Usefulness of The Syntax Revascularization Index and The Concept of Reasonable Incomplete Revascularization In "All-Comer" Patients Undergoing Percutaneous Coronary Intervention
Abstract
Objectives: In particular settings, achieving complete coronary revascularization could be very challenging. The Syntax Revascularization Index (SRI) represents a useful tool to assess the degree of coronary revascularization in patients undergoing percutaneous coronary intervention (PCI). This study aimed to assess the prognostic usefulness of the SRI in an "all comer" cohort of patients undergoing PCI.
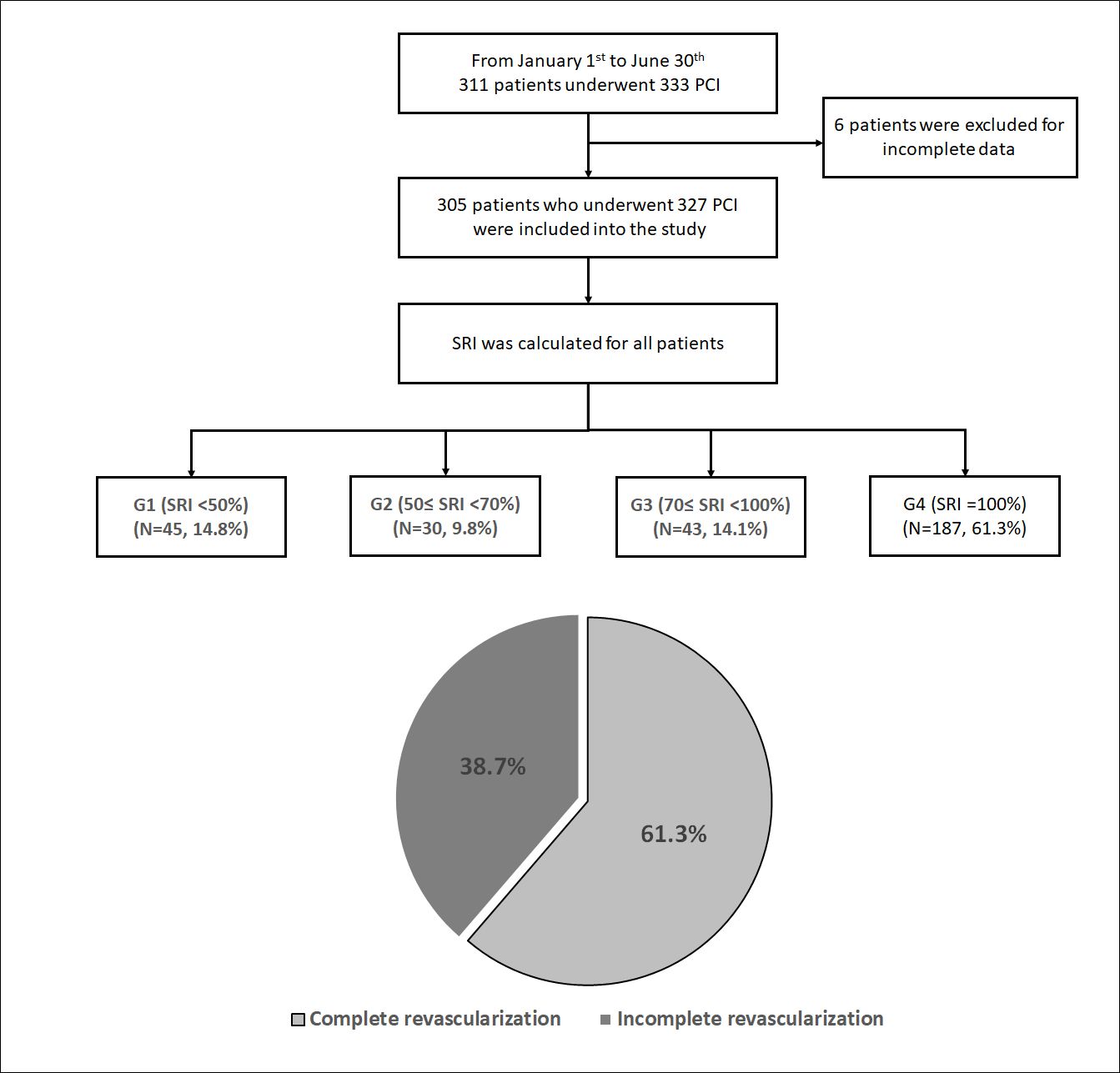
Methods: We performed a prospective observational single-center study, including 305 "all comers" patients, who underwent 327 PCI from January 1st to June 30th. According to the Syntax revascularization index (SRI), patients were subdivided into 4 subgroups: G1 (SRI < 50%), G2 (50% ≤ SRI < 70%), G3 (70% ≤ SRI < 100%) and G4 (SRI = 100%). One-year follow-up was performed in all patients. Major adverse cardiac events (MACE) were defined as the composite endpoint of cardiovascular death, non-fatal myocardial infarction and unplanned revascularization.
