Minimally Invasive Dacryocystorhinostomy
Introduction
Primary Acquired Nasolacrimal duct obstruction (PANDO) is not an uncommon clinical condition to come across in clinical practice and is more common in females.
Secondary causes of nasolacrimal duct obstruction can be divided into infectious, traumatic, neoplastic, inflammatory, iatrogenic and idiopathic. Nasolacrimal duct block is the main cause of dacryocystitis.
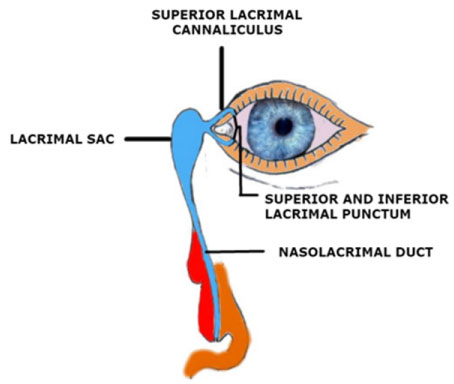
Complications can arise if and when dacryocystitis is not treated well in time for a long time and such a situation decreases the chances of a successful outcome of any surgical intervention (Figure 1).
The basic aim of dacryocystorhinostomy (DCR) is to make a bypass channel to deal with an obstruction in the nasolacrimal duct passage. There are multiple ways and approaches to perform dacryocystorhinostomy. External dacryocystorhinostomy carries a very high success rate, but is potentially invasive, is to be done usually under general anesthesia and can cause an ugly scar on the face. Laser assisted dacryocystorhinostomy carries a less favorable outcome in terms of long term success while endoscopic nasal approach of performing a DCR is dependent on a skillful ENT surgeon as well and, an outcome usually less favorable compared to external DCR.
In view of this we need to have an alternate technique of performing lacrimal duct by-pass surgery which should be efficient in terms of the outcome, can be performed under local anesthesia safely without running the risk of complications of general anesthesia and any compromise on the outcome and aesthetic aspect of this surgical procedure.
Keeping the above facts in mind, I developed this technique which appears to be safe, effective and economically a viable option to try before considering more invasive approach. The surgery can be done under topical and local anesthesia. Patient is well explained regarding the diagnosis, basic details about the procedure, advantages, likely events during the surgery and required/expected cooperation.
Indications
Primary and secondary acquired nasolacrimal duct obstruction (where applicable) in adults is the main indication of performing this procedure especially when epiphora is interfering with the daily living activities of a patient.
When there is a complete or partial obstruction of the nasolacrimal duct causing epiphora, it may cause skin excoriation, visual impairment, social embarrassment, chronic ocular discharge and acute or chronic dacryocystitis. Less common indications include facial nerve palsy and gustatory lacrimation (crocodile tears). In the presence of lacrimal duct obstruction, this lacrimal drainage bypass procedure is mandatory prior to any intraocular surgery like cataract, because of the higher risk of post-operative endophthalmitis.
Contraindications
Thick lacrimal bone is usually difficult to perforate with the trephine and enlarging that opening by trephine nibbling is also not easy to proceed with. In view of this patients with thick lacrimal bone should be excluded as candidate for this procedure. In more than 60% of patients lacrimal bone is about 100 micron thick, which is fairly easy to deal with by this technique.
More than 300 microns thickness of the lacrimal bone should not be operated with this technique as perforating the thick lacrimal bone is not easy with the lacrimal trephine.
Bleeding disorders can cause severe and serious bleeding in the nose which may not be easy to control and manage without the help of an ENT consultant. It is recommended that such patients should not be operated upon with this technique, till the time this bleeding disorder is well managed before planning surgery.
Nasal pathology causing epiphora must be treated at its own merit as in some cases conditions like nasal poly can cause epiphora.
Anatomical abnormality in the nasolacrimal passage is also a contraindication and it needs to be evaluated before planning this procedure. This can be diagnosed with the help of dacryocystography beforehand.
Acute infection in the nasolacrimal passage needs to be managed preoperatively.
Presurgical Evaluation
Successful outcome of the surgery depends upon the proper evaluation to determine the exact cause of epiphora and site of obstruction in the nasolacrimal passage.
