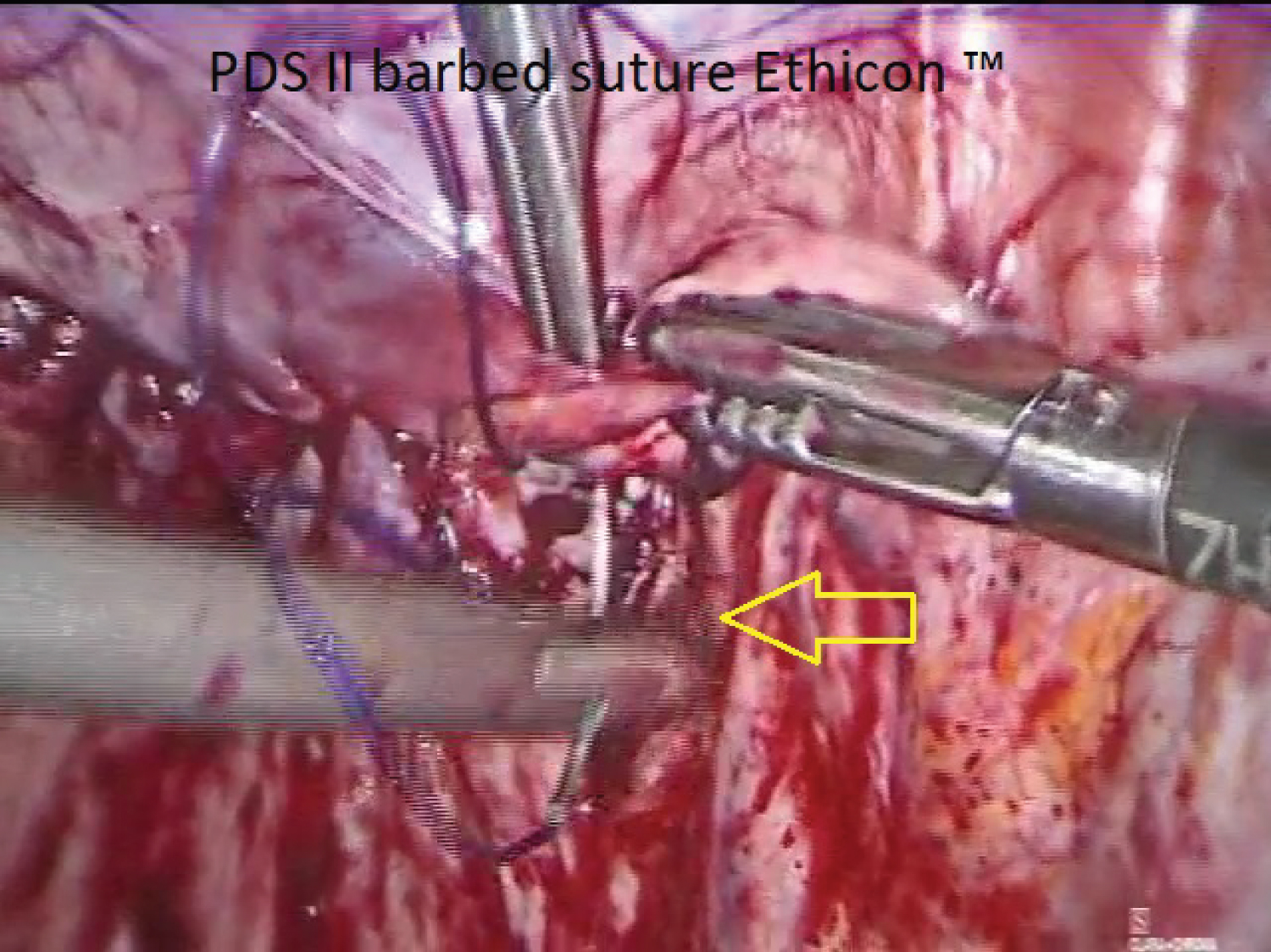
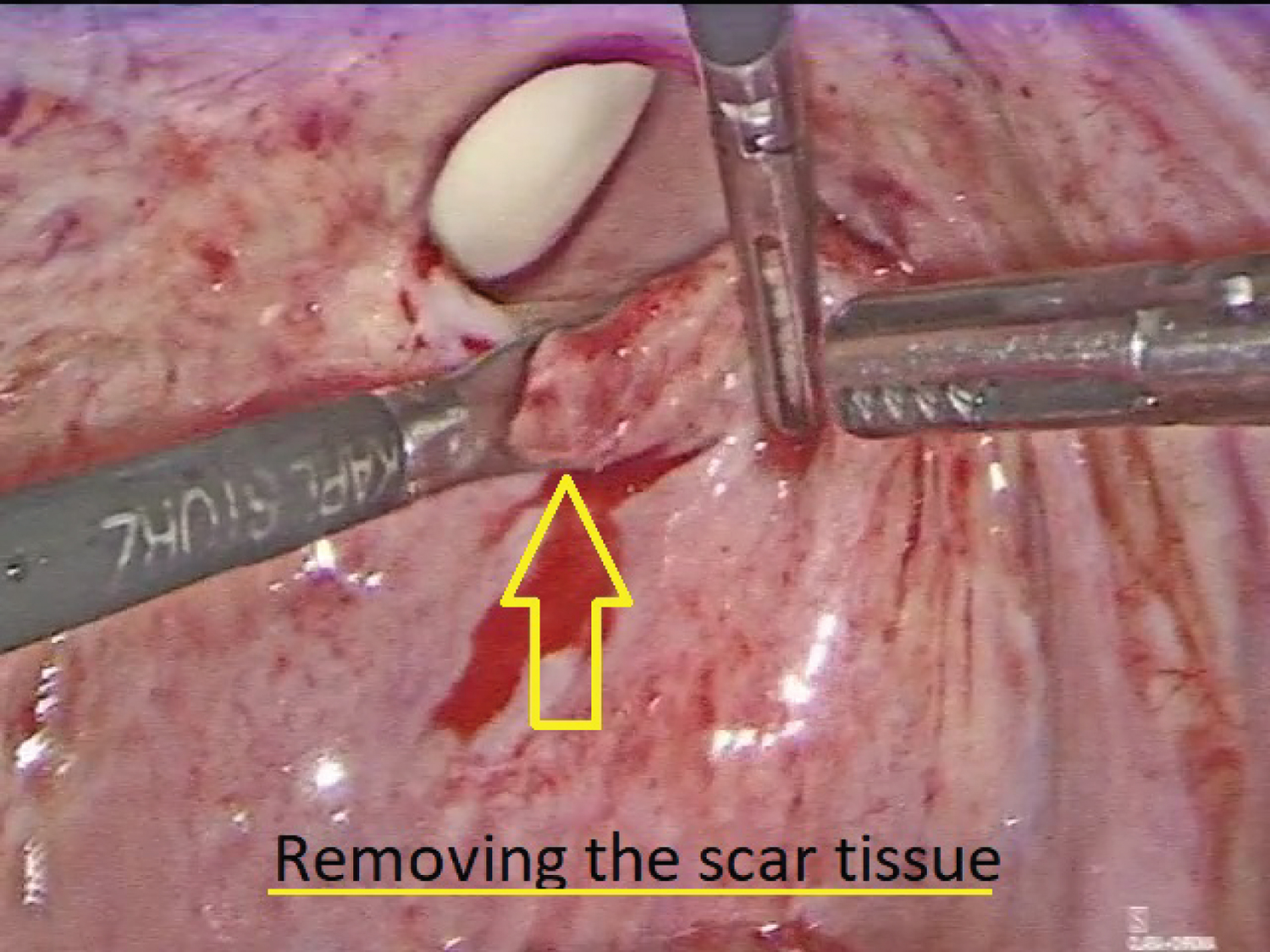
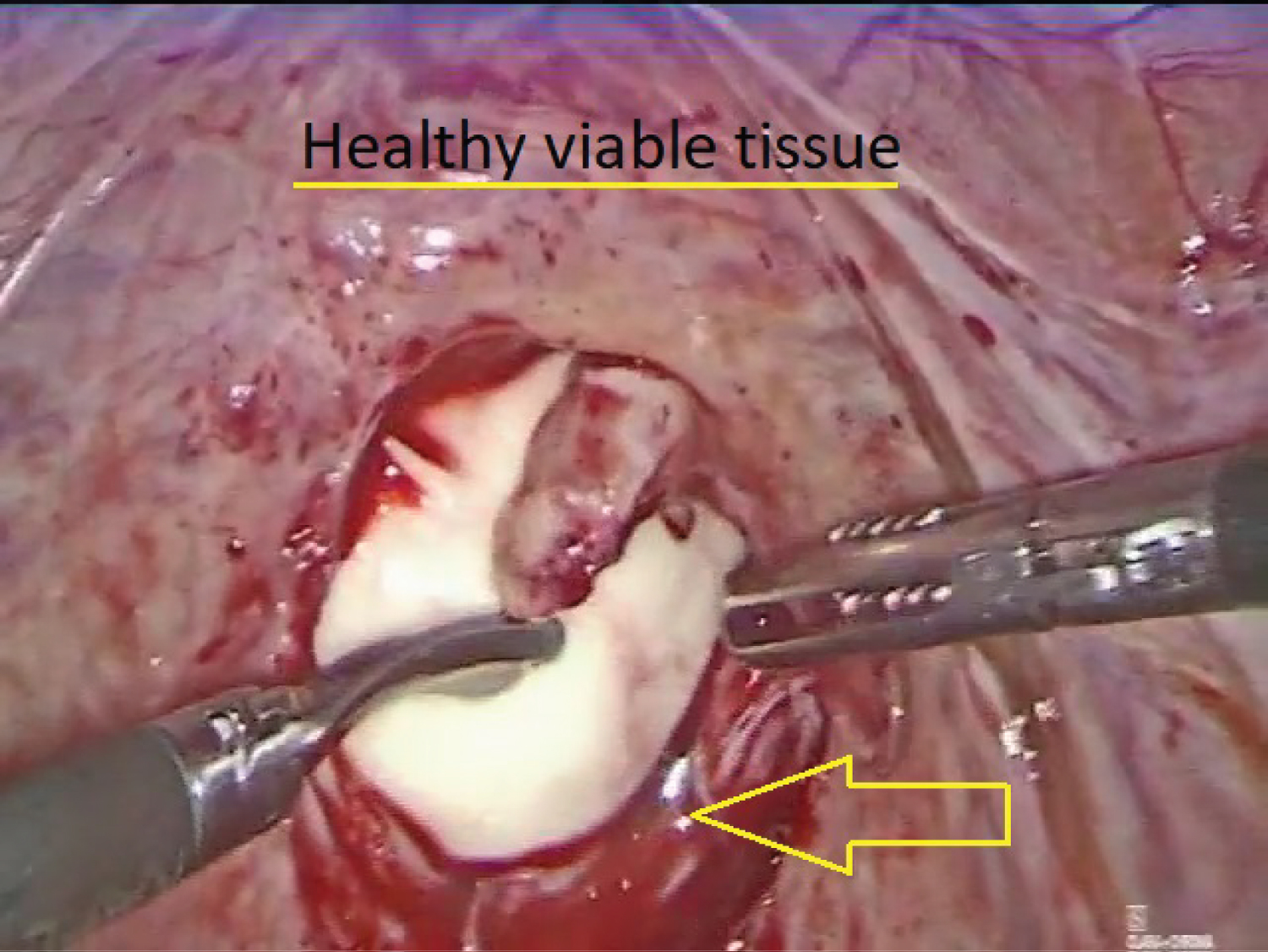
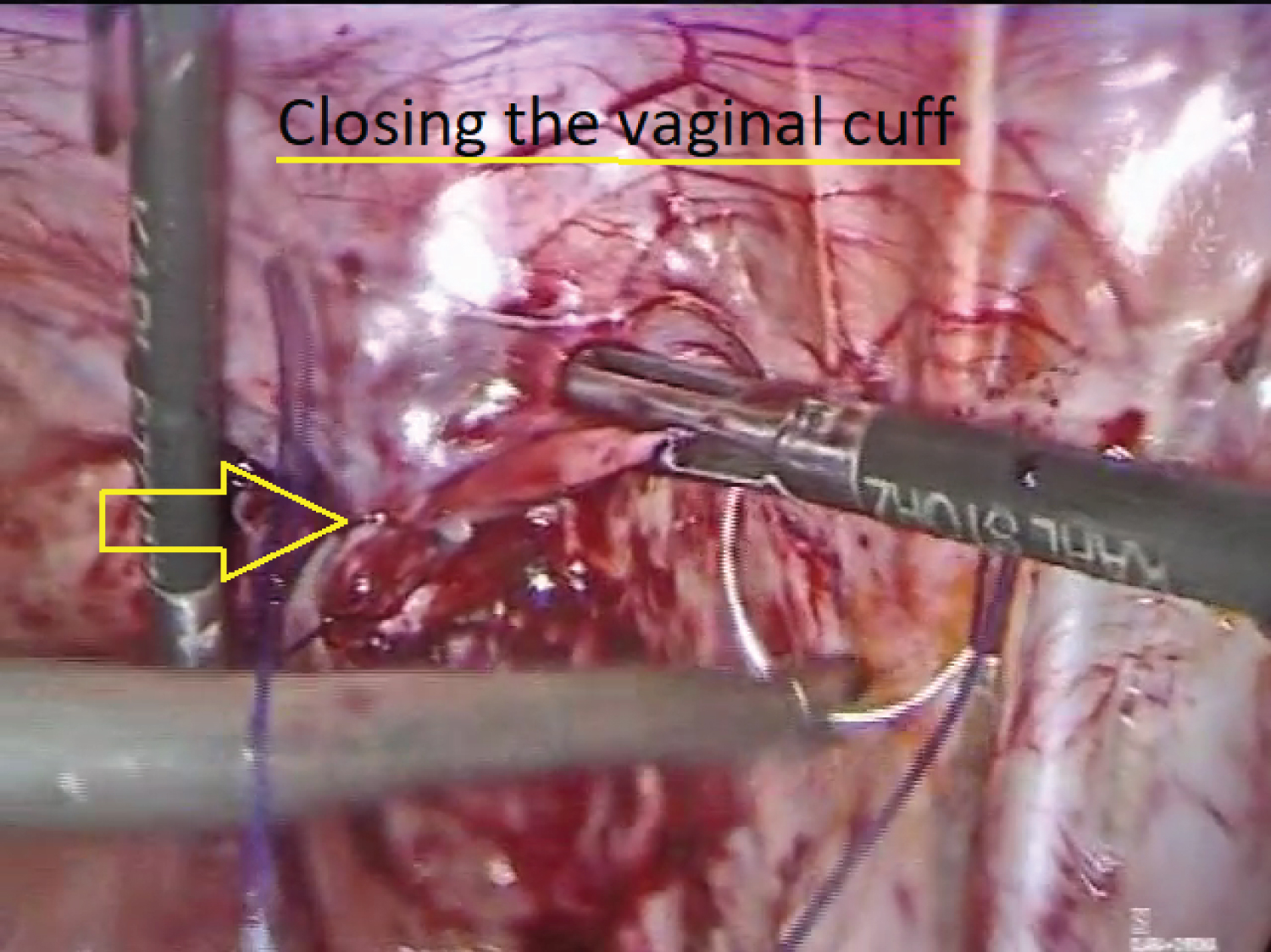
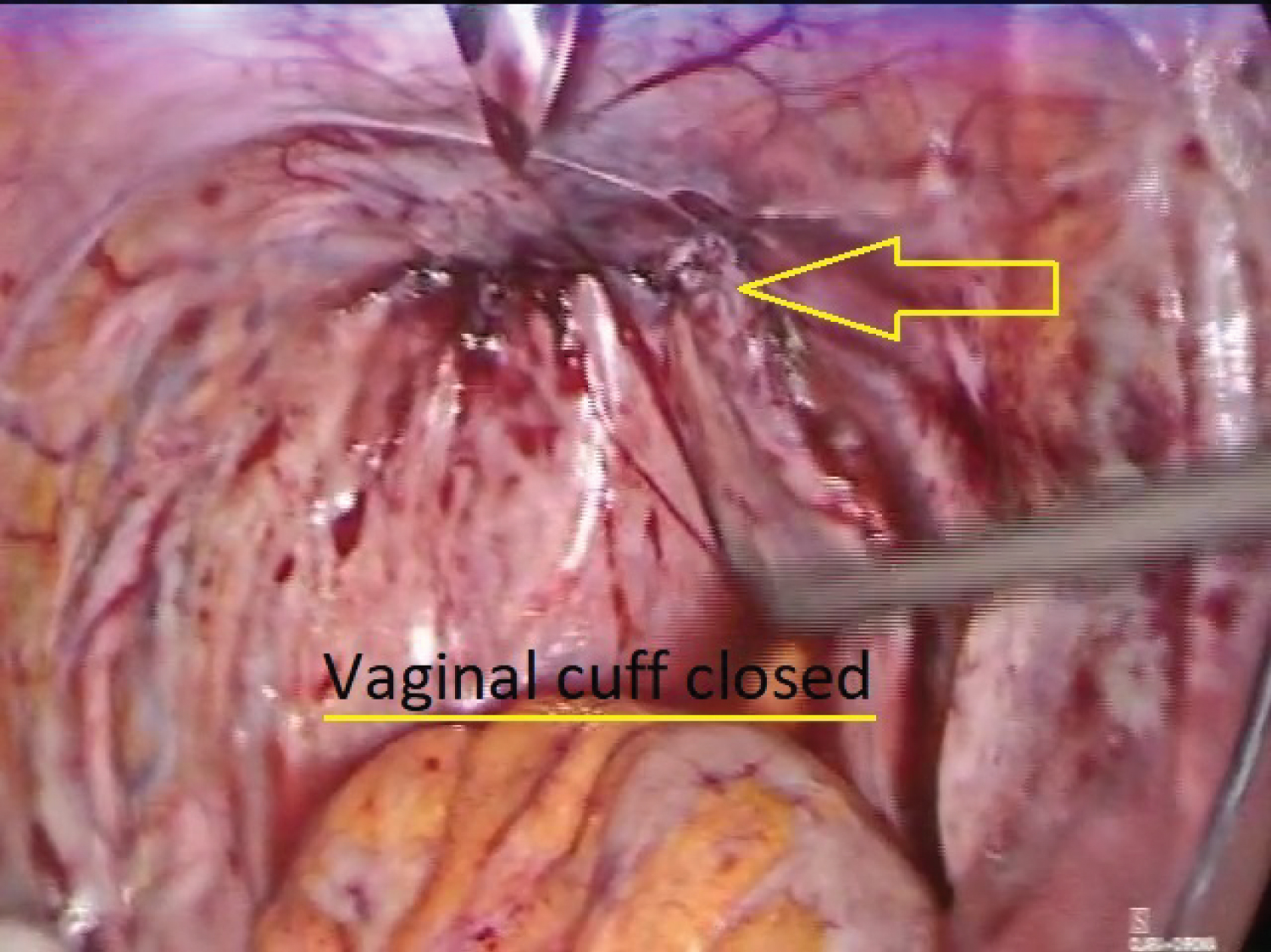
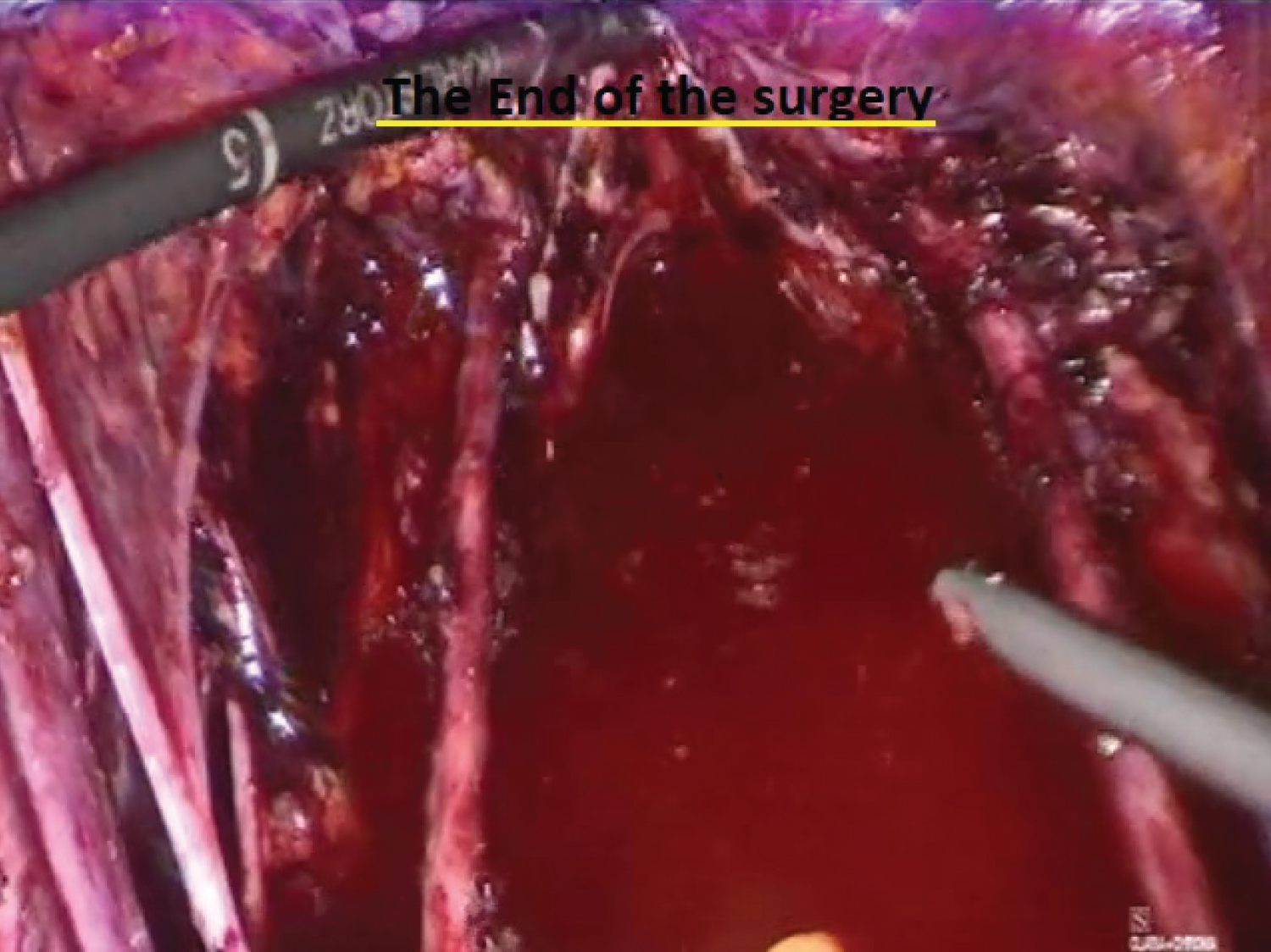
Complete vaginal cuff dehiscence without evisceration was diagnosed (Figure 3). Culture from the pelvic fluid was taken (Figure 4) Laparoscopic surgical repair was necessary (Figure 5). A barbed PDS II barbed suture (Ethicon™) suture was used. The