Research of Pencil Cells and Precheratocyte in Patients with Microcytic Anemia- Our Experience
Abstract
The most frequent forms of microcytic anemia are: Iron deficiency anemia (IDA), β-thalassemia and chronic disease anemia (ACD) alongside the traditional laboratory parameters (RDW, iron, ferritin, etc.), the evaluation of the peripheral smear, for the search for some cellular elements is also fundamental for a correct diagnosis.
Pencil cells are ellipsocytes having the major axis three times longer than the minor axis and the target cells. Precheratocytes are erythrocytes with preserved central pallor and one or more distinct vacuoles, with sharp edges, adhering to the plasma membrane. The aim of this work wanted to evaluate the diagnostic power that the detection of precheratocytes and pencil cells, carried out by quantitative morphological analysis on a peripheral blood smear, has in discriminating the different types of microcytic anemias.
Materials and methods: In the period June-October 2021, 60 patient samples diagnosed with microcytic anemia were recruited at the Hospital Clinical Pathology Laboratory of the Azienda Osepdaliero Universitaria Policlinico di Bari: 20 diagnoses of IDA, 20 diagnoses of ACD, and 20 diagnoses of β-thalassemia who had not received blood transfusions. Whole blood samples, collected in tubes with K2 EDTA anticoagulant, were analyzed within six hours of collection. Two blood smears were prepared from each sample, stained with May-Grunwald-Giemsa Stain for evaluation of erythrocyte morphology. Upon examination under an optical microscope, 20 red blood cells (RBCs) × 50 fields were observed to visualize 1000 RBCs.
Results: Precheratocytes were found in 17/20 (85%) samples of patients with IDA and in 11/20 (55%) samples of patients with β-thalassemia, with a statistically insignificant difference (p = 0.08). 10/20 (50%) patients with ACD had precheratinocytes with a statistically significant difference only compared to patients with IDA (p = 0.04). Pencil cells were found in 17/20 (85%) of patients with IDA and in 11/20 (55%) of patients with β-thalassemia with a statistically insignificant difference (p = 0.08). 11 (55%) of patients with ACD had pencil cells on smear but no statistically significant difference compared to patients with IDA (p = 0.08).
The analysis of the ROC curves, through the values of the area under the curve (AUC) has shown that among the instrumental parameters evaluated the RDW and the % IPO together with the values of precheratocytes and pencil cells, show the highest accuracy in discriminating the cases of IDA from β-thalassemia; the morphological tests alone for the search for precheratocytes and pencil cells show greater accuracy than the other indices in discriminating cases of IDA from ACD. We did not find any statistically significant correlation between the erythrocyte indices and the presence of precheratocytes or pencil cells in the three groups of pathologies considered.
Discussions: The diagnosis of microcytosis is carried out both with the morphological examination on the slide and with the use of erythrocyte parameters provided by the current automatic hematological analyzers. In microcytic hypochromic anemia, poikilocytes, both precheratocytes and ellisoocytes (pencil cells), are more present in patients with iron deficiency anemia (IDA) than in those with chronic disease anemia (ACD) or those with β-thalassemia. The presence of precheratocytes and pencil cells found through the quantitative morphological analysis of the peripheral blood smear could be of support in the differential diagnosis of IDA towards β-thalassemia or ACD.
Keywords
Microcytic anemia, Pencil cells, Precheratocyte
Introduction
Iron deficiency anemia (IDA), β-thalassemia, and to a lesser extent, chronic disease anemia (ACD) are the most common causes of microcytosis [1-3].
The laboratory tests used for their differential diagnosis include the amplitude of red blood cell distribution (RDW), the iron and ferritin assay, the total iron-binding capacity (TIBC), the transferring saturation, the electrophoresis of the hemoglobin, and occasionally, reticulocyte counts and peripheral blood smears [4].
The examination of the peripheral smear, in the case of microcytic anemias, allows the search for particular cytotypes, such as "pencil cells", traditionally described in iron deficiency smears, and the "target cells" or even cells with basophilic punctuation found in cases of Minor β-thalassemia [5-9]. Pencil cells are ellipsocytes having the major axis three times longer than the minor axis [10] and the target cells.
The most recent literature reports that, in addition to the presence of small and hypochromic erythrocytes and pencil cells, a type of poikilocyte called precheratocyte is also found in the IDA smears [11]. Precheratocytes, originally described by Bell as intermediate forms in the sequence of burr cell formation [12], are erythrocytes with preserved central pallor and one or more distinct vacuoles, with sharp edges, adhering to the plasma membrane [7]. It is thought that they are the precursors of keratocytes which, in turn, originate from the amputation of a semilunar membrane fragment following the rupture of the vacuoles present under the plasma membrane [13].
