Prediction of 5-year Mortality in Invasively Managed NSTE-ACS Patients: Role of the Age, Creatinine, And Ejection Fraction (ACEF) Score
Abstract
Background: Long-term risk stratification in non-ST-elevation acute coronary syndrome (NSTE-ACS) by the ACEF score has not yet been assessed. The ACEF score (age/left ventricular ejection fraction +1 [if creatinine > 20 mg/l]) has been established in patients evaluated for coronary artery bypass surgery.
Methods: This is a prospective observational study, including 196 NSTE-ACS patients with invasive management and completing a 5-year follow-up after hospital discharge. ACEF score was calculated at admission. The primary endpoint was 5-year all-cause death. The secondary endpoint was major adverse cardiac and cerebrovascular events (MACCE). The overall population was divided into tertiles of ACEF score (low, mid, and high ACEF score). The discrimination of the ACEF score was assessed by receiver operating characteristic curves and associated area under the curve (AUC) and evaluated in a multivariate analysis.
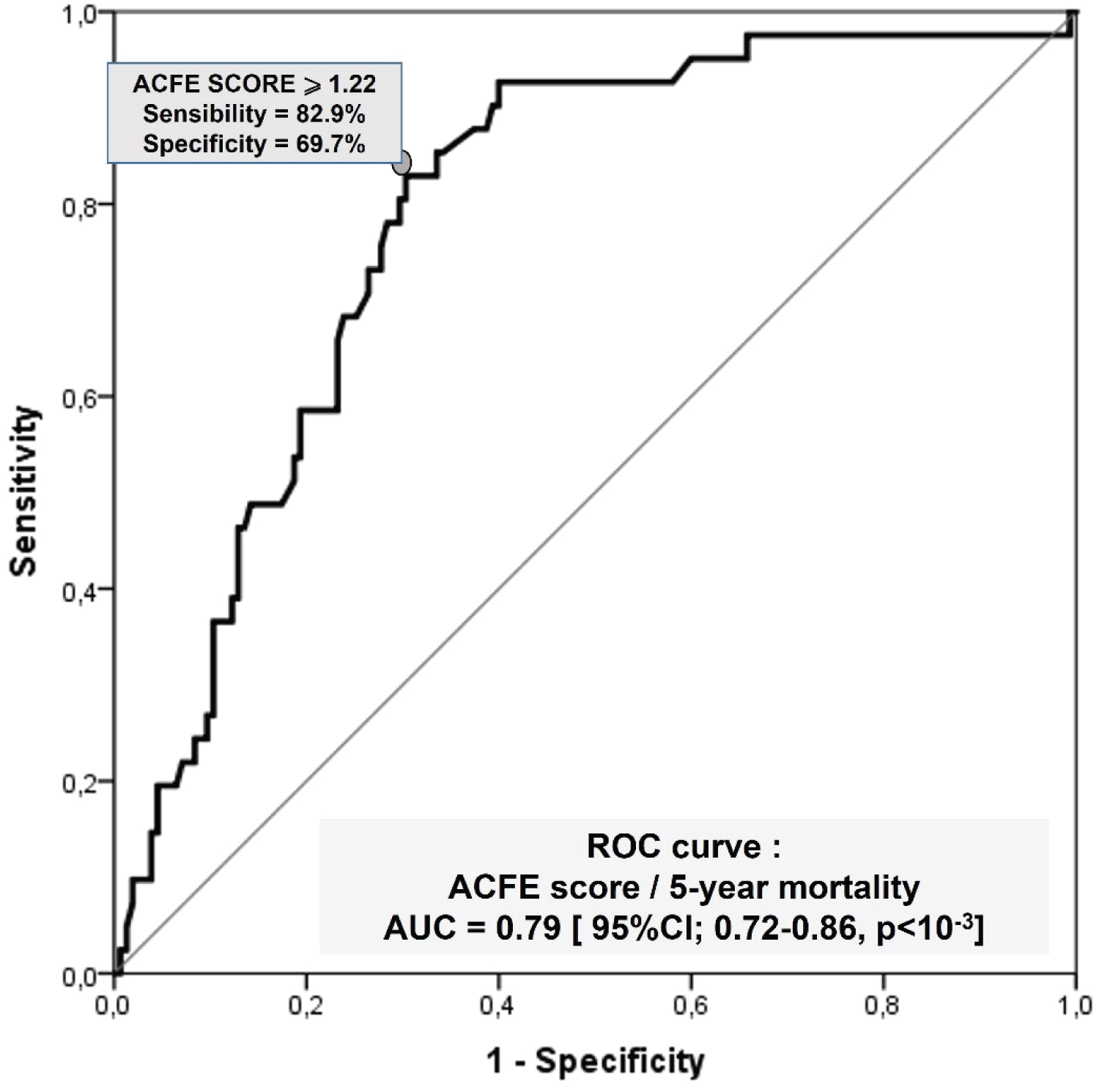
Results: Patients in the ACEF-High tertile showed the highest incidence of death at 5 years (43.1% vs. 3.1% in ACEF-Low and 16.4% in ACEF-Mid; log-rank p < 10-3). The ACEF score could significantly discriminate between patients who died and those who were still alive at 5 years (AUC 0.79, 95%CI 0.72-0.86), and an ACEF score ≥ 1.22 was identified as the optimal cutoff point to predict 5-year mortality (sensitivity 82.9%, specificity 69.7%). An ACEF score ≥ 1.22 was an independent predictor of 5-year mortality (HR 10.98, 95% CI 4.34-27.80; p < 10-3).