History regarding use of topical medications, radiation, trauma, chemotherapy, chemical/thermal burn, infections like trachoma, herpes simplex/zoster, systemic diseases like diabetes, hypertension, bleeding disorders must be clearly documented in the presurgical evaluation.
Females are more prone for PANDO due to the anatomical difference in the nasolacrimal passage and hormonal changes around menopause, to develop primary acquired nasolacrimal duct block as a result of involutional stenosis of the nasolacrimal duct.
ENT consultation must be sought to rule out any nasal pathology as the likely cause of epiphora.
Ascertaining the location of nasolacrimal duct block is an important aspect of presurgical evaluation as it decides the course and safety of surgical planning.
Any other cause for lacrimation and epiphora must be evaluated in detail so that appropriate planning for the surgical intervention should be carried out.
Possible choice of anesthesia must also be evaluated as some patients are apprehensive about the general anesthesia, while others are fearful about being awake during the surgery under local anesthesia.
Thickness of the lacrimal bone should always be evaluated with the help of CT scan. We must understand that patients with thick lacrimal bone are usually not suitable candidates for this surgical option. Lacrimal bone is a thin plate of lamellar bone and, in more than 70% of patients, is 100-300 micron in thickness. Patients with lacrimal bone thicker than this are not a suitable for this procedure. In view of this on the average about 70-80% of cases can be offered this treatment option. Maximum documented thickness of lacrimal bone is 722 micron which is very uncommon. About 67% cases have a lacrimal bone which is 100 micron or less than this.
Consent & Counselling
Complete information about the indication, advantages, steps of the procedure and limitations of the surgical procedure needs to be discussed with the patient along with any explanations of the relevant questions asked by the patient. Risk of all possible complications must be carefully discussed along with setting realistic expectations out of this surgical procedure before surgery is a very important aspect to be given due consideration. Patient should be given enough time to think and raise any concerns. All the details must be recorded and documented for all medicolegal reasons and future reference.
Investigation
Performing relevant investigations is very valuable in making the proper management plan preoperatively in order to have a higher success rate of this procedure.