laparoscopic surgery underwent without any complications; patient recovery was unremarkable.
Complete vaginal cuff dehiscence refers to the separation of the vaginal edges; Complete cuff dehiscence involves full-thickness separation of the entire length of the vaginal incision, whereas partial cuff dehiscence involves full-thickness separation of only a portion of the vaginal incision. Vaginal cuff dehiscence with evisceration indicates expulsion of intraperitoneal contents through the separated vaginal incision [6]. In this case, complete vaginal cuff dehiscence was diagnosed.
The incidence of dehiscence after a hysterectomy of 0.19 to 0.31 percent; The true incidence of vaginal cuff dehiscence after hysterectomy is challenging to determine since this complication is likely underreported [6,7].
The rate of vaginal cuff dehiscence is higher after total laparoscopic hysterectomy than an abdominal or vaginal total hysterectomy [8].
Pelvic radiation has been proposed but unproven as a risk factor; other factors can be smoking, sexual activity, estrogen status, vaginal hematoma, or infection [9].
Surgical repair is mandatory, removing the scar cuff tissue leaving healthy tissue, and sutured with PDS II or barbed suture Stratafix (Ethicon™) PDS 14 cm double needle [10].
Cultures for aerobic and anaerobic bacteria are recommended, and copious irrigation with iodine diluted with saline solution is mandatory before cuff closure [11].
There are no conclusive data to suggest one method of cuff closure is superior. Suture type, one- versus two-layer closures, and continuous versus interrupted sutures have all been studied with no specific conclusions [12].
Back in 2018, Ramirez P, et al. published in the New England Journal of Medicine an article comparing the two surgical techniques abording early-stage cervical cancer in a randomized clinical trial; Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer; The conclusion was that minimally invasive procedure has lower rates of survival vs. open surgery by 10.6% [13]. In this article, there is no mention about the surgeon's level of experience, not even the learning curve; given that to perform a radical hysterectomy laparoscopically or robotic needs more excellent experienced surgeons and extra training [14]; another factor is that this article was published in a non-surgical journal. This article has been hit the MIGS (Minimally Invasive Gynecologic Surgery) in cervical cancer in western countries.