Results: The mean age was 62.3 ± 10.7 years, 80% were males. The distribution between SRI subgroups was as follows: G1 (n = 45, 14.8%); G2 (n = 30, 9.8%); G3 (n = 43, 14.1%), and complete revascularization (G4) (n = 187, 61.3%). In comparison with G4, 1-year survival free from MACE and cardiovascular death were lower in G1 [(94.6% vs. 86.7%; log-rank p = 0.048) and (96.8% vs. 88.9%; log-rank p = 0.022), respectively]. SRI satisfactorily predicted 1-year MACE and the optimal SRI cut-off was 75%. Reasonable incomplete revascularization (75% ≤ SRI < 100%) performed as well as complete revascularization in the settings of diabetes, elderly patients, left ventricular dysfunction and high-risk patients.
Conclusion: Our data showed the importance of complete revascularization in improving cardiovascular outcome. SRI ≥ 75% represented a reasonable target when complete revascularization is not achievable.
Keywords
Incomplete revascularization, Percutaneous coronary intervention, Syntax score, Syntax revascularization index
Introduction
Complete revascularization appears to be intuitively desirable in patients with coronary artery disease (CAD). Historically, coronary artery bypass grafting (CABG) surgery used to be the gold standard to reach complete revascularization [1,2]. Thanks to the advancements made in percutaneous revascularization techniques with the increased expertise of operators, percutaneous coronary intervention (PCI) has become the most widely used revascularization modality in patients with stable coronary artery disease (SCAD) and those with acute coronary syndromes (ACS) [3]. Although up to 50% of patients undergoing PCI for ACS have multivessel CAD [4,5], PCI has proven to be capable of obtaining high rates of complete revascularization [6]. However, achieving complete revascularization may be very challenging, particularly in patients with very complex CAD or in those at high risk due to severe comorbidities (elderly, diabetes, chronic kidney disease…). Furthermore, obstinately following "the dogma" of revascularization completeness might be harmful in some scenarios, increasing the risk for adverse events such as coronary perforations, stent thrombosis (ST) or lesion restenosis [7-9].
To overcome these difficulties, the concept of 'reasonable incomplete revascularization' using a derivative of the Syntax score (SS) called Syntax Revascularization Index (SRI) was developed [10]. SRI was demonstrated to predict major adverse cardiac events (MACE) after PCI with first-generation drug-eluting stents (DES) and an SRI ≥ 70% was considered as reasonable goal for patients with complex CAD [9]. More recently, Xu, et al. confirmed these findings using second generation DES, with an SRI cutoff of 85% [11].
In Tunisia, complete revascularization faces many difficulties such as the increasing prevalence of diabetes [12], the problematic percutaneous management of chronic total occlusions (CTO) and stent reimbursement issues. In addition, data regarding the impact of the degree of coronary revascularization on cardiovascular outcome are scarcely reported.
For all these reasons, we performed this prospective study aiming to evaluate the impact of the degree of coronary revascularization (as assessed by SRI) on mid-term cardiovascular outcome in a population of "all comer" Tunisian CAD patients undergoing PCI.
Material and Methods
Study population
We performed a prospective observational single-center study, at the Cardiology Department of Abderrahmen Mami Hospital, Ariana, Tunisia. From January 1st to June 30th 2017, "all comer" patients undergoing coronary angiography and showing significant CAD were screened. Patients who underwent PCI were included into the study; while those in whom either medical therapy or surgical revascularization were indicated, were not included. The exclusion criteria were the following: i) Age < 18 years; ii) Pregnant or lactating women; and iii) Incomplete data at enrollment.SS was evaluated, and SRI calculated in all patients. According to the degree of coronary revascularization, as assessed by SRI, patients were subdivided into 4 subgroups: G1 (SRI < 50%); G2 (50% ≤ SRI < 70%); G3 (70% ≤ SRI < 100%) and G4 (SRI = 100%). The study was carried out according to the principles of Helsinki declaration, and an informed written consent was obtained in all patients.
Percutaneous revascularization, medical therapy and score calculation
All PCI procedures were performed by 4 experienced operators according to current guideline recommendations [13]. Radial route was the preferred first-line access. Before PCI, patients received intra venous aspirin (250 mg), a loading dose (300-600 mg) of clopidogrel and a bolus of unfractionned heparin. The use of bare metal stents (BMS), DES or drug-eluting balloons (DEB) was dependent on the patient's insurance status, presence of diabetes, lesions' location and length, and operator's discretion. Only DES of second and third generation were used.
In ACS patients with multivessel disease, staged PCI was generally indicated: PCI of the culprit artery was performed during the index procedure, while the remaining lesions in the non-culprit arteries were treated either during the same hospitalization or within 30 days from the Index PCI. Multivessel disease patients referred for SCAD generally underwent multivessel PCI (of the selected lesions to be treated) within the same procedure.
Coronary lesions located within a segment with a reference diameter of ≥ 2.0 mm, were assessed by visual estimation and quantitative coronary analysis (QCA). They were considered significant if there was more than 70% reduction in the lumen diameter [≥ 50% in case of stenosis of proximal left anterior descending or left main (LM)].
