A Fitting Warning an Atypical Cause of First Seizure Event
Abstract
Human Immunodeficiency Virus (HIV) has caused one of the greatest global pandemics in recent times and presents with a myriad of clinical manifestations due to its complex pathogenesis. Despite this, there is significant under-detection and delay in diagnosis. HIV also has significant neurological presentations, including seizures, which this case illustrates, as an atypical first presentation of HIV. With minimal risk factors or symptomatology for HIV and imaging findings suggestive of a malignant brain lesion as the cause of her seizures, a pathological diagnosis of toxoplasmosis was ultimately obtained in this patient and led to the eventual HIV diagnosis. She was managed on highly active antiretroviral therapy and anti-parasitic therapy with good clinical effect.
Literature review demonstrates new onset seizures in the setting of HIV are more common than previously expected. Aetiology of seizures in HIV remains broad including a range of infectious, malignant and metabolic causes and investigations for these should be instigated. Though there is wider recognition of the behavioural and epidemiological indications for HIV testing, there is less awareness of the extremely broad clinical indications outside of AIDS defining illnesses. Studies have demonstrated the cost effectiveness of routine HIV testing in various indicator conditions and coupled with the significant clinical benefit in early intervention, suggests a need to increase HIV testing and awareness, including in seizures and neurological diseases.
Keywords
HIV, Seizures, Toxoplasmosis, Testing Indications
Introduction
Human Immunodeficiency Virus (HIV) is the cause of one of the most significant global pandemics in the 20th and 21st centuries with just under fifty million fatalities and an estimated 0.7% of adults worldwide between 15-49-years living with the virus or around 37.7 million people [1].
HIV infection can present in a myriad of ways ranging from asymptomatic, a mononucleosis type of syndrome to various mucocutaneous, gastrointestinal and neurological presentations. If they are late presenters and immunocompromised, patients may present with signs of an opportunistic infection [2].
Despite the availability of effective diagnostic tests, an estimated 11% of people living with HIV are undiagnosed in Australia, while between 22-68% of patients across demographics have a late diagnosis [3].
The most common neurological manifestations of HIV itself is headache, however aseptic meningitis can occur with rarer manifestations possible including encephalopathy, myelopathy, and peripheral neuropathies [4]. The manifestations associated with opportunistic infections are much broader.
Seizures are an uncommonly reported initial presentation of HIV. This case illustrates an unusual presentation of HIV and highlights the potential benefits of routine HIV testing in a wide range of conditions including seizure disorders.
Case Presentation
A 45-year-old independent Caucasian female had multiple presentations to the Emergency Department of a regional hospital after a first episode of seizure. Prior to her first presentation, she attended a recreational event where alcoholic beverages were consumed and subsequently presented with a focal seizure which progressed to a generalised tonic clonic seizure (GTCS) of 3 minutes duration followed by a 1 hour post ictal period.
She was initially discharged after intravenous fluid administration and observation. She recovered spontaneously. Biochemistry was unremarkable however, no intracranial imaging was performed at the time. She subsequently presented 4 days later to a metropolitan centre with pre-ictal paraesthesia in the left arm and associated motor disturbance in the fingers including twitching, before she progressed again to a GTCS of 3 minutes duration with associated tongue biting, all which eventually terminated spontaneously. This was followed by a 40 minute period of post-ictal agitation.
She had no significant medical comorbidities except for scoliosis which required two surgical interventions greater than 20-years ago in 1989 and 1999. On both these occasions she required blood transfusions. She had 5 kg of unintentional weight loss in the 6-12 months preceding her current presentation but no other constitutional symptoms.
She consumed 2-4 standard drinks of alcohol weekly and smoked marijuana 2-4 times per week. She did not smoke cigarettes and did not use any other recreational substances. She has generally maintained stable monogamous relationships and practiced safe sex. Her travel history included a visit to Africa more than 5-years previously. Her physical examination was unremarkable including her neurological examination, which yielded no abnormalities.
Investigations
Laboratory studies demonstrated a lymphopaenia with a lymphocyte count of 0.5 × 10^9/L. Her white cell count (WCC) of 4.5 × 10^9/L, her platelets were 173 × 10^9/L and her haemoglobin was 148 g/L. This was slightly lower than her presentation 4 days ago where her WCC was 7.6 × 10^9/L and her platelets were 204 × 10^9/L.