It is very important to perform the relevant laboratory investigations like complete blood picture, bleeding time, clotting time, screening for hepatitis, HIV and other required tests along with radiological investigations like dacryocystography, X-ray of the lacrimal passage area and CT Scan for the thickness of the lacrimal bone, any extension of air sinuses in the lacrimal bone and any pathology in and around the nasolacrimal passage.
Presurgical preparation
Start with systemic antibiotic in case if there is evidence of dacryocystitis. In case if there is no active infection then before the starting the procedure I usually give a broad spectrum IV antibiotic to prevent any possible post-operative infection. Nose is packed with the guaze soaked in lignocaine with adrenaline to avoid the risk of bleeding from the nose.
Surgical technique
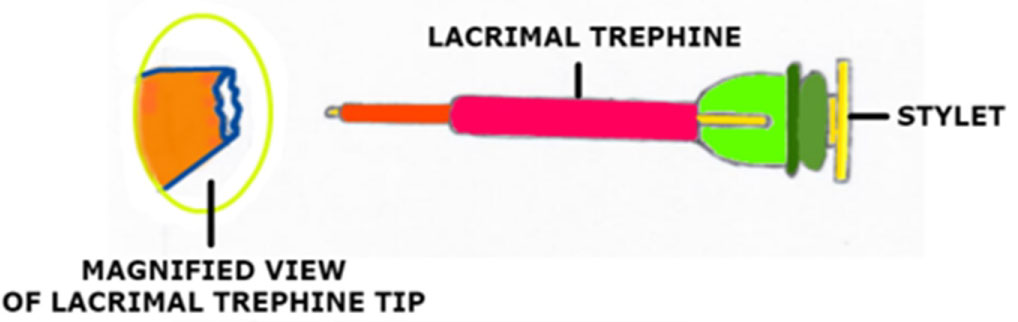
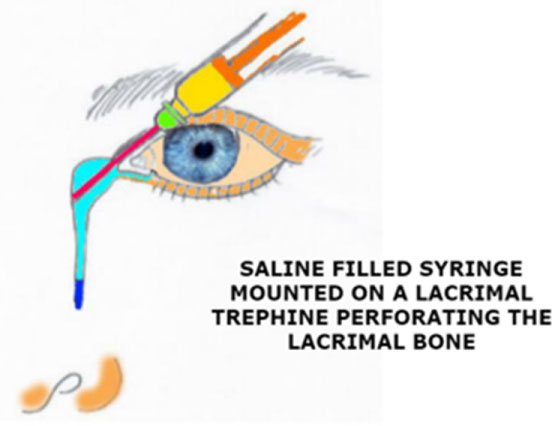
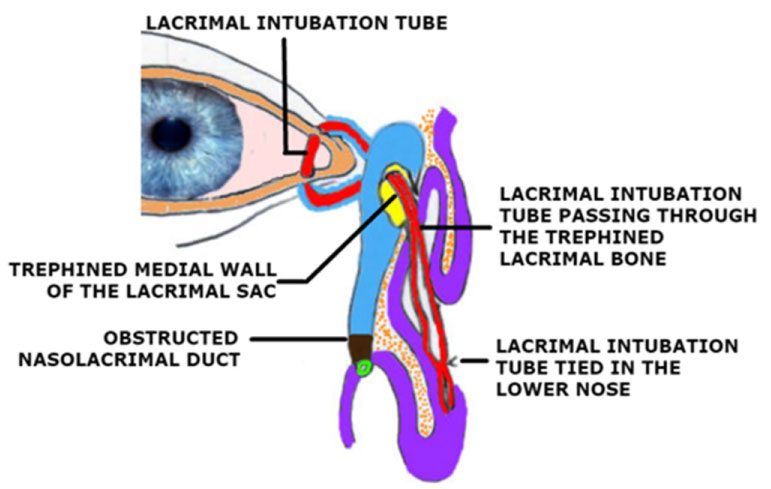
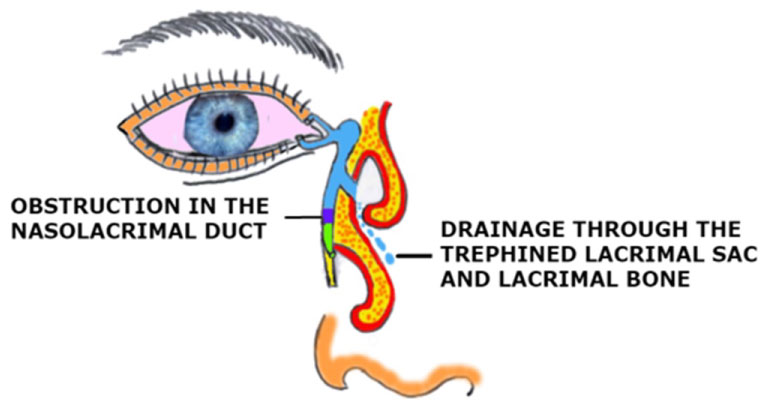
Topical anesthesia eye drops are instilled followed by instilling 2 drops of 5% Povidone Iodine in the conjunctival sac. Surgical field is cleaned with 10% Povidone Iodine. Patient is prepared and draped well before proceeding with the surgery. Conjuctival sac is irrigated with sterile saline. Superior lacrimal punctum is dilated with a lacrimal punctum dilator. Then I irrigate the lacrimal passage with lignocaine 1% before this ensure that nose is packed very well. I wait for 2 minutes so that local anesthesia effect is picked well on the nasal mucosa and lacrimal passage. Following this a dispersive viscoelastic is irrigated in the lacrimal passage to inflate. Following this a Lacrimal Trephine with stylet is passed till its tip touches the medial, inferior and posterior wall of the lacrimal sac (Figure 2).
At this moment the stylet is withdrawn and a 5 cc syringe with sterile saline is attached to the hub of the lacrimal trephine without retracting the tip of the trephine. Then the syringe is directed inferiorly, posteriorly and medially and rotated to perforate the lacrimal bone. Loss of resistance indicates the successful perforation of the lacrimal sac, lacrimal bone, then this primary opening is enlarged by nibbling the bone around the primary opening. After this irrigation of the normal saline is performed and patient is instructed that if any saline is felt in the throat, it should be swallowed and at the same time observe if the saline comes out of the nasal openings. In some cases a dilute solution of flouresceine can also be used for better visualization and confirmation of the successful irrigation of the nasolacrimal passage (Figure 3).