In clinical practice, the use of these morphological features for the differential diagnosis of microcytic anemias is limited due to the scarcity of quantitative data to support this use.
In this work wanted to evaluate the diagnostic power that the detection of precheratocytes and pencil cells, carried out by quantitative morphological analysis on a peripheral blood smear, has in discriminating the different types of microcytic anemias. The paper is also aimed to assess whether there is a correlation between the presence of these cells and some erythrocyte parameters provided by the automated blood count.
Materials and Methods
In the period June-October 2021, 60 patient samples diagnosed with microcytic anemia were recruited at the Hospital Clinical Pathology Laboratory of the Azienda Osepdaliero Universitaria Policlinico di Bari: 20 diagnoses of IDA, 20 diagnoses of ACD, and 20 diagnoses of β-thalassemia who had not received blood transfusions.
Enrolled patients had the following characteristics: patients with IDA had the following parameters: MCV < 80 fl, ferritin < 35 ng/ml, Hb < 13 g/dl; patients with β-thalassemia presented the following parameters: MCV < 80 fl, % HbA2 > 3.2; patients with ACD had the following parameters: MCV < 80 fl, ferritin > 280 ng/ml, Hb < 12 g/dl.
The blood count was performed on the ADVIA 2120 automatic analyzer. The parameters evaluated were: RBC, Hgb, MCV, MCHC, RDW, CHr, % IPO, MICRO/IPO.
Whole blood samples, collected in tubes with K2 EDTA anticoagulant, were analyzed within six hours of collection. Two blood smears were prepared from each sample, stained with May-Grunwald-Giemsa Stain for evaluation of erythrocyte morphology. Upon examination under an optical microscope, 20 red blood cells (RBCs) × 50 fields were observed to visualize 1000 RBCs.
Statistic Analysis
For the statistical analysis the MED CALC program was used, the Fischer test was used for the comparison between the percentage values, the Mann Whitney U test for the comparison between the means, the Pearson test for the analysis of correlation. Values of p < 0.05 were considered statistically significant.
To identify the tests with a better discriminating capacity for the differential diagnostics of microcytic anemia, we compared, through the ROC curve method, the diagnostic accuracy of MCHC, RDW, CHr, % IPO, precheratocytes, and pencil cells and identified the optimal value of cut-off for each test. A 5% p-value threshold was adopted for all tests used.
Results
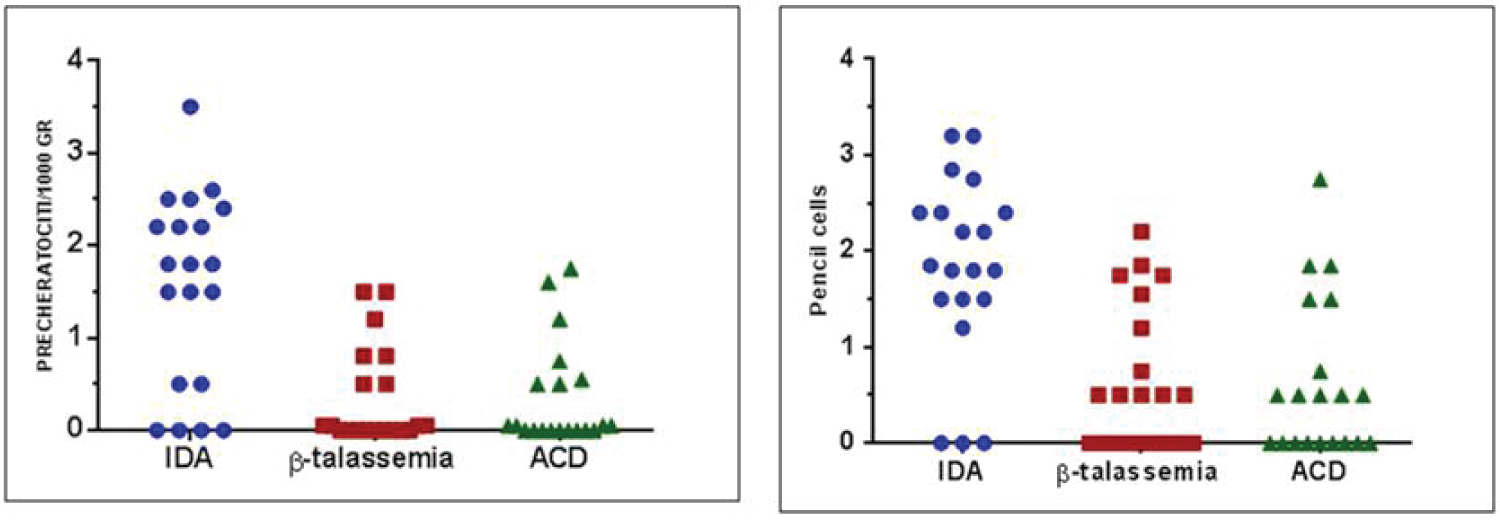
Table 1 reports the data of the mean values of the instrumental parameters evaluated in the three groups of samples and their comparison. The table shows that there is a statistically significant difference for the RDW, % IPO, MICRO/IPO. Precheratocytes were found in 17/20 (85%) samples of patients with IDA and in 11/20 (55%) samples of patients with β-thalassemia, with a statistically insignificant difference (p = 0.08). 10/20 (50%) patients with ACD had precheratinocytes with a statistically significant difference only compared to patients with IDA (p = 0.04). Figure 1 shows the distribution of precheratocytes and pencil cells in the three populations examined.