Each coronary lesion considered to be significant was scored to yield the overall SS, which was calculated with the SS online calculator (http://www.syntaxscore.com/calculator/start.htm) [14]. For each patient, all angiographic variables involved in the calculation of SS were computed by the consensus of two independent experienced interventional cardiologists blinded to clinical data. In case of discordance a third interventional cardiologist's opinion was requested.
The residual Syntax score (rSS) being a measure of the relative completeness of revascularization, was calculated based on the remaining obstructive CAD after treatment with PCI [15]. The Delta Syntax score (DSS), representative of the burden of disease removed by PCI, was calculated by subtracting the rSS from the baseline SS [10]. Then the SRI, representative of the degree of revascularization after PCI, was calculated by dividing the DSS by the baseline SS and multiplying the result by 100 [(SRI = (DSS/SS) × 100] [10]. To calculate the baseline Syntax score II (SS II), we used the SS II online calculator (http://www.syntaxscore.com/calculator/start.htm) [16]. Complete revascularization was defined as SRI = 100%; otherwise it was considered to be incomplete. Reasonable incomplete revascularization was defined as an incomplete revascularization with an SRI above the determined ideal cut-off. Subjects with SS II ≥ 25 (median) were considered as high-risk patients.
When PCI was indicated, lesions to be treated or to be left to medical therapy among those considered to be significant, were selected by the consensus of the interventional cardiologists' team. No intra-coronary imaging or invasive functional assessment modalities were available during the study period. Since neither ticagrelor nor prasugrel are available in Tunisia, clopidogrel was the only anti P2Y12-receptor inhibitor prescribed in our population. After undergoing PCI, patients were discharged with dual anti platelet therapy (DAPT): aspirin 100-160 mg and a maintenance dose of clopidogrel (75 mg), daily. All variables were prospectively collected by two research fellows.
Follow-up
The follow up was performed by either clinical visit or phone call at 3, 6 and 12 months to document information about the occurrence of MACE or any hospitalization. Clinicians involved in the follow-up were blinded to PCI data. If a patient was hospitalized in another structure, data about that hospitalization was requested from the attending physician after the patient's consent.
Definitions and endpoints
The primary endpoint was the occurrence of MACE at 1-year follow-up. Secondary endpoints were components of the primary endpoint (cardiovascular death, non-fatal MI, unplanned revascularization, definite ST and hospitalization for cardiovascular reason at 1 year).
MACE were defined as the composite endpoint of cardiovascular death, non-fatal MI and unplanned revascularization. All deaths were considered of cardiovascular origin unless otherwise documented. MI was defined according to the consensus document on the third universal definition of MI [17]. Unplanned revascularization included any need for further revascularization during follow-up excluding PCI of non-culprit lesions scheduled within a staged revascularization strategy. Target lesion revascularization (TLR) was defined as a repeat revascularization (percutaneous or surgical) of the treated lesion. According to the Academic Research Consortium recommendations, definite ST was defined as the presence of a thrombus (at the angiogram) that originates in the stent or in the segment 5 mm proximal or distal to the stent [18]. ST was considered to be acute if occurring within the first 24 hours, subacute if > 24 hours to 30 days, and late if > 30 days to 1 year after stent implantation [19]. Hospitalization for cardiovascular reason was defined as the composite of hospitalization for coronary ischemic events, arrythmia, heart failure and stroke.
Statistical analysis
Continuous variables were presented as mean ± SD and were compared using the Student unpaired t-test. Categorical variables were presented as counts and percentages and compared using the chi2-test when appropriate (expected frequency > 5); otherwise, the Fisher exact test was used.
The independent predictors of incomplete revascularization were identified using a stepwise logistic regression. At univariate analysis the following variables were tested: Age ≥ 75 years, male gender, current smoking, diabetes, hypertension, PAD, prior stroke, prior MI, prior PCI, prior CABG, CKD, ACS, LVEF ≤ 40%, multivessel disease, intra-stent restenosis, LM disease, CTO, SS > 22, SS II ≥ 25 (median) and medical insurance. Those with p < 0.1 were included in a multivariate model.
Event-free survival during follow-up was evaluated according to the Kaplan-Maier method [20]. The difference between the different subgroups [(complete vs. incomplete revascularization) and (G1, G2 and G3 vs. G4)] was assessed by log-rank p.
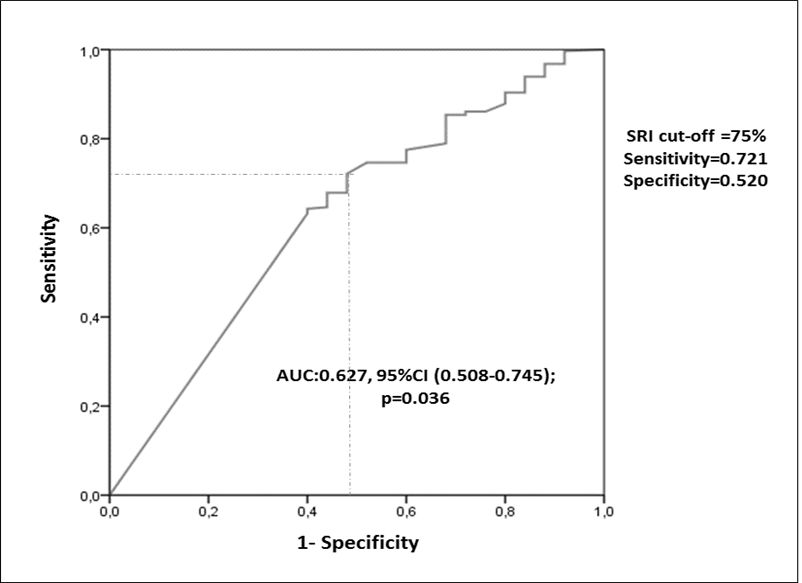
Receiver Operating Characteristic (ROC) curve and area under the curve (AUC) were used to assess discrimination of SRI and to identify its ideal cut-off to predict MACE at 1 year [21].