There were no abnormalities in her biochemistry.
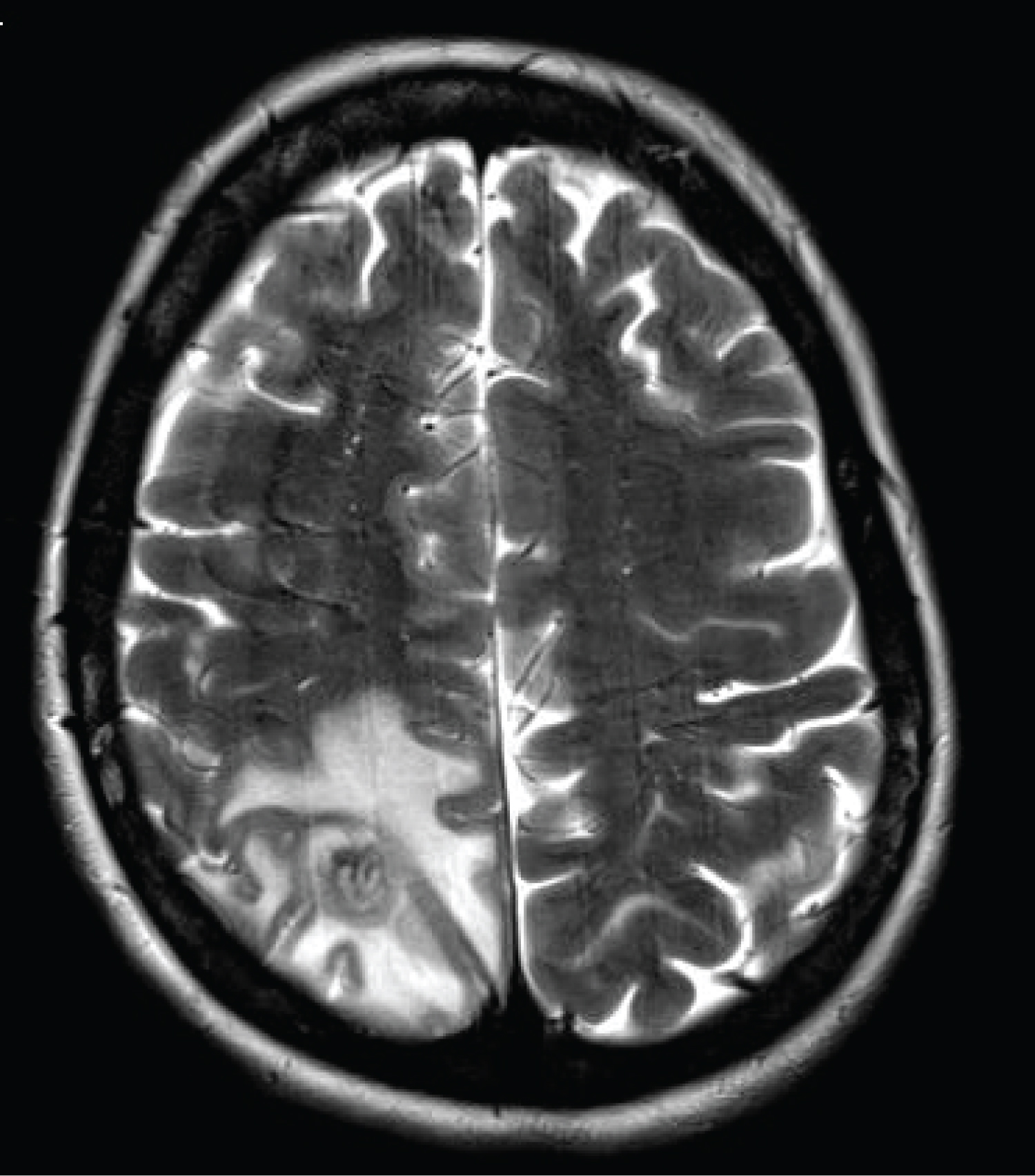
Computed Tomography (CT) of her brain demonstrated a solitary rim enhancing lesion in the right parietal lobe measuring 12 mm in diameter with marked surrounding oedema and mild mass effect, but no haemorrhage, overall suggestive of a metastasis.
