Metastatic Melanoma: A Rare Cause of Gastrointestinal Intussusception under Nivolumab
Abstract
Background: Melanoma is a malignant tumor with a low 5-year survival rate. The small intestine is a privileged site for the development of metastases, which often cause intussusception and gastrointestinal bleeding. Nivolumab is a monoclonal antibody that has produced higher response rates than other chemotherapeutics.
Case presentation: A 52-year-old patient with a positive history of melanoma who had been previously treated with surgical excision and then received nivolumab is discussed. The patient subsequently showed gastrointestinal symptoms and underwent urgent surgery for intussusception.
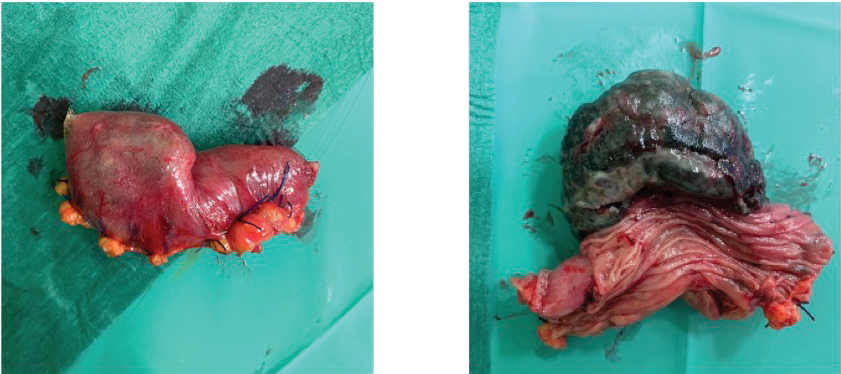
The operative piece showed a mass that was positive for melan A and suggestive of melanoma metastasis.
Conclusion: Intestinal intussusception after nivolumab is rare and requires early diagnosis and emergency surgery to yield a good prognosis.
Background
Malignant melanoma (MM) accounts for 1% to 3% of all cancers [1], and it usually has a poor prognosis with an estimated 5-year survival rate of approximately 10% [2]. Gastrointestinal (GI) metastasis from cutaneous melanoma is found in about 60% of patients in autopsies studies [3] with the small bowel being the most commonly affected site of the gastrointestinal tract (GIT).
Intestinal intussusception is a very rare condition in adults, accounting for 5% of all-cause intussusceptions [4]. Tumors are the main cause of adult intussusceptions, and metastatic malignant melanoma being responsible for about 15% of cases [5]. Intestinal melanoma is usually asymptomatic with persistent non-specific abdominal pain, anemia of unknown origin, GI bleeding, and intestinal obstruction as the most common symptoms when present. Intestinal intussusception is an unusual presentation of metastatic MM with very few reported cases in literature.
Nivolumab is an immune check-point inhibitor that has been approved for the treatment of metastatic MM. It acts by blocking the interaction between programmed death 1/programmed death ligand 1 (PD1/PD1L) and has been demonstrated to be superior to conventional chemotherapies in terms of overall survival and objective response rates [6].
As far as we know, only two cases of MM spreading to the GIT and presenting as intestinal intussusception during Nivolumab therapy have been reported in the literature [7].
We present a case report of an intestinal intussusception secondary to small bowel metastasis of cutaneous melanoma during Nivolumab therapy.
Case Presentation
A 52-year-old male patient was admitted to the gastroenterology department for new-onset anemia (Hb 8.8 gr/dL) and change in bowel habits, and mild diffuse abdominal pain. His previous medical history was positive for cutaneous melanoma of the right trunk that was treated by surgical excision in March 2019 (Clark level III, 7 mm Breslow thickness and presence of ulceration). Axillary lymphadenectomy was also performed and revealed the presence of 2/26 positive lymph nodes. The patient was subsequently treated by immunotherapy with the anti-PD1 monoclonal antibody Nivolumab (last infusion in May 2020). His family history was positive for breast cancer (mother) and ovarian cancer (aunt).