Conclusion: The ACEF score is a simple and useful tool for long-term risk stratification in NSTE-ACS patients.
Keywords
ACEF score, NSTE-ACS, 5-year mortality, Long-term risk stratification
List of Abbreviations
ACEF Score: Age, Creatinine, And Ejection Fraction Score; ACS: Acute Coronary Syndrome; AUC: Area under the Curve; CABG: Coronary Artery Bypass Graft; CI: Confidence Interval; CVA: Cerebrovascular Accident; HR: Hazard Ratios; MACCE: Major Adverse Cardiac and Cerebrovascular Events; MI: Myocardial Infarction; NSTE-ACS: Non-ST Elevation Acute Coronary Syndrome; PCI: Percutaneous Coronary Intervention; ROC: Receiver Operating Characteristic Curve; rSS: residual Syntax Score; SD: Standard Deviation; STEMI: ST-Elevation Myocardial Infarction; Syntax Score: Synergy between PCI with Taxus and Cardiac Surgery Score
Background
Acute coronary syndrome (ACS) is a syndrome caused by decreased blood flow in the coronary arteries and is known to be the first cause of mortality in Algeria and most countries [1].
Predicting clinical outcomes in patients suffering non-ST-elevation acute coronary syndrome (NSTE-ACS) is essential in current practice. Several predictive scores have been proposed, which can be categorized as clinical, anatomical, and composed [2-4].
The age, creatinine, and ejection fraction (ACEF) score was introduced in 2009 by Ranucci, et al. with the purpose to predict short- and long-term outcomes in patients undergoing coronary artery bypass graft (CABG) [5]. After this first work, the predictive value of the ACEF score has been evaluated in patients treated with percutaneous coronary intervention (PCI) for cardiac and non-cardiac outcomes [6-8].
Moreover, there is a lack of evidence regarding the capability of the ACEF score to maintain its predictive power in an acute statement like patients with NSTE-ACS and at long-term follow-up. The purpose of this study was to evaluate the predictive power of the ACEF score at 5-year follow-up in a population of patients with NSTE-ACS managed invasively.
Methods
Study population and procedures
This was a single-center observational prospective study. All patients with NSTE-ACS undergoing coronary angiography at the department of cardiology - CHU Oran, Algeria between November 2015 and October 2016 were considered eligible.
All patients, including those receiving conservative treatment, underwent coronary angiography. Patients without significant coronary artery lesion (coronary stenosis < 50%) and who do not complete the 5-year follow-up were excluded. The local scientific committee approved this study, with all patients giving written informed consent for coronarography, data storage, and analysis.
According to standard practice, coronary angiography, percutaneous coronary intervention (PCI), and CABG were performed. The technicalities of the procedure were left at the operator’s discretion. All patients were treated with a tailored treatment plan, which included dual anti-platelet therapy, in line with the 2015 NSTE-ACS ESC guidelines [9].
ACEF score calculation
The ACEF score was calculated as follows: ACEF = age/left ventricle ejection fraction +1 [if creatinine > 20 mg/l] [5]. The left ventricular ejection fraction was calculated by echocardiography using the standard biplane Simpson method. The first available value of serum creatinine was considered.
The extent and de complexities of the coronary lesion were evaluated by the proportion of patients with multivessel disease, significant left main coronary artery disease (LMCAD), and the Syntax (Synergy Between PCI with Taxus and Cardiac Surgery) score: a system for grading the complexity of coronary anatomy via angiography (Sianos, et al., 2005). After the invasive attitude, we calculated the residual Syntax score (rSS) to assess the revascularization proportion [10-13].
Follow-up and clinical end points
Clinical follow-up was obtained up to 5 years using office visits or telephone interviews. The primary endpoint of the study was all-cause mortality. Secondary endpoints were major adverse cardiac and cerebrovascular events (MACCE), which included cardiac death, non-fatal myocardial infarction (MI), or cerebrovascular accident (CVA). MI included both periprocedural and spontaneous events and was defined according to the fourth universal definition [14]. CVA was defined as any cerebrovascular accident confirmed by cerebral imaging.