The mean number of precheratocytes/1000 RBCs was higher in IDAs (1.55) than in both β-thalassemia (0.35) (p = 0.005) and ACD cases (0.36) (p = 0.005). Pencil cells were found in 17/20 (85%) of patients with IDA and in 11/20 (55%) of patients with β-thalassemia with a statistically insignificant difference (p = 0.08). 11 (55%) of patients with ACD had pencil cells on smear but no statistically significant difference compared to patients with IDA (p = 0.08). The mean number of pencil cells/1000 RBCs was higher in IDAs (1.8) than in both β-thalassemia (0.67) (p 0.005) and ACD (0.63) (p < 0.005) (Table 2).
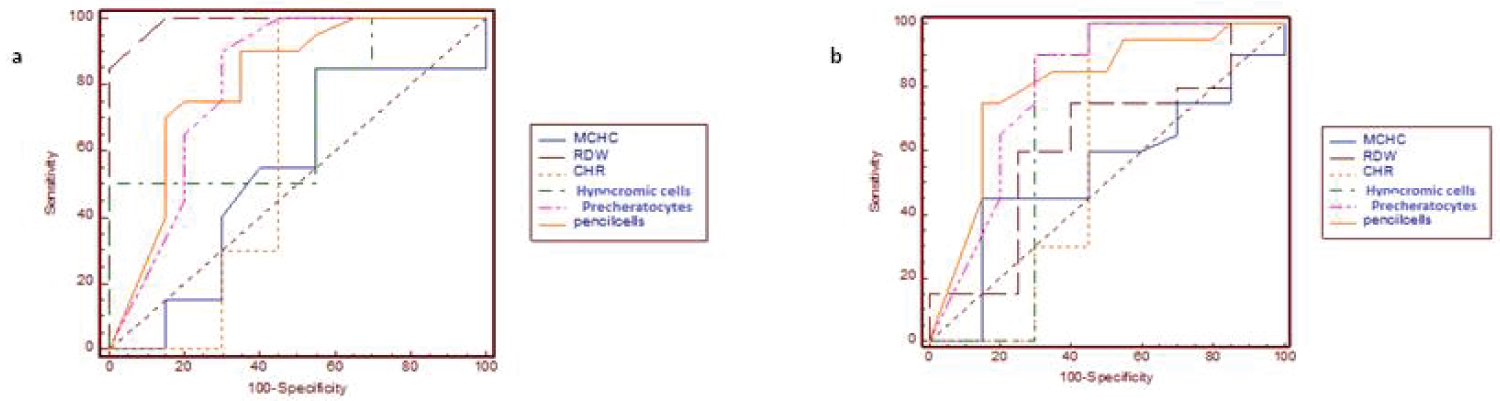
The analysis of the ROC curves, through the values of the area under the curve (AUC) has shown that among the instrumental parameters evaluated the RDW and the %IPO together with the values of precheratocytes and pencil cells, show the highest accuracy in discriminating the cases of IDA from β-thalassemia (Figure 2 and Table 3); the morphological tests alone for the search for precheratocytes and pencil cells show greater accuracy than the other indices in discriminating cases of IDA from ACD (Figure 2 and Table 4).
We did not find any statistically significant correlation between the erythrocyte indices and the presence of precheratocytes or pencil cells in the three groups of pathologies considered (Table 5).
Discussions
The diagnosis of microcytosis is carried out both with the morphological examination on the slide and with the use of erythrocyte parameters provided by the current automatic hematological analyzers. In microcytic hypochromic anemia, poikilocytes, both precheratocytes and ellisoocytes (pencil cells), are more present in patients with iron deficiency anemia (IDA) than in those with chronic disease anemia (ACD) or those with β-thalassemia [11].