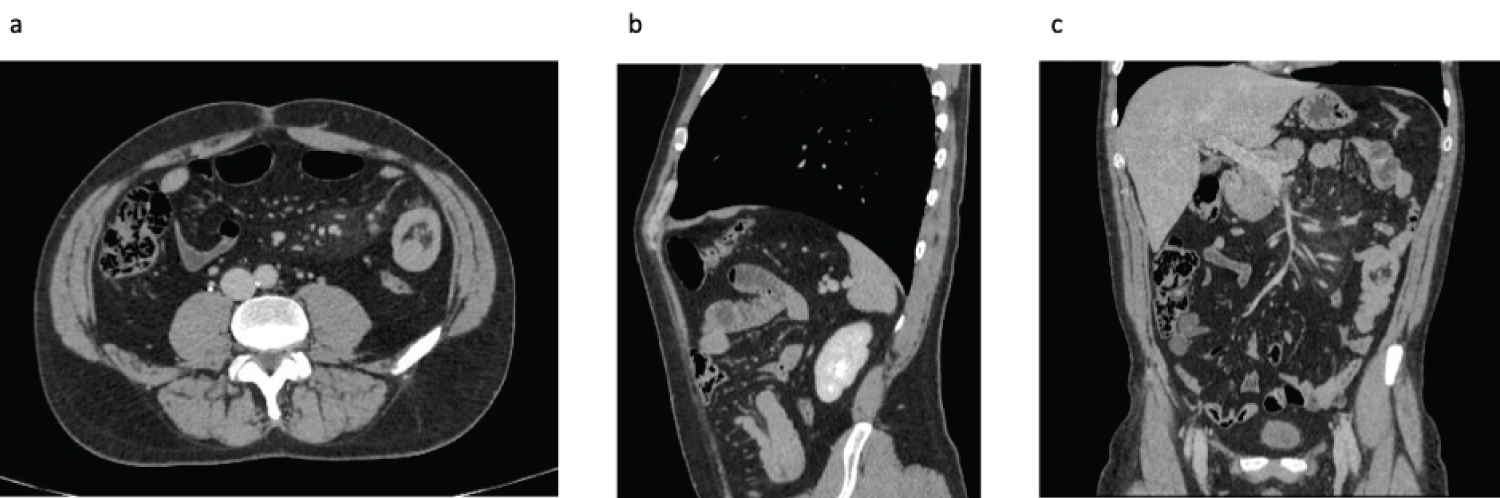
Symptoms first appeared in April 2020, when the patient complained of a change in stool consistency, but no alterations in the number of bowel movements, abdominal pain, nausea, or vomiting were reported. Fecal occult blood test was negative. Given the positive oncological history, further investigation through a total body computed tomography (CT) scan was performed in June 2020 and revealed results that were suspicious for intussusception (Figure 1 a-c).
In July 2020, he presented to the emergency department for new-onset anemia (Hb 8.8 gr/ dL) and was admitted to the Gastroenterology Department. At the time of admission, physical examination showed abdominal distension, mild tenderness, and pain upon palpation. Fecal occult blood test was positive. Abdominal ultrasound revealed congested and targeted appearance of a small intestinal loop, associated with inhomogeneity of the surrounding adipose tissue (findings suggestive of intussusception on a secondary basis). Therefore, he was transferred to the colorectal surgery department and underwent emergency laparoscopic surgery on July 23rd, 2020.
Surgery
Pneumoperitoneum induction was performed using Verres needle inserted into the left hypochondrium. A 12 mm optical trocar was then inserted in the right paraumbilical line, and two other median 12 mm optical trocars were inserted in the epigastrium and hypogastrium. The loops of the small intestine were explored; intussusception was detected at about 150 cm from Treitz muscle. Upstream intestinal loops were dilated. A median mini laparotomy was then performed after which the invaginated portion of the intestine was externalized. We proceeded with resection of the invaginated intestinal tract and with packaging of the an isoperistaltic lateral-lateral mechanical anastomosis. Upon the opening of the surgical piece, the tumor presented as a 6 cm dark-colored intraluminal mass with a polypoid appearance.