Statistics
Continuous variables are expressed as mean ± SD, or median (interquartile range). Categorical variables are reported as frequencies and percentages. Normality of ACEF score distribution was assessed with the Kolmogorov-Smirnov test. One-way analysis of variance or Kruskal-Wallis test was used to compare continuous variables between tertiles of ACEF score.
Comparisons between categorical variables were evaluated using the Pearson χ2 test. Survival curves were built using the Kaplan-Meier method, and the log-rank test was used to evaluate differences between groups. Cox regression analysis was used to find independent predictors of death, with results expressed as hazard ratios (HR) and 95% confidence intervals (CIs). Specifically, all variables with a significant (< 0.05) univariate association with the outcome measure were included in the multivariate model. The calibration of the ACEF score was evaluated using the Hosmer-Lemeshow goodness-of-fit test (the lower the χ2 value and higher the p-value, the more calibrated the score), and by calculating the mean absolute difference between the observed and the expected event rate across the ACEF score tertiles (Mean Δ; the lower the value, the better the calibration). The discrimination of the ACEF score was assessed by receiver operating characteristic curves and associated area under the curve (AUC) and by the index of separation (difference between the predicted probability of an event in the group with the worst prognosis and the predicted probability in the group with the best prognosis). The optimal cutoff point of ACEF score to discriminate between patients with and without events was calculated by determining the value that provided the greatest sum of sensitivity and specificity.
All statistical analyses were performed using SPSS 23 (IBM), and a p-value < 0.05 was considered statistically significant.
Results
In this prospective observational study, 296 patients with a suspected NSTE-ACS diagnostic were initially assessed, 100 patients of them do not match the inclusion criteria; 74 (25.0%) patients were excluded for the absence of significant coronary artery lesion at the coronarography, 04 (04/222;1.8%) patients died during the hospital stay and 22 (22/218;10.1%) patients do not complete the 5-year follow-up (the reasons for loss of follow-up were inability to contact a patient or patient refusal of further follow-up).
Finally, the study population included 196 patients with a mean age of 63 years [30-90 years] and a male gender predominance (67.3%).
Of the 196 patients who completed follow-up, death occurred in 41 patients (20.9%) and MACCE in 85 patients (43.4%) including 37 cardiac deaths (18.9%), 55 MI (28.1%) and 4 ischemic strokes (2.0%).
The ACEF score did not follow a normal distribution (Kolmogorov-Smirnov = 0.106; p < 10-3), ranging from 0.46 to 2.57 with a median of 1.16 (interquartile range from 0.96 to 1.46). The overall population was divided into tertiles of ACEF score: ACEF-Low (< 0.97; n = 64), ACEF-Mid (between 0.97 and 1.24; n = 67), and ACEF-High (> 1.24; n = 65). The clinical, procedural characteristics and outcomes are shown in Table 1. Patients in the ACEF-High tertile had more frequent hypertension, prior MI, KILLIP ≥ 2 at the initial presentation, multivessel disease, and significant left main coronary artery disease (LMCAD), however, they had a fewer smokers.
There was no significant difference in the medical strategy (conservative, PCI, or CABG) and in the number of patients who do not receive revascularization (conservative treatment only) between ACEF score tertiles (36.9% vs. 32.8% vs. 29.6%; p = 0.682).
In terms of revascularization statutes, despite a higher mean Syntax score in high ACEF score tertile, after invasive management, there were no differences in the rSS (residual Syntax score) between the ACEF score tertiles (Table 1).