Stepwise Cox regression was then performed to identify independent predictors of 1-year MACE. The parameters included in univariate analysis were the following: age ≥ 75 years, male gender, current smoking, diabetes, hypertension, PAD, prior stroke, prior MI, prior PCI, prior CABG, CKD, ACS, LVEF ≤40%, multivessel disease, intra-stent restenosis, LM disease, CTO, SS > 22, SS II ≥ 25 (median), exclusive use of DES, complete revascularization and SRI ≥ ideal cut-off. Those with p < 0.1 were included in a multivariate model.
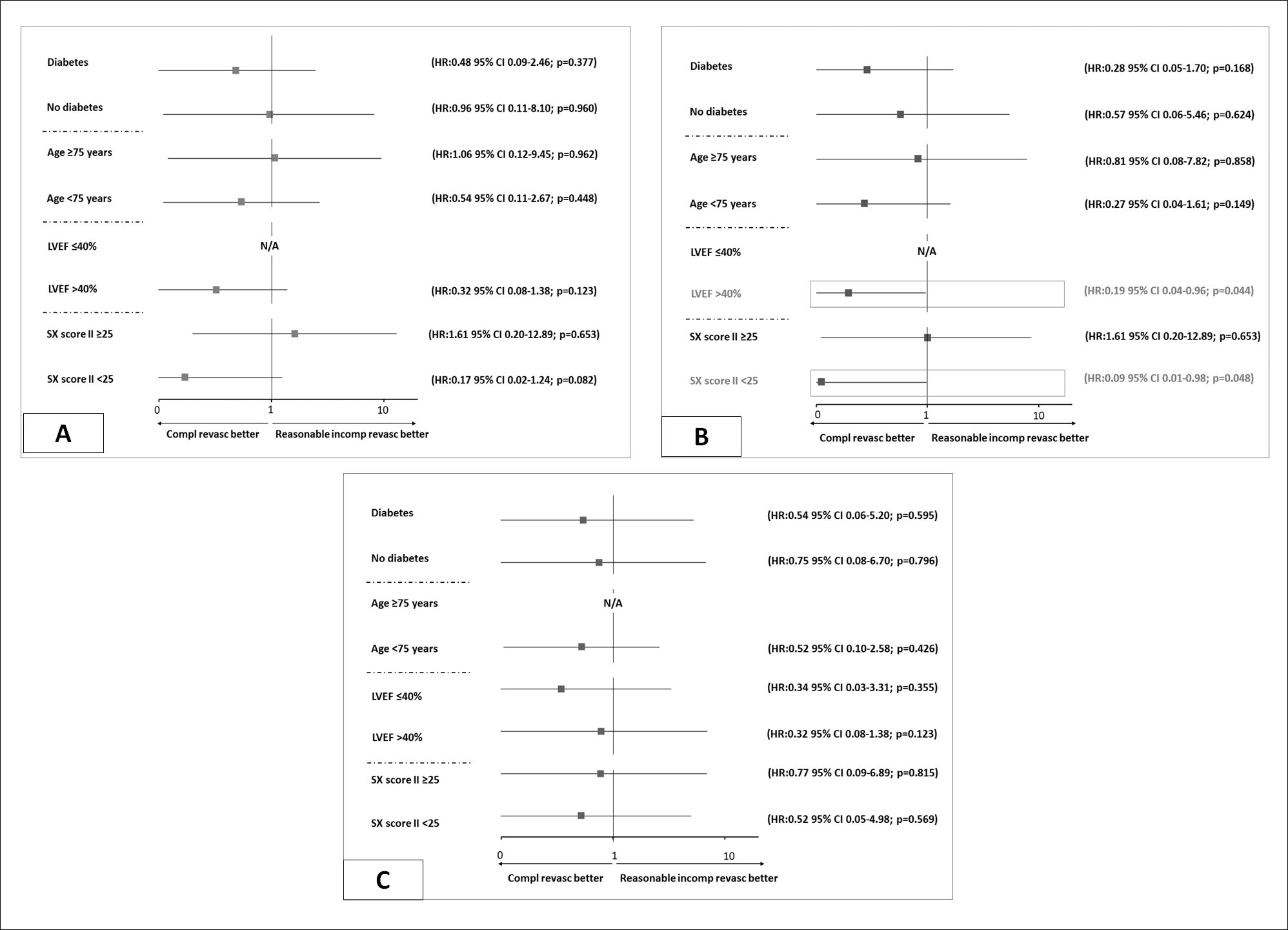
Finally, univariate Cox regression was employed to compare reasonable incomplete revascularization (ideal SRI cut-off ≤ SRI < 100%) vs. complete revascularization in the following specific subgroups: diabetics and non-diabetics patients; age ≥ 75 years and age < 75 years; LVEF ≤ 40% and LVEF > 40%; SSII ≥ 25 and SSII < 25.