The contribution of the morphological examination to the differential diagnosis of microcytic anemias remains controversial [14]. In fact, if it is true that the different parameters provided by the current hematological analyzers in use have largely replaced the morphological examination of the peripheral blood smear, it is also true that in iron deficiency anemia, for example, it is possible to identify microcytosis on the slide before it occurs. have a reduction in MCV.
The authors wanted to evaluate whether the presence of precheratocytes and pencil cells found through the quantitative morphological analysis of the peripheral blood smear could be of support in the differential diagnosis of IDA towards β-thalassemia or ACD. Our results confirm the literature data indicating a significantly higher quantity of poikilocytes in the blood smears of patients with iron-deficient anemia compared to cases of β-thalassemia and ACD. Through the study of the ROC curves it is clear that precheratocytes and pencil cells have a good diagnostic capacity in discriminating patients with IDA from those with β-thalassemia or ACD; RDW shows a high performance in discriminating patients with IDA from those with β-thalassemia.
Conclusion
From the data collected, it is possible to state that although the morphological examination of the peripheral smear cannot be used as a major criterion for the differential diagnosis of microcytic anemias, it certainly represents a valid diagnostic aid in support of automation in the differential diagnosis of microcytic anemias.
Author Contributions
A.M., R.L. and M.P. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: A.M., R.L., S.S., and V.B. Acquisition, analysis, and interpretation of data: M.P., R.L., L.L., F.C., D.L., F.D.S. Drafting of the manuscript: A.M., R.L., S.S. and E.C. Critical revision of the manuscript for important intellectual content: R.L., MI.P., L.L, and F.D.S. Statistical analysis: F.C., R.L. and V.B. Administrative, technical, or material support: M.P., and F.D.S. Supervision: E.C., L.L., and F.D.S. All authors have read and agreed to the published version of the manuscript.
Funding
No public funds or private grants available for this paper.
Acknowledgments
The authors express their gratitude to Catacchio Fara, Pertosa Luigia, Ferrara Gianfilippo for there contribution to preparation the peripheral smear. Without their contribution it would not have been possible to do this work.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Moreno Chulilla JA, Romero Colás MS, Gutiérrez Martín M (2009) Classification of anemia for gastroenterologists. World J Gastroenterol 15: 4627-4637.
- Guralnik JM, Eisenstaedt RS, Ferrucci L, et al. (2004) Prevalence of anemia in persons 65-years and older in the United States: Evidence for a high rate of unexplained anemia. Blood 104: 2263-2268.
- Thomas C, Thomas L (2005) Anemia of chronic disease: Pathophysiology and laboratory diagnosis. Lab Hematol 11: 14-23.
- Vranken Michele Van (2010) Evaluation of microcytosis. Am Fam Physician 82: 1117-1122.
- Perkins S (2006) Diagnosis of anemia and hypochromic microcytic anemia. In: Kjeldsberg CR, Practical Diagnosis of Hematologic Disorders. Vol 1. Chicago, IL: ASCP Press 2006: 3-16.
- Beutler E, Kipps TJ, et al. (2006) Williams Hematology, New York, NY: McGraw-Hill, 565-570.
- Glassy EF (1998) Color atlas of hematology. Northfield, IL: College of American Pathologists.
- Joishy SK, Shafer JA, Rowley PT (1986) The contribution of red cell morphology to the diagnosis of beta-thalassemia trait. Blood Cells 11: 367-374.
- Rowley PT (1976) The diagnosis of beta-thalassemia trait: A review. Am J Hematol 1: 129-137.
- Rodgers MS, Chang CC, Kass L (1999) Elliptocytes and tailed poikilocytes correlate with severity of iron-deficiency anemia. Am J Clin Pathol 111: 672-675.
- Harrington AM, Ward PCJ, Kroft SH (2008) Iron deficiency anemia, ß-thalassemia minor, and anemia of chronic disease: A morphologic reappraisal. Am J Clin Pathol 129: 466-471.
- Bell RE (1963) The origin of "Burr" erythrocytes. Br J Haematol 9: 552-555.
- Harrington AM, Kroft SH (2008) Pencil cells and prekeratocytes in iron deficiency anemia. Am J Hematol 83: 927.
- Jen P, Woo B, Rosenthal PE, et al. (1983) The value of the peripheral blood smear in anemic inpatients: The laboratory's reading v a physician's reading. Arch Intern Med 143: 1120-1125.
Corresponding Author
Dr. Roberto Lovero, Clinical Pathology Unit, AOU Policlinico Consorziale di Bari, Ospedale Giovanni XXIII, Bari 70124, Italy; Azienda Ospedaliero-Universitaria Consorziale Policlinico di Bari, University of Bari "Aldo Moro", Piazza Giulio Cesare n.11, 70124 Bari, Italy.
Copyright
© 2022 Mileti A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.