Clinical events at 5 years
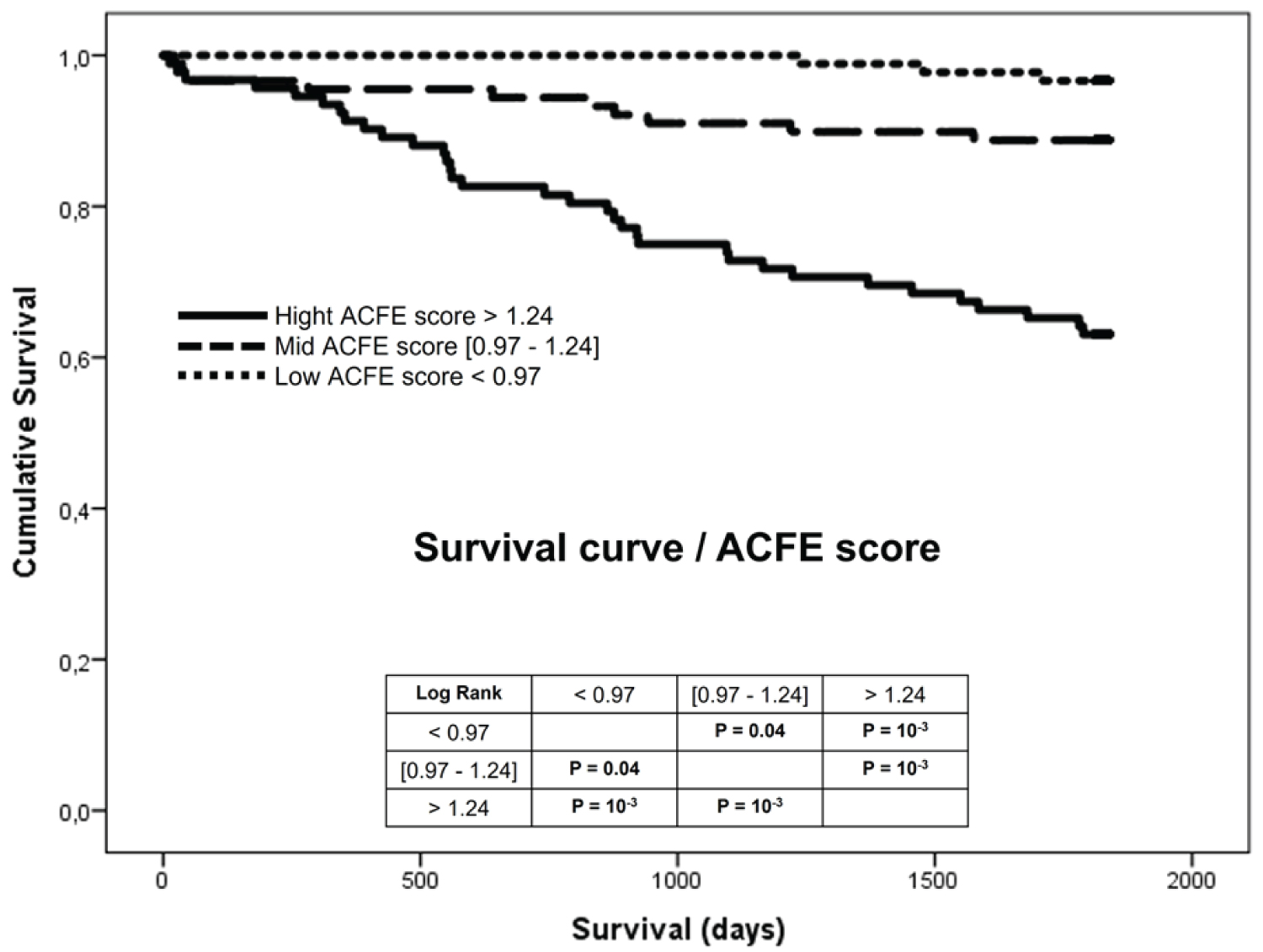
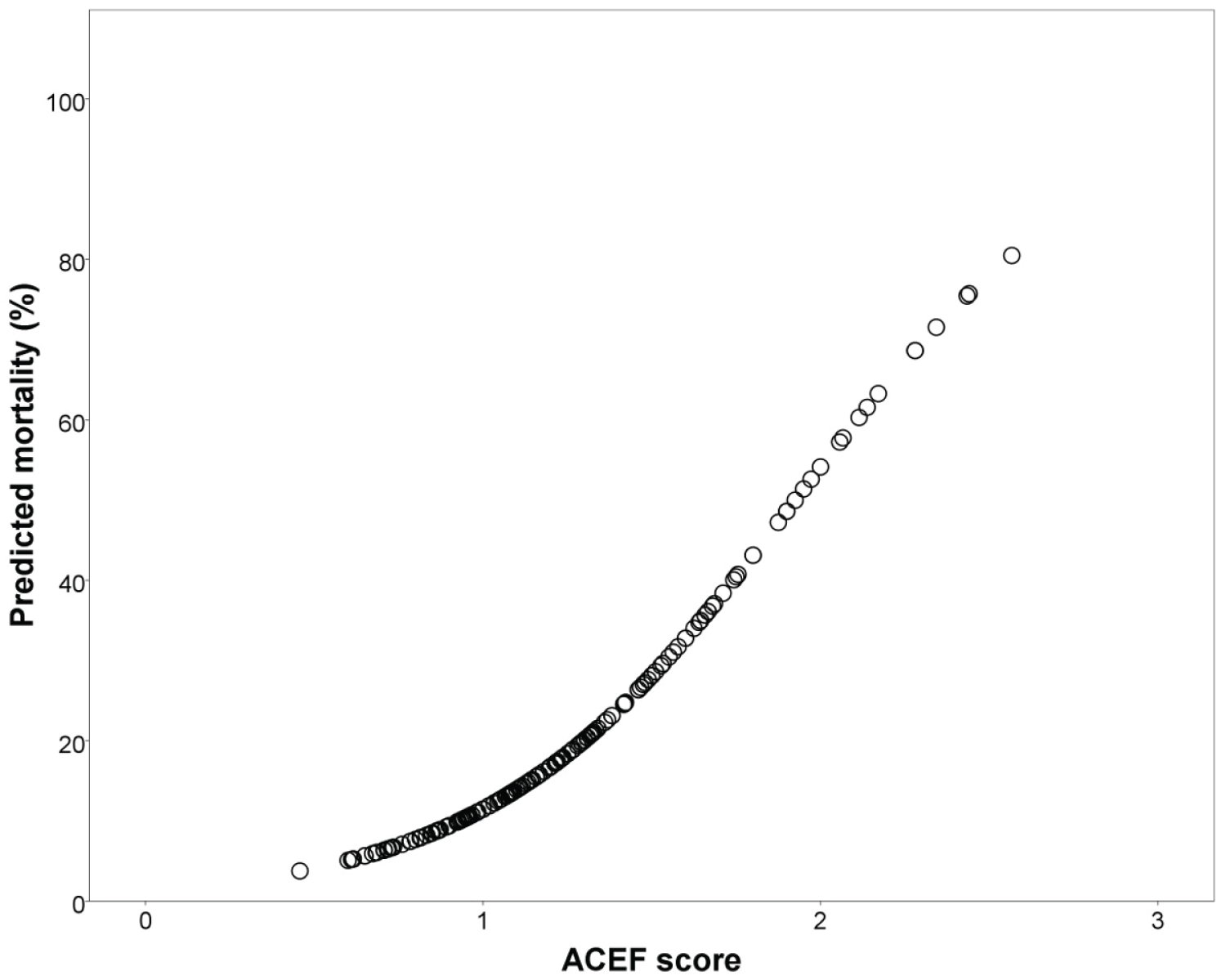
The cumulative incidence of clinical events at 5 years is reported in Table 1. The ACEF score showed good calibration and discrimination for 5-year death and MACCE occurrence (Table 2). Kaplan-Meier curves for death at 5-year according to ACEF score tertiles are depicted in Figure 1. Patients in the ACEF-High group showed the highest incidence of death (43.1% log-rank; p < 10-3 vs. both ACEF-Low and ACEF-Mid). A significant difference was observed in the 5-year incidence of death between the ACEF-Low (3.1%) and the ACEF-Mid tertiles (16.4%) (log-rank; p = 0.04). The relationship between ACEF score and 5-year mortality risk is graphically shown in Figure 2.
No significant difference was observed across ACEF score tertiles in the incidence of non-fatal MI and CVA, whereas patients in the ACEF-high tertile presented the highest rates of MACCE (56.9%, log-rank; p = 0.018).
ROC Curve and Cox regression analysis
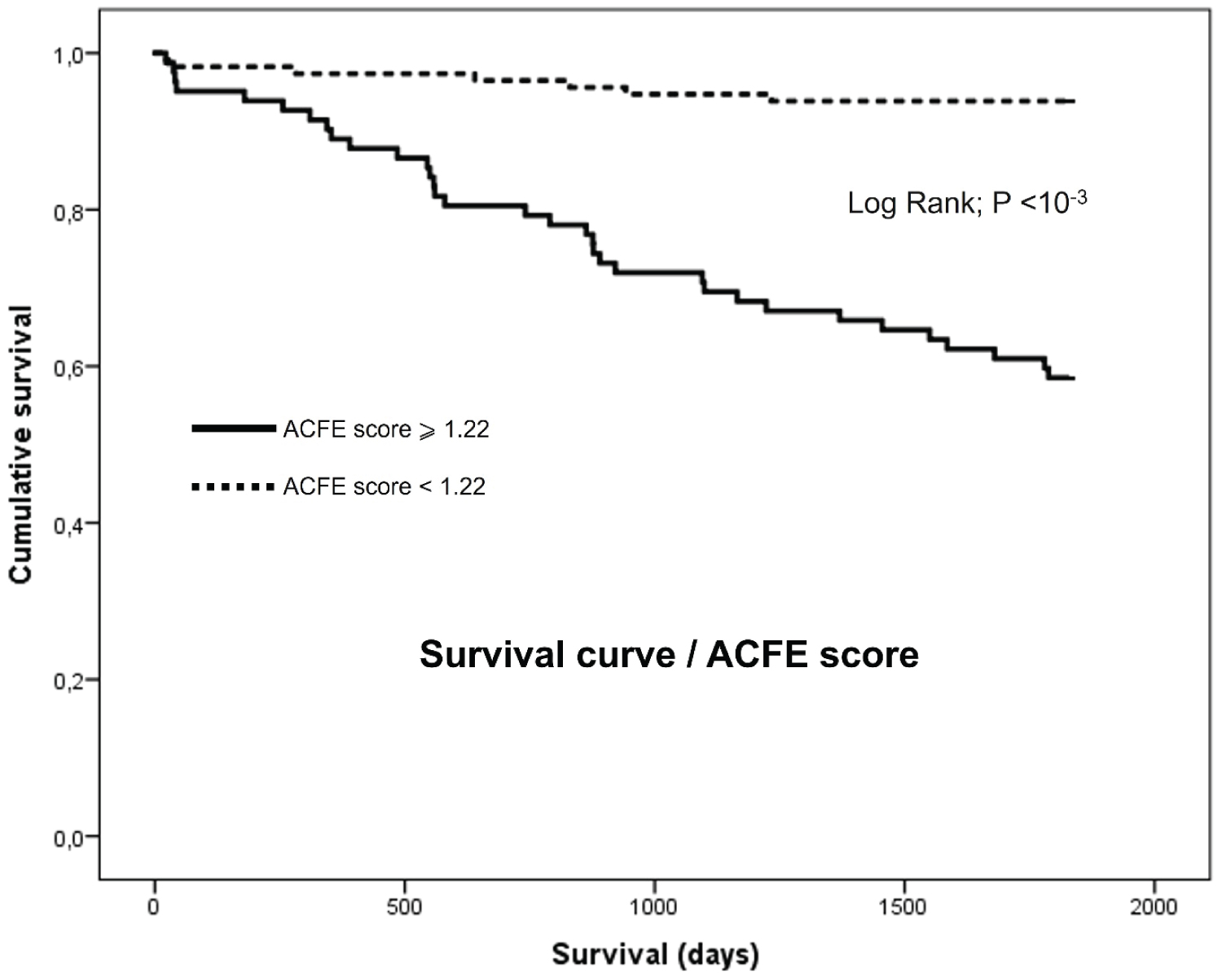
At ROC curve analysis, the ACEF score could significantly discriminate between patients who died and those who were still alive at 5 years (AUC 0.79, 95%CI 0.72-0.86, p < 10-3; Table 2 and Figure 3). An ACEF score ≥ 1.22 was identified as the optimal cutoff point to predict 5-year mortality, with a sensitivity of 82.9%, and specificity of 69.7% confirmed by the analysis of the Kaplan Maier