Microgranular Acute Promyelocytic Leukaemia (APML) with FLT3p.N676K
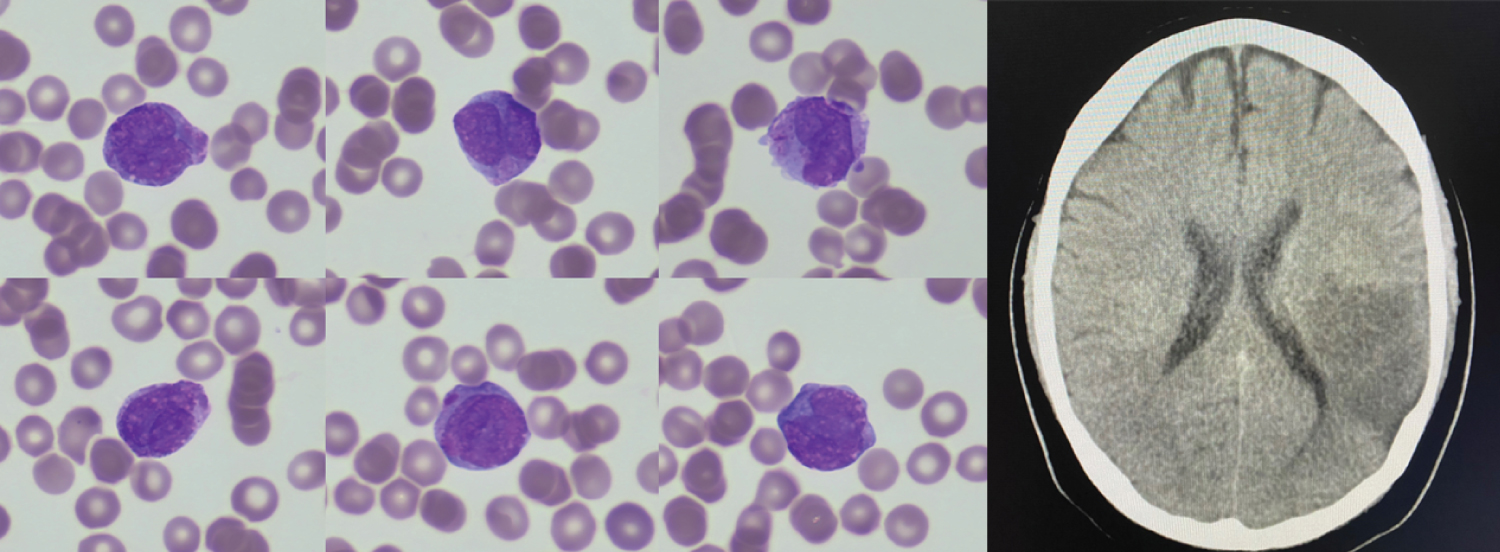
A 46-year-old male presented with easy bruising, easy bleeding, haemoglobin 68 g/L, white blood cells 11.67 × 109/L, platelet 17 × 109/L, PT 15.1 seconds, APTT 25 seconds, fibrinogen 2.7 g/L, D-dimer 74600 μg/L fractional excretion of urea (FEU). The blood film (Figure 1- left panel), May-Grünwald-Giemsa stain ×100 objective) showed pancytopenia and many promyelocytes. Bone marrow smear was infiltrated by hypogranular promyelocytes with frequent Auer rods. By flow cytometry, these cells (78%) were positive for CD34, CD117, CD33, CD56, cMPO and negative for HLA-DR. Fluorescence in situ hybridization analysis detected PML-RARA. Next generation sequencing (Archer variantplex) identified the pathogenic variant in FLT3 p.N676K (VAF 40%). He was treated with all-trans retinoic acid (ATRA), idarubicin, prophylactic steroid and blood products. On day 2 of induction, his WBC went up to 20.9 × 109/L. He developed aphasia and type 1 respiratory failure without fever, cough, chest pain, hemoptysis or positive microbiology findings. Computerised tomography (CT) head (Figure 1- right panel) showed large acute infarction in the middle cerebral artery distribution. As the risk of bleeding was high, antiplatelet and anticoagulation was felt to be contraindicated. Echocardiogram and carotid doppler did not show any cause of stroke. CT pulmonary angiogram showed multifocal ground-glass opacification, without pulmonary embolism or oedema. As the suspicion of differentiation syndrome was high, ATRA was held off until improvement of respiratory failure. Three weeks into induction, he developed sub acute ischaemic bowel, melaena, neutropenic sepsis and he passed away.
APML patients with FLT3-ITD mutations are more likely to present with elevated WBC counts and have poorer prognosis [1]. Here we reported an APML patient with FLT3 p.N676K, who presented with high WBC count, developed thromboembolic events during induction chemotherapy and had early death within 30 days of diagnosis. Rapid molecular testing is important for risk stratification. Novel approach is needed to manage this high-risk group of patients.
References
Corresponding Author
Ke Xu, Department of Haematology, University College London Hospitals NHS Foundation Trust, University College London, London NW1 2PG; Specialist Integrated Haematology Malignancy Diagnostic Service, Health Services Laboratories, University College London Hospitals NHS Foundation Trust, University College London, London, UK, Tel: 0044-(0)2034567890.
Copyright
© 2023 Xu K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.