Once a proper sized by-pass opening is created, then I proceed to bicannalicular silicon intubation and the two ends of tube are tied in the nose at a suitable location. The intubation tube is removed after 6 months (Figure 4 and Figure 5).
Post operative care
Patient is advised not to blow the nose as it may cause bleeding and dislodging of the tube placed in the lower part of the nose.
Topical and systemic antibiotic cover is important in the early postoperative period to avoid postop infection.
Nasal decongestant/antibiotic drops are also advised to keep the nasal mucosa decongested.
Topical steroid eye drops to control the post surgery inflammation as inflammation promotes the fibrosis during the healing phase.
Analgesics are also recommended as in some cases pain can be a concern.
Head up positioning in the post op period should be advised as it will help in the drainage of the secretion and any blood oozing.
Complications
Nasal bleeding can take place, but usually this is quite innocuous in most of the cases, usually presents during the procedure and this can be controlled with nasal packing.
Inability to perforate the bone is usually due to a very thick lacrimal bone but in some cases poor intraoperative maneuvering and blunt trephine can also cause this unexpected happening during the surgery.
Infection can take place in any invasive surgical procedure and this surgery is not an exception. However preop evaluation/management and post-operative antibiotic cover is very helpful to avoid this complication
Recurrence of epiphora due to recurrent obstruction, scarring and or the failure of the procedure can also take place after surgery.
Sump leading to epiphora can happen if and when the perforation is made a little high in the lacrimal sac, as a result gravitational flow of the tears takes place in an unnatural way.
Re-closure can take place after removal of the lacrimal tubes and scarring of the bony osteum caused by fibrosis can close the by-pass opening.
Avoiding the risks
Proper preop evaluation is very important to avoid the risk of possible complications.
Proper technique of the procedure is equally important to avoid the risk of complications and to have a successful outcome.
Training must be proper to avoid the risk of complication and to ensure a successful outcome.
Instrumentation has to be proper and perfect, as the technique this procedure demands.
MMC 0.2 mg/ml for 2 minutes should be kept at the end of irrigation onto the guaze packed in the nose. This is likely to help in preventing the post op fibrosis.
Advantages of this technique
This surgical technique appears to be minimally invasive. Since there is no disruption of the lacrimal pump function with this procedure is another advantage. This surgical procedure can be done under topical/local or general anesthesia. Another advantage is that it is cosmetically ideal as there is no risk of scar on the skin/face. It is a short duration procedure of 10-15 minutes and it is easy for the patient to tolerate this short duration of the procedure on the operation table.
Complications associated with conventional external DCR like, risk of bleeding from the angular vein, inadequate size of the bony osteum, wound dishiscence, wound infection, tube displacement, rhinostomy crusting, intra-nasal synechiae formation, facial scar, non functional DCR, medial canthus distortion, sump syndrome, cheeze wiring of the lacrimal cannaliculus, lacrimal pump failure, etc. can be avoided.
Limitations
Since it is a blind procedure without direct observation of the site and size of the bony perforation to make a bypass drainage passage, chances of making a standard opening in terms of the diameter and location of the opening are less than ideal. Moreover the trephine needs to be of larger diameter and better in design features to ensure a proper creation of the bypass channel. At the same time this technique may not be a suitable choice for patients with thick lacrimal bone. Probably a large study may be needed to refine the technique and success of this approach. Treating the bony osteum with mitomycin may prevent the fibrosis and chances of recurrence of nasolacrimal duct block and to enhance the success rate with this surgical approach.
Conclusion
It is a short duration procedure with minimal risk of complication having a high success rate in properly selected patients and with a short learning curve requiring inexpensive instrumentation and minimally invasive anesthesia.
Art work-Nikko Glenn Ramones-RN.
Corresponding Author
Mohammad Idrees, Consultant Ophthalmology, REDO Eye Hospital, Rawalpindi, Pakistan, E-mail: sightsaver88@yahoo.com
Copyright
© 2019 Idrees M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.