survival curve shown in Figure 4. Five-year mortality was 41.5% in patients with ACEF score ≥ 1.22 and 6.1% in patients with ACEF score < 1.22 (unadjusted HR 8.22, 95% CI 3.64-18.56; p < 10-3). After adjustment for other univariate predictors of death (significant LMCAD, multivessel disease, and the absence of revascularization), ACEF score values ≥ 1.22 remained independently associated with 5-year mortality (HR 7.19, 95% CI 3.16-16.34, p < 10-3; significant LMCAD: HR 2.67, 95% CI 1.29-5.64, p = 0.010 and the absence of revascularization: HR 1.96, 95% CI 1.03-3.71, p = 0.040).
Discussion
In our study, the ACEF score effectively predicted death at 5-year follow-up in NSTE-ACS managed invasively. Patients with ACEF score ≥ 1.22 had a more than 7-fold increase in mortality compared to those with a lower ACEF score. ACEF risk score incorporates only three variables, thereby representing one of the simplest scores in terms of assessment [5]. To our knowledge, this is the first study investigating the predictive ability of ACEF score on hard outcomes at such long-term follow-up in a population of patients suffering NSTE-ACS managed invasively regardless of therapeutic attitude (PCI, CABG, or medical treatment only) reflecting the real-life practice. Most of the studies investigating the predictive ability of the ACEF score were conducted in ACS or chronic coronary syndrome (CCS) patients treated only by CABG or PCI [15-18], few studies have focused on patients managed conservatively [19,20].
In studies investigating ACS patients exclusively, the ACEF score was able to predict 1-year mortality as effectively as more sophisticated predictive models [21].
In our cohort, patients with the highest ACEF score tertile showed significantly increased rates of MACCE (including cardiac death, non-fatal myocardial infarction, or cerebrovascular accident) at 5-year follow-up. However, this endpoint was driven by an increase in cardiovascular mortality. Non-fatal-MI and CVA were not significantly different across ACEF score tertiles. One aspect worth considering in the interpretation of these results relates to the extent of the coronary lesion and the revascularization status. The absence of revascularization is strongly related to the increased risk of adverse events [22]. It could be speculated that revascularization could reduce the ischemic and anatomical burden related to coronary lesions, thus impacting the performance of the score in adverse events prediction. In our study, the high ACEF score tertile included more patients with multivessel disease and high mean Syntax score but after the invasive management of patients, there were no significant differences between ACEF tertiles in terms of mean residual Syntax score indicating a consistent revascularization index in the different tertiles and complete revascularization was achieved in 75% of the procedures in the PCI group.