In all cases p values < 0.05, were considered statistically significant. All data were processed using SPSS version 21.0 (SPSS, Chicago, Illinois).
Results
From January 1st to June 30th, 311 "all comer" patients underwent 333 PCI at our centre. Six patients were excluded because of incomplete data. Then, a total of 305 patients, who underwent 327 PCI, were finally included into the study. Figure 1 illustrates the flow chart of the study population. According to the revascularization degree, the distribution between SRI subgroups was as follows: (G1, SRI < 50%) (n = 45, 14.8%); (G2, 50% ≤ SRI < 70%) (n = 30, 9.8%); (G3, 70% ≤ SRI < 100%) (n = 43, 14.1%), and complete revascularization (G4, SRI = 100%) was obtained in 187 patients (61.3%).
Patients' characteristics and independent predictors of incomplete revascularization
Table 1 summarizes the clinical baseline characteristics of the study population. The mean age was 62.3±10.7 years, and 80% were males. Diabetes and hypertension were prevalent in 55.7% and 47.5% of cases, respectively while 37% and 35.7% of patients were current smokers and had dyslipidemia, respectively. There were significant differences between the rates of elderly patients, those with a history of MI or a history of CABG among different SRI groups (Table 1).
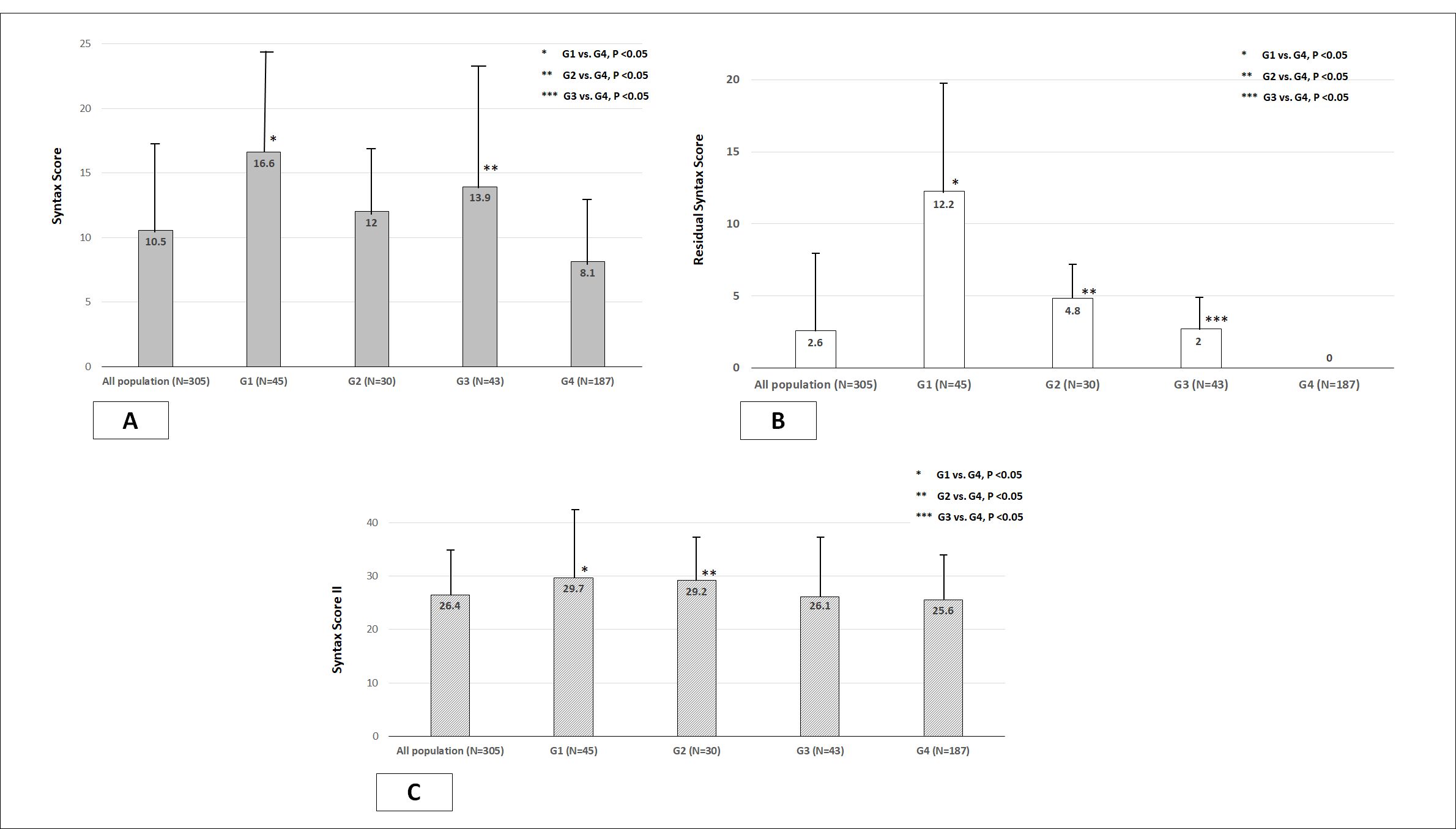
Table 2 summarizes the angiographic and procedural characteristics of the study population. The mean SS was 10.5 ± 7.2 and 10.2% of patients had SS > 22. The mean SS II score was 26.6 ± 9.4 (Figure 2). There were significant differences between the prevalence of multivessel disease, LM disease and CTOs between the different SRI groups (Table II). In incompletely revascularized patients, the SS was higher (particularly in G1 and G3) as well as SS II (particularly in G1 and G2), comparatively with complete revascularization subgroup (G4) (Figure 2).