Histopathology
Histopathological examination of a 7 cm ileal intestinal tract was conducted (Figure 2). The serosa presented as a gray, smooth, shiny surface. A black ulcerated polypoid mass of 55 × 32 × 30 mm was present 35 mm from the surgical margin with a diffuse infiltration of the gut wall. Immunohistochemistry was then performed and showed positivity for Melan A, Melanosome HBM45, S100, CD117, and c-Kit.
Outcome and follow-up
In the postoperative period, the patient had not complications and was discharged on the sixth postoperative day. The follow-up at 12 months did not show disease recurrence.
Discussion
Malignant melanoma is a very aggressive tumor, characterized by a high metastatic capacity and a poor prognosis. It is the extraintestinal malignancy with the highest risk of metastasis to the GIT. Remarkably, about 50% to 60% of affected patients present bowel metastasis as indicated by autopsy reports [8]. Interestingly, only 1%-4% of these are diagnosed before a patient's death, mostly because patients with metastatic intestinal melanoma are usually asymptomatic [5]. Metastases from cutaneous MM usually spread through the bloodstream, and this transfer could easily explain why metastatic lesions are found much more frequently in the small intestine (71%-91% of cases), which is characterized by higher blood supply, while the large intestine represents the least affected site at 22%-26% of cases [9]. Interestingly, the predilection of cutaneous melanoma for metastatic implants in the small intestine has been recently attributed to the CCR9-CCL25 axis [10]. In contrast, melanomas originating primarily from the GIT are rare entities; indeed, most intestinal melanomas are considered to metastasize from primary occult cutaneous neoplasms, either not identified by conventional methods or spontaneously regressed [11]. Recognized risk factors for MM spread to the GIT include a primary tumor characterized by regression, ulceration and high mitotic rate, Clark level III or higher, and superficial spreading melanoma [8,12].
Common complaints related to intestinal metastasis include persistent abdominal pain, nausea, and vomiting, which are the most common clinical presentations followed by intestinal obstruction or intussusception (1/3 of cases) in addition to GI bleeding or anemia of unknown origin in about 26% of cases [13].
Intussusception is a rare condition in adults, accounting for 5% of all-cause intussusceptions and causing 1%-5% of intestinal obstructions [14]. In contrast to pediatric intussusception, which is usually idiopathic, small bowel intussusception in adults shields a neoplastic cause in 65% of cases [5] with malignant tumors accounting for 20% of the cases; 50% are of primary origin, and 50% are metastatic [15]. The clinical presentation is usually characterized by intestinal obstruction, persistent abdominal pain, nausea, vomiting, and/or GI bleeding/anemia [16]. Small bowel intussusception caused by metastatic MM as leading point has rarely been reported in literature. The final diagnosis is usually made-intra-operatively although many available imaging techniques could raise the suspicion of GIT neoplasm. Among these, abdominal ultrasound, which is fast and easy to perform, may reveal a "target", "doughnut", or "bull's eye" sign. Capsule endoscopy could be an adjunctive valuable tool, providing that obstruction has been previously excluded. However, a computed tomography (CT) scan remains the preferred imaging modality despite having a sensitivity of only 60% with respect to detecting small bowel metastasis [17].
Surgical treatment of small bowel intussusception is currently considered standard-of-care. Notably, surgical resection of the affected segment is only palliative and not curative, it prevents further complications and it is effective in prolonging remission and survival rates. Indeed, a median overall survival of 64 months has been reported assuming that R0 was achieved [18].
In the last 10 years, only 36 cases of bowel intussusceptions caused by metastatic MM have been reported in literature of which only two cases occurred during concurrent Nivolumab therapy, and all of them required surgical treatment.
Conclusion
This case describes a rare condition, an intestinal symptomatic intussusception from melanoma metastasis, which is an unusual presentation.