Magnetic Resonance Imaging (MRI) of her brain demonstrated a 13x12mm ring enhancing lesion with considerable vasogenic oedema in the right posterosuperior parietal lobe subcortical white matter, again suggestive of a solitary metastasis, though the possibility of a primary brain tumour (e.g. glioma) is not excluded. CT of her chest, abdomen and pelvis for further malignancy screening was negative.
Treatment
The patient was admitted under the Neurosurgical team and commenced on Levetiracetam 500 mg twice daily (BD) and Dexamethasone 4mg, four times a day (QID). She was subsequently discharged after one day on the same medication regimen and Pantoprazole 40mg daily.
Progress
Subsequently, the patient was offered operative management and a stereotactic right parietal craniotomy was performed. Tissue pathology demonstrated widespread necrosis surrounded by reactive gliosis and inflammatory infiltrates but only mildly atypical glial cells with no evidence of metastasis. Instead, encysted organisms highly suspicious for cerebral toxoplasmosis was identified.
HIV testing was subsequently performed, and the patient was diagnosed with HIV with positivity to both HIV antigen and antibody test, a diagnosis confirmed on Western Blot testing. She was significantly immunosuppressed with a CD4+ count of 20 cells/uL and had significant viraemia with a viral load of 17,000 copies/mL. HIV genotyping showed a pansensitive virus.
She also had positive immunoglobulin G (IgG) antibodies to Toxoplasma. The remainder of infection screen was negative including Hepatitis B, C, Tuberculosis and Syphilis. Cytomegalovirus and Epstein-Barr virus testing demonstrated IgG positivity however, both were IgM negative, suggestive of past infection. Ophthalmology review also yielded no evidence CMV retinitis.
She was commenced on Abacavir/dolutegravir/lamivudine combination for treatment of her HIV and commenced on Sulfadiazine 1.5g QID, Pyrimethamine 75mg daily, Calcium Folinate 15 mg daily and also placed on a reducing regimen of prednisone for treatment of her cerebral toxoplasmosis. She was then continued on maintenance therapy of sulfadiazine 1g BD, pyrimethamine 25mg daily and Calcium Folinate 15mg daily for ongoing treatment of toxoplasmosis until here CD4 + count was greater than 200 cells/uL. Her CD4+ cell count eventually recovered to greater than 300 cells/uL and she improved clinically.
Discussion
New onset seizures in HIV are more common than commonly perceived, estimated at a rate of 4-11% [5]. Seizures are more prevalent in HIV patients (approximately 6%) compared with the general population (approximately 0.4-1%) [6].
Furthermore, seizures are the presenting sign of HIV in 18% of patients [7] and most present as generalised seizures [5].
Once HIV infection is confirmed, the potential causes of seizures are broad, with intracerebral opportunistic infection a key differential. Of these, the most common cause involving intracranial mass lesions is toxoplasmosis [5], with other causes including cryptococcal abscess and meningitis, progressive multifocal leukoencephalopathy, tuberculomas and abscesses, syphilitic gummas and nocardial abscesses [5,6,8].
Previous case reports of toxoplasmosis mimicking malignancy have been demonstrated [9], where operative intervention was similarly engaged in prior to HIV diagnosis. This again highlighted the need to maintain a broad differential and exclude potential diagnoses with less invasive investigations before proceeding to invasive intervention.
Other aetiologies of seizures in HIV include metabolic causes such as hyponatraemia and hypomagnesaemia, malignancy such as CNS lymphoma and HIV encephalitis [10,11]. The latter is the most probable cause in patients with no evidently identified brain disease [5].
Investigations to evaluate seizures in the setting of HIV should include intracranial imaging to exclude structural causes. In the elucidation of intracranial pathology, MRI is superior to CT for characterisation of the lesion [12,13]. Blood tests which evaluate current immune status should also be performed including HIV viral load and CD4+ cell count as well as screening for opportunistic infections. Lumbar puncture should also be considered.
At present indications of HIV testing in Australia presently include a combination of behavioural and epidemiological factors as well as clinical indicators.
Common behavioural and epidemiological factors include patients who engage in high-risk sexual practices, men who have sex with men, intravenous drug users and patients from or have travelled to high prevalence countries [14].
Common clinical indicators include any AIDS defining conditions, transfusion recipients from countries where blood supply safety is not guaranteed, pregnant women and a range of indicator conditions [14].