As to the length of follow-up, few previous studies have investigated the predictive ability of ACEF score beyond one year. In a study of 348 patients with complex coronary artery disease (51.4% with ACS), ACEF had a good discrimination ability for mortality (AUC = 0.77) at four years [23].
In our study, we found similar discrimination ability of ACEF score for 5-year mortality (AUC = 0.79), suggesting similar performance in patients with STEMI, NSTE-ACS, and chronic coronary syndrome (CCS).
ACEF score is a simple prognostic model, and, as such, it is easily computable in most patients, especially those with NSTE-ACS undergoing coronarography. Several factors could explain the findings of respectable AUC values of purely clinical risk score without the inclusion of angiographic parameters.
Firstly, the study population which encompassed only NSTE-ACS patients with significant coronary stenosis at the coronarography could be less affected by the angiographic findings. Furthermore, longer follow-up in the present study could diminish the influence of acute setting parameters like Killip class; abnormal cardiac enzymes; ECG changes). Finally, age, creatinine level, and cardiac capacity are known to be strong independent factors of mortality and have a similar influence on short-term and long-term outcomes, while the inclusion of other parameters has more impact on the treatment strategy and short-term prognosis [24-26].
The present analysis has revealed that NSTE-ACS patients with significant left main coronary artery disease (LMCAD) had a worse prognostic and the absence of revascularization by PCI or CABG of these patients with significant coronary stenosis (explained by the extended and/or very narrowing of lesions, distal lesion and weakened patients recused for CABG) was associated with high 5-year mortality. These findings are not surprising since significant LMCAD and the absence of revascularization are well-established negative prognostic factors [27-29].
Being able to identify patients with increased risk of mortality, incorporating ACEF score calculation in our routine clinical practice might help to improve post-discharge management. More aggressive secondary prevention measures (more frequent monitoring of renal and cardiac function, adaptation of the medication prescription like the duration of the double anti-aggregating platelet therapy, and cardioverter-defibrillators implantation for prevention of sudden death following the guidelines) might be beneficial in such patients.
Limitations of the study
A small sample size despite a high incidence of endpoints does not allow for additional sub-analyses and only NSTE-ACS patients who underwent coronary angiography with significant coronary stenosis were included disallowing generalizing the result to patients treated without coronary angiography and those with non-significant coronary lesions.
Conclusion
Our study shows that the ACEF score, a simple clinical risk score can predict mortality at 5-year follow-up in patients with NSTE-ACS managed invasively undergoing all-treatment strategies.
Declarations
Ethics approval and consent to participate: The local university scientific committee (Oran university 1 "Ahmed BenBella", Algeria) approved this study, with all patients giving written informed consent for coronarography, data storage, and analysis.
Committee Reference number
Not available and not applicable as this was not a clinical trial (we did nothing to the patients for the sake of the study).
Consent for publication written informed consents were obtained from the participant’s Availability of data and material: The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Competing interests
The author declares that he has no competing interests.
Funding
None.
Authors' contributions
The author conceived the idea and designed the study model. He collected data, analyzed the data, and wrote the manuscript. He revised the work. The author has read and approved the manuscript.
Acknowledgments
None.
References
- Vos T, Lim SS, Abbafati C, et al. (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet 396: 1204-1222.
- Serruys PW, Farooq V, Vranckx P, et al. (2012) A global risk approach to identify patients with left main or 3-vessel disease who could safely and efficaciously be treated with percutaneous coronary intervention: The SYNTAX trial at 3 years. JACC Cardiovasc Interv 5: 606-617.
- Bob-Manuel T, Ifedili I, Reed G, et al. (2017) Non-ST elevation acute coronary syndromes: A comprehensive review. Curr Probl Cardiol 42: 266-305.
- Farooq V, Van Klaveren D, Steyerberg EW, et al. (2013) Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: Development and validation of SYNTAX score II. Lancet 381: 639-650.
- Ranucci M, Castelvecchio S, Menicanti L, et al. (2009) Risk of assessing mortality risk in elective cardiac operations: age, creatinine, ejection fraction, and the law of parsimony. Circulation 119: 3053-3061.
- Wykrzykowska JJ, Garg S, Onuma Y, et al. (2011) Value of age, creatinine, and ejection fraction (acef score) in assessing risk in patients undergoing percutaneous coronary interventions in the “All-Comers” LEADERS Trial. Circ Cardiovasc Interv 4: 47-56.
- Chichareon P, Modolo R, van Klaveren D, et al. (2019) Predictive ability of ACEF and ACEF II score in patients undergoing percutaneous coronary intervention in the GLOBAL LEADERS study. Int J Cardiol 286: 43-50.
- Biondi-Zoccai G, Romagnoli E, Castagno D, et al. (2012) Simplifying clinical risk prediction for percutaneous coronary intervention of bifurcation lesions: The case for the ACEF (age, creatinine, ejection fraction) score. EuroIntervention 8: 359-367.