The multivariate analysis identified SS > 22 [Odds ratio (OR): 2.64, 95% confidence interval (CI) 1.01-7.05; p = 0.048)] and multivessel disease (OR: 14.95, 95% CI 8.11-27.58; p < 0.001) as the independent predictors of incomplete revascularization (Table 3).
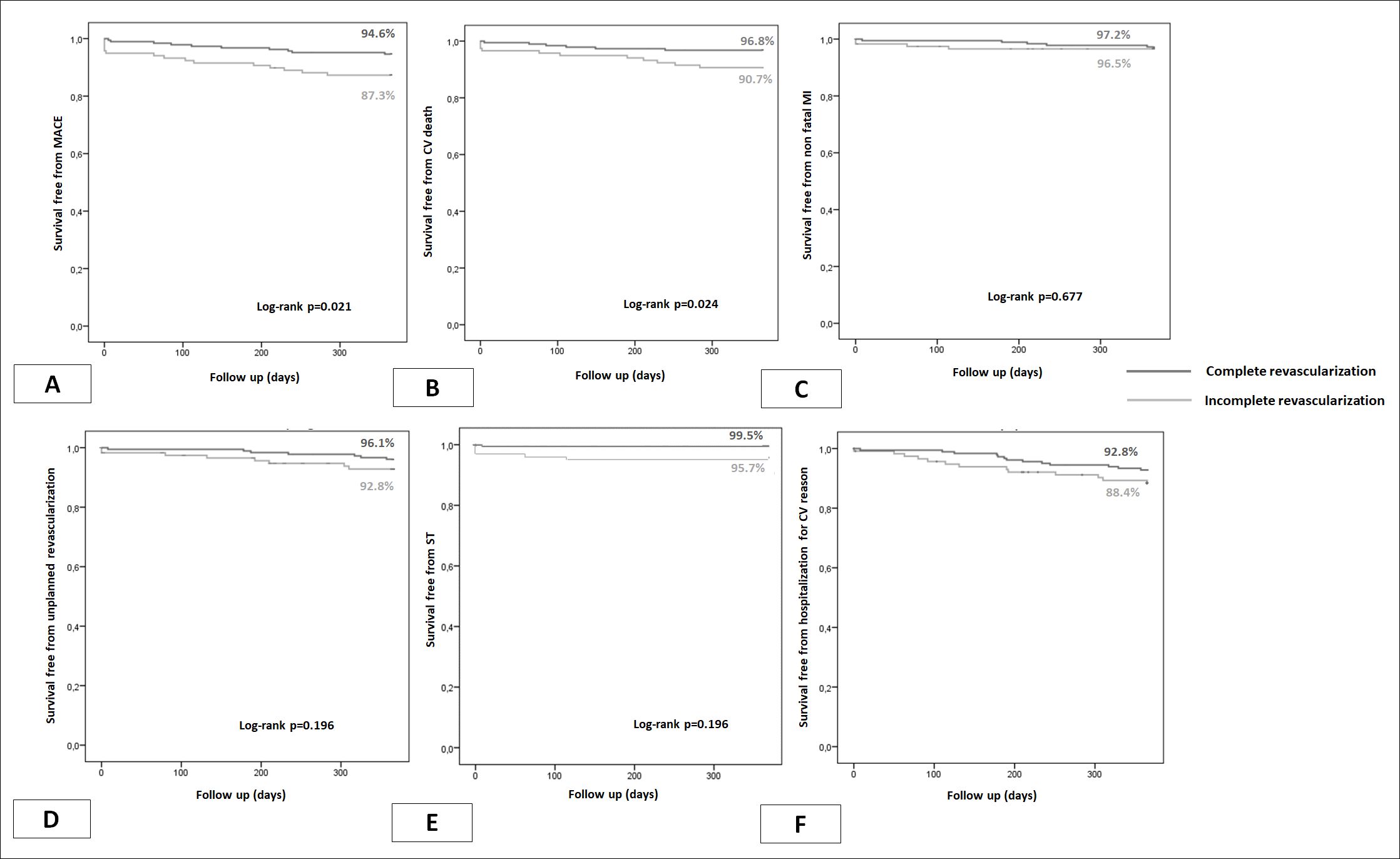
One-year clinical outcome and the predictive value of SRI
One-year clinical outcome was obtained in all patients. Overall, 25 patients (8.2%) experienced MACE at 1 year (Table 4). Patients with complete revascularization experienced less cardiovascular deaths (3.2% vs. 9.3%; p = 0.023), ST (4.2% vs. 0.5%; p = 0.023) and MACE (5.3% vs. 12.7%; p = 0.022) in comparison with patients incompletely revascularized (Table 4). At 1-year follow up, survival free from MACE was significantly reduced (87.3% vs. 94.6%; p = 0.021) as well as survival free from cardiovascular death (90.7% vs. 96.8%; p = 0.024) and definite ST (99.5% vs. 95.7; p = 0.023) in patients who underwent incomplete revascularization in comparison with whom completely revascularized (Figure 3). No difference was observed concerning hospitalization for cardiovascular reason (Figure 3).