There are different clinical trials like a systematic review and meta-analysis done by Tanitra Tantitamit Kuan-Gen Huang, et al. affirming the study suggesting that Laparoscopic Radical Hysterectomy was as safe and effective as open surgery in terms of survival outcomes [15]. Shailesh Puntambekar recently published Achieving Type C2 (Type III) Laparoscopic Radical Hysterectomy with Preservation of Nerves: A Possibility [16,17].
This type of surgery still being the first choice for the treatment of cervical cancer early stages in eastern countries.
In this case, the patient's recovery and health have been unremarkable until now.
This issue needs to be addressed, and new strong evidence needs to come up to have a better conclusion about the surgical technique to be used (Figure S1, Figure S2, Figure S3, Figure S4 and Figure S5).
Disclosure Statement
The authors declare that they have no conflicts of interest and nothing to disclose.
References
- (1989) The 1988 Bethesda System for reporting cervical/vaginal cytological diagnoses. National cancer institute workshop. JAMA 262: 931-934.
- Kurman RJ, Norris HJ, Wilkinson EJ (1992) Atlas of tumor pathology: Tumors of the cervix, vagina, and vulva. (3rd edn), Armed Forces Institute of Pathology. Washington
- Adegoke O, Kulasingam S, Virnig B (2012) Cervical cancer trends in the United States: A 35-year population-based analysis. J Women's Health (Larchmt) 21: 1031-1037.
- Olawaiye AB, Baker TP, Kay M, et al. (2021) The new (Version 9) American Joint Committee on Cancer tumor, node, metastasis staging for cervical cancer. A Cancer Journal for Clinicians 71: 287-298.
- Querleu D, Paul Morrow C (2008) Classification of radical hysterectomy. Lancet Oncol 9: 297-303.
- Iaco PD, Ceccaroni M, Alboni C, et al. (2006) Transvaginal evisceration after hysterectomy: Is vaginal cuff closure associated with a reduced risk? Eur J Obstet Gynecol Reprod Biol 125: 134-138.
- Hur HC, Donnellan N, Mansuria S, et al. (2011) Vaginal cuff dehiscence after different modes of hysterectomy. Obstet Gynecol 118: 794-801.
- Uccella S, Ceccaroni M, Cromi A, et al. (2012) Vaginal cuff dehiscence in a series of 12,398 hysterectomies: Effect of different types of colpotomy and vaginal closure. Obstet Gynecol 120: 516-523.
- Ala-Nissilä S, Laurikainen E, Mäkinen J, et al. (2019) Vaginal cuff dehiscence is observed in a higher rate after total laparoscopic hysterectomy compared with other types of hysterectomy. Acta Obstet Gynecol Scand 98: 44-50.
- Siedhoff MT, Yunker AC, Steege JF (2011) Decreased incidence of vaginal cuff dehiscence after laparoscopic closure with bidirectional barbed suture. J Minim Invasive Gynecol 18: 218-223.
- Agdi M, Al-Ghafri W, Antolin R, et al. (2009) Vaginal vault dehiscence after hysterectomy. J Minim Invasive Gynecol 16: 313-317.
- Ramirez PT, Klemer DP (2002) Vaginal evisceration after hysterectomy:A literature review. Obstet Gynecol Surv 57: 462-467.
- Ramirez PT, Frumovitz M, Pareja R, et al. (2018) Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med 379: 1895-1904.
- Park JY, Kim JH (2019) 1870 Comparison of laparoscopic versus open radical hysterectomy in early cervical cancer after completing learning curve and reducing intraperitoneal tumor exposure. J Minim. Invasive Gynecol 26: S225.
- Tantitamit T, Huang K-G, Lee C-L (2020) Laparoscopic versus open radical hysterectomy in women with early-stage cervical cancer: A systematic review and meta-analysis. Taiwan J Obstet Gynecol 59:481-488.
- Puntambekar S, Pattanaik S (2019) Achieving Type C2 (Type III) laparoscopic radical hysterectomy with preservation of nerves: A possibility. J Minim Invasive Gynecol 26: S1-S97.
- Nick AM, Lange J, Frumovitz M, et al. (2011) Rate of vaginal cuff separation following laparoscopic or robotic hysterectomy. Gynecol Oncol 120: 47-51.
Corresponding Author
Carlos Leal, MD, PhD, Department of Obstetrics and Gynecology, Division of Gynecologic Oncology, Universidad Autónoma de Chihuahua, Calle de La Llave #1419 suite 103 Colonia Centro, CP 31000, Mexico.
Copyright
© 2022 Leal C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.