In the scientific literature, only two other similar cases involving patients with a similar clinical picture and the same diagnosis who were being treated with Nivolumab have been published.
An early diagnosis based on laboratory results, such as occult blood test, a complete blood count, and instrumental tests (ultrasound and/or CT) in the suspicion of intestinal metastases and a surgical consultation to determine the best possible short and long-term outcome for the patient is extremely important.
References
- Lens M, Bataille V, Krivokapic Z (2009) Melanoma of the small intestine. Lancet Oncol 10: 516-521.
- Ishihara K, Saida T, Otsuka F, et al. (2008) Statistical profiles of malignant melanoma and other skin cancers in Japan: 2007 update. Int J Clin Oncol 13: 33-41.
- Branum GD, Seigler HF (1991) Role of surgical intervention in the management of intestinal metastases from malignant melanoma. Am J Surg 162: 428-431.
- Barussaud M, Regenet N, Briennon X, et al. (2006) Clinical spectrum and surgical approach of adult intussusceptions: A multicentric study. Int J Colorectal Dis 21: 834-839.
- Agha FP (1986) Intussusception in adults. AJR Am J Roentgenol 146: 527-531.
- Yun S, Vincelette ND, Green MR, et al. (2016) Targeting immune checkpoints in unresectable metastatic cutaneous melanoma: a systematic review and meta-analysis of anti-CTLA-4 and anti-PD-1 agents trials. Cancer Med 7: 1481-1491.
- Miyazawa H, Yanagi T, Yamaguchi Y, et al. (2017) Two cases of melanomas paradoxically metastasizing to the intestinal tract during nivolumab therapy. J Dermatol 44: 959-962.
- Schuchter LM, Green R, Fraker D (2000) Primary and metastatic diseases in malignant melanoma of the gastrointestinal tract. Curr Opin Oncol 12: 181-185.
- López RG, Santomé PM, Porto EI, et al. (2011) Intestinal perforation due to cutaneous malignant melanoma mestastatic implants. Rev Esp Enferm Dig 103: 386-388.
- Krige JE, Nel PN, Hudson DA (1996) Surgical treatment of metastatic melanoma of the small bowel. Am Surg 62: 658-663.
- Aktas A, Hos G, Topaloglu S, et al. (2010) Metastatic cutaneous melanoma presented with ileal invagination: Report of a case. Ulus Travma Acil Cerrahi Derg 16: 469-472.
- Liang KV, Sanderson SO, Nowakowski GS, et al. (2006) Metastatic Malignant Melanoma of the Gastrointestinal Tract. Mayo Clin Proc 81: 511-516.
- A K, Ek F, Je K, et al. (1991) CT of malignant melanoma: Patterns of small bowel and mesenteric involvement. J Comput Assist Tomogr 15: 570-574.
- Azar T, Berger DL (1997) Adult intussusception. Ann Surg 226: 134-138.
- Chiang JM, Lin YS (2008) Tumor spectrum of adult intussusception. J Surg Oncol 98: 444-447.
- Ghaderi H, Jafarian A, Aminian A, et al. (2010) Clinical presentations, diagnosis and treatment of adult intussusception, a 20 years survey. Int J Surg 8: 318-320.
- Goldstein HM, Beydoun MT, Dodd GD (1977) Radiologic spectrum of melanoma metastatic to the gastrointestinal tract. AJR Am J Roentgenol 129: 605-612.
- Deutsch GB, Flaherty DC, Kirchoff DD, et al. (2017) Association of surgical treatment, systemic therapy, and survival in patients with abdominal visceral melanoma metastases, 1965-2014: Relevance of surgical cure in the era of modern systemic therapy. JAMA Surg 152: 672-678.
Corresponding Author
Simona Deidda, MD, Department of Surgical Science, University of Cagliari, Monserrato, S.S. 554 Bivio Sestu, Cagliari 09042, Italy.
Copyright
© 2022 Deidda S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.