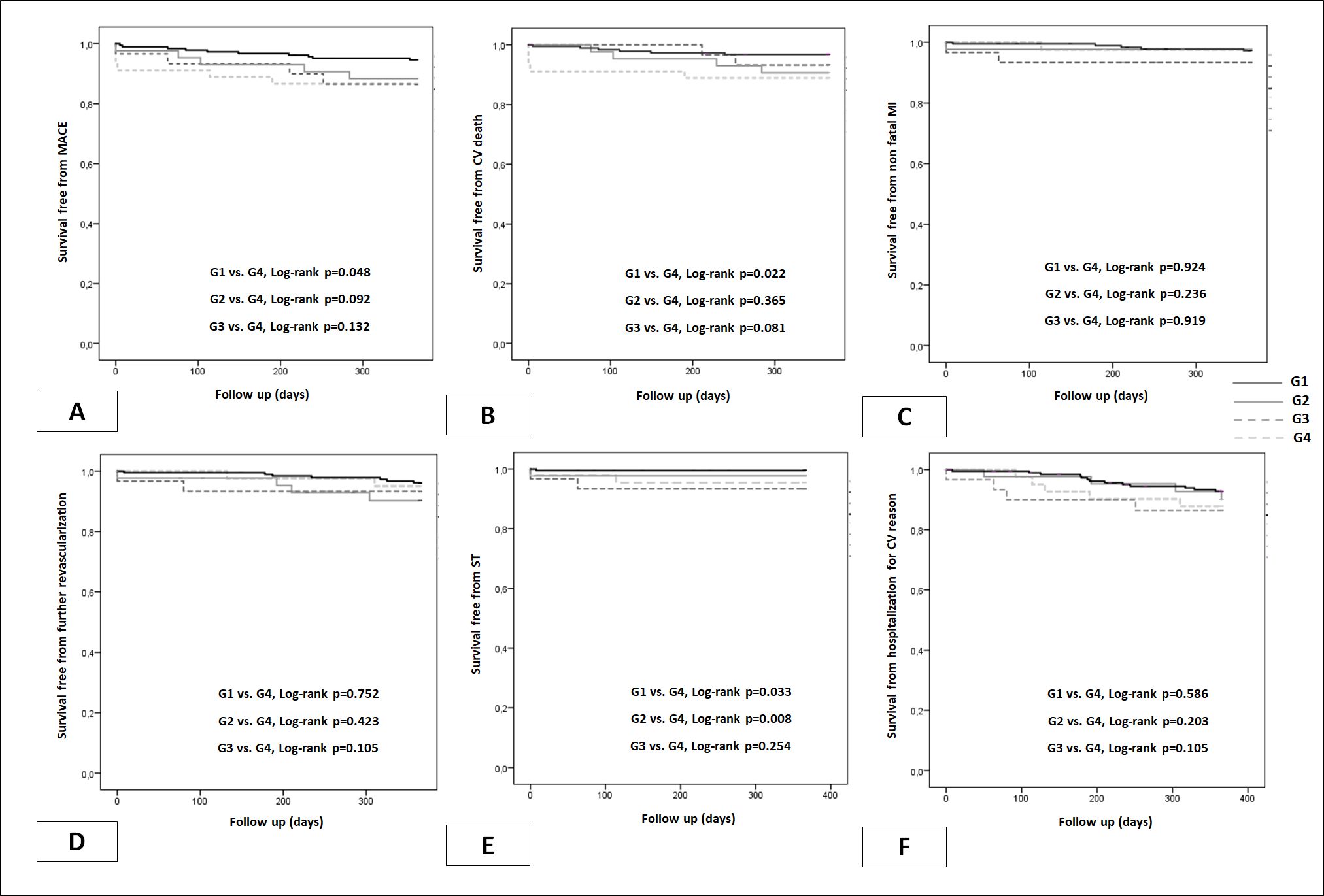
Table 5 summarizes 1-year clinical outcome according to SRI subgroups. Significant differences were observed between different SRI subgroups in terms of cardiovascular deaths, definite ST and MACE (Table 5). KM analysis also showed significant differences between different SRI groups in terms of MACE, cardiovascular deaths and ST free survivals (Figure 4).