- Roffi M, Patrono C, Collet J-P, et al. (2016) 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task force for the management of acute coronary syndromes in patients presenting without persistent st-segment elevation of the european society of cardiology (ESC). Eur Heart J 37: 267-315.
- Serruys PW, Hara H, Onuma Y (2020) Did the SYNTAX score pass the test of time? JACC Cardiovasc Interv 13: 1207-1210.
- Milojevic M, Head SJ, Mack MJ, et al. (2017) Influence of practice patterns on outcome among countries enrolled in the SYNTAX trial: 5-year results between percutaneous coronary intervention and coronary artery bypass grafting. Eur J Cardiothorac Surg 52: 445-453.
- Takahashi K, Serruys PW, Gao C, et al. (2021) Ten-year all-cause death according to completeness of revascularization in patients with three-vessel disease or left main coronary artery disease: Insights from the SYNTAX extended survival study. Circulation 144: 96-109.
- Farooq V, Serruys PW, Bourantas CV, et al. (2013) Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation 128: 141-151.
- Thygesen K, Alpert JS, Jaffe AS, et al. (2019) Fourth universal definition of myocardial infarction (2018). European Heart Journal 40: 237-269.
- Brunetti ND (2018) The ACEF score in acute coronary syndrome: "Never was so much owed by so many to so few". Int J Cardiol 270: 70-71.
- Chen H, Yu X, Kong X, et al. (2021) Predictive value of ACEF score for clinical prognosis of elderly patients with ST-segment elevation myocardial infarction after percutaneous coronary intervention. Ann Palliat Med 10: 1380-1387.
- Reindl M, Reinstadler SJ, Tiller C, et al. (2018) ACEF score adapted to ST-elevation myocardial infarction patients: The ACEF-STEMI score. Int J Cardiol 264: 18-24.
- Ösken A, Hacı R, Şekerci SS, et al. (2021) Predictive value of the age, creatinine and ejection fraction score in patients undergoing primary percutaneous coronary intervention with bail-out tirofiban therapy. Postepy Kardiol Interwencyjnej 17: 170-178.
- Gao S, Ma W, Huang S, et al. (2021) Predictive value of the age, creatinine, and ejection fraction score in patients with myocardial infarction with nonobstructive coronary arteries. Clin Cardiol 44: 1011-1018.
- Dziewierz A, Siudak Z, Rakowski T, et al. (2017) The ACEF (age, creatinine, ejection fraction) score predicts ischemic and bleeding outcomes of patients with acute coronary syndromes treated conservatively. Postepy Kardiol Interwencyjnej 13: 160-164.
- Lee JH, Bae MH, Yang DH, et al. (2015) Prognostic value of the age, creatinine, and ejection fraction score for 1-year mortality in 30-day survivors who underwent percutaneous coronary intervention after acute myocardial infarction. Am J Cardiol 115: 1167-1173.
- Nagaraja V, Ooi SY, Nolan J, et al. (2016) Impact of incomplete percutaneous revascularization in patients with multivessel coronary artery disease: A systematic review and meta-analysis. J Am Heart Assoc 5: 1-22.
- Janella BL, Campos CM, Caixeta A, et al. (2017) Assessment of long-term mortality in patients with complex coronary artery disease undergoing percutaneous intervention: Comparison of multiple anatomical and clinical prognostic risk scores. EuroIntervention 13: 1177-1184.
- Granger CB, Goldberg RJ, Dabbous O, et al. (2003) Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med 163: 2345-2353.
- Boukerche F, Hammou L (2018) Stratification du risque dans le SCA sans sus décalage du segment ST dans une population Oranaise: « Etude ORAN ». Journal of the Faculty of Medicine of Oran 2: 363-369.
- Prastaro M, Pirozzi E, GaibIazzi N, et al. (2017) Expert review on the prognostic role of echocardiography after acute myocardial infarction. J Am Soc Echocardiogr 30: 431-443.
- Doucet S, Jolicœur EM, Serruys PW, et al. (2019) Outcomes of left main revascularization in patients with acute coronary syndromes and stable ischemic heart disease: Analysis from the EXCEL trial. Am Heart J 214: 9-17.
- Schulman-Marcus J, Boden WE (2017) Early revascularization in NSTE-ACS: Insights from the ICTUS long-term follow-up. J Am Coll Cardiol 70: 1423-1424.
- Bhatt DL, Lopes RD, Harrington RA (2022) Diagnosis and treatment of acute coronary syndromes: A review. JAMA 327: 662-675.
Corresponding Author
Farouk Boukerche, Oran University Hospital Center, Oran, Algeria; Oran University 1, Ahmed BenBella, Oran, Algeria
Copyright
© 2022 Boukerche F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.