While there is significant awareness of most behavioural and epidemiological factors as well as AIDS defining conditions, there is less awareness of the indicator conditions which are quite broad. Furthermore, despite the wide indications for testing, there is still a significant delay in HIV diagnosis.
Given our diagnosis rate of HIV is approximately 89%, there are 11% of HIV patients who remain undiagnosed in the community [3].
In addition, 36% of new HIV diagnoses were considered late diagnoses [3]. These represent significant proportions of HIV patients who have not availed themselves of the optimal management of this increasingly chronic disease, given highly effective anti-retroviral therapy.
Given that complications of delayed HIV diagnoses are severe from a holistic perspective and there is significantly improved prognosis for patients who have timely diagnosis and treatment for HIV [15], there is significant benefit in increasing both awareness and broadening the testing indications for HIV.
These could include routine HIV screening tests for conditions such as seizures which would both be cost effective and improve prognosis in diagnosed patients.
The HIDES I study demonstrates that it is cost effective to routinely test for indicator conditions where the undiagnosed HIV prevalence is greater than 0.1% [16], and this has been adopted as the recommended guidance from the Euro TEST organisation [17]. The results of this study could potentially be expanded to include neurological disorders such as seizures though further studies are needed.
Seizures are an uncommon but under recognised initial presentation for HIV and through a potential expansion in indications in HIV testing and greater awareness, greater diagnostic clarity and improved patient outcomes may be achieved (Figure 1).
References
- https://www.who.int/data/gho/data/themes/hiv-aids.
- Braun DL, Kouyos RD, Balmer B, et al. (2015) frequency and spectrum of unexpected clinical manifestations of primary HIV-1 infection. Clin Infect Dis 61: 1013-1021.
- https://data.kirby.unsw.edu.au/national-hiv-strategy
- Singer EJ, Valdes-Sueiras M, Commins D, et al. (2010) Neurologic presentations of AIDS. Neurol Clin 28: 253-275.
- Garg RK (1999) HIV infection and seizures. Postgrad Med J 75: 387-390.
- Ssentongo P (2019) Prevalence and incidence of new-onset seizures and epilepsy in patients with human immunodeficiency virus (HIV): Systematic review and meta-analysis. Epilepsy Behav 93: 49-55.
- Holtzman DM, Kaku DA, So YT (1989) New-onset seizures associated with human immunodeficiency virus infection: causation and clinical features in 100 cases. Am J Med 87: 173-177.
- Kim HK, Chin BS, Shin HS (2015) Clinical features of seizures in patients with human immunodeficiency virus infection. J Korean Med Sci 30: 694-699.
- Parekh P, Boggs JP, Silverberg M, et al. (2013) Seizure as an initial presentation of human immunodeficiency virus: Acute toxoplasmosis mimicking glioblastoma multiforme. BMJ case Rep.
- Van Paesschen W, Bodian C, Maker H (1995) Metabolic abnormalities and new-onset seizures in human immunodeficiency virus-seropositive patients. Epilepsia 36: 146-150.
- Wong MC, Suite ND, Labar DR (1990) Seizures in human immunodeficiency virus infection. Arch Neurol 47: 640-642.
- Adam A (2021) Benign and malignant intracranial tumours in adults. (eds) Adam A, Dixon AK, Gillard JH. In: Grainger & Allison's diagnostic radiology: A textbook of medical imaging, (7th edn) Elsevier.
- Richard H, Winn MD (2017) Structural imaging of traumatic brain injury in winn. In: Youmans & Winn neurological surgery, (7th edn) Elsevier.
- https://testingportal.ashm.org.au/national-hiv-testing-policy/indications-for-hiv-testing/
- Lundgren JD, Babiker AG, Gordin F, et al. (2015) Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med 73: 795-807.
- Sullivan AK, Raben D, Reekie J, et al. (2013) Feasibility and effectiveness of indicator condition-guided testing for HIV: Results from HIDES I (HIV indicator diseases across Europe study). PLoS One 8: e52845.
- https://eurotest.org/Projects-Collaborations/Indicator-Condition-Guided-HIV-Testing-HIDES/Guidance-HIV-Indicator-Conditions
Corresponding Author
Yu Feng Shi, Department of Immunology, Concord Hospital, Hospital Road, Concord, NSW, 2139, Australia
Copyright
© 2022 Shi YF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.