ROC curve analysis revealed that SRI predicted the occurrence of 1-year MACE (AUC: 0.627, 95%CI significantly 0.508-0.745; p = 0.036) (Figure 5). The optimal SRI cut-off was 75% for a sensitivity of 0.721 and a specificity of 0.520.
Multivariable Cox regression identified prior stroke [Hazard ratio (HR): 6.78, 95% CI 1.30-35.4; p = 0.023)], ACS (HR: 4.60, 95% CI 1.41-15.02; p = 0.012), LVEF ≤ 40% (HR: 2.93, 95% CI 1.04-8.26; p = 0.042), SS II ≥ 25 (HR: 3.65, 95% CI 1.14-11.71; p = 0.029) and SRI ≥ 75% (HR: 0.41, 95% CI 0.16-0.99; p = 0.048) as independent predictors of MACE at 1-year follow up (Table 6).
Complete vs. reasonable incomplete revascularization in particular subsets of patients
Reasonable incomplete revascularization (75 ≤ SRI < 100%) was obtained in 35 patients (11.5%). Figures 6 illustrated the comparison between complete and reasonable incomplete revascularization in terms of MACE (Figure 6A), cardiovascular death (Figure 6B) and unplanned revascularization (Figure 6C) at 1 year, respectively. In diabetic and elderly patients, achieving complete revascularization had no benefit at 1 year in comparison with reasonable incomplete revascularization (all p NS). In patients with impaired LVEF, no difference in 1-year outcome was observed according to the degree of revascularization; while in patients with LVEF > 40%, although no difference was observed in terms of overall MACE occurrence, complete revascularization protected against CV death at 1 year follow up (HR: 0.19 95% CI 0.04-0.96; p = 0.044), in comparison with reasonable incomplete revascularization (Figure 6B). In high risk patients (SS II ≥ 25), achieving complete revascularization did not influence 1-year outcome (all p NS); whereas in lower risk patients (SS II < 25), complete revascularization was shown to reduce CV death in comparison with reasonable incomplete revascularization (HR: 0.09 95% CI 0.01-0.98; p = 0.048) (Figure 6B).
Discussion
In the current study, we assessed for the first time, the added value of SRI on mid-term clinical outcome in a prospective contemporary cohort of "real world" all comer patients undergoing PCI. The major findings can be summarized as follows: a) Complete revascularization was obtained in 61.3% of patients, b) The independent predictors of incomplete revascularization were multivessel disease and SS > 22, c) SRI satisfactorily predicted mid-term outcome and SRI ≥ 75% protected against 1-year MACE, d) reasonable incomplete revascularization (75 ≤ SRI < 100) led to similar mid-term outcome than complete revascularization in elderly, diabetic and high-risk patients.
According to clinical characteristics, our study population showed a high cardiovascular risk profile. Indeed, diabetes was prevalent in more than half our patients (55.7%). This prevalence is much higher than that in other all comer PCI studies and largely above the Tunisian average (15.1%) [12,22]. Such differences might be due to the close relationship between diabetes and CAD and to the fact that diabetes is under diagnosed in the Tunisian population and can often be firstly diagnosed following a coronary event. The prevalence of other risk factors [smoking (37%), hypertension (47.5%), dyslipidemia (35.7%) and overweight (mean BMI 26.4 ± 2.8)] further confirm the high-risk profile of our population.
The mean age of our patients was 62.3 ± 10.7, while elderly (age ≥ 75) represented 13.4%. Interestingly, the elderly proportion in all incomplete revascularization SRI subgroups was higher than that in complete revascularization subgroup. Although it was not identified as an independent predictor at multivariate analysis, age ≥ 75 was associated with incomplete revascularization at univariate analysis. The reluctance of interventional cardiologists to perform long and cumbersome procedures in older patients, consequently decreasing the chances of achieving complete revascularization, could explain this latter finding.
There were also significantly more patients with CKD in the SRI subgroups G2 and G3, in comparison with G4. Patients with CKD are more likely to develop contrast induced nephropathy [13]. Therefore, interventionalists tend to reduce procedural time and contrast exposure in these patients. Achieving complete revascularization is consequently more challenging.
One of the originalities of our study is that we included both single and multivessel CAD in comparison with other registries focusing on the SRI concept which only included multivessel disease patients [4,10]. We believed this can better illustrate real life practice. Indeed, the presence of several lesions (proximal, mid and/or distal) within the same vessel or in significant side branches, in a single vessel disease patient could also challenge the completeness of revascularization. Multivessel disease was encountered in almost half of our patients (47.9%) and strongly predicted incomplete revascularization (OR 14.95; CI 8.11-27.58; p < 0.001). The mean SS score was 10.5 ± 7.2 and 1/10 (10.2%) of patients had a SS > 22. The fact that SS > 22 independently predicted incomplete revascularization further highlights that the more complex and extensive is CAD the lower are the chances to obtain complete revascularization.CTO, a well-known predictor of incomplete revascularization in literature [23], was present in only 9.5% of patients. This low prevalence comparatively with other registries [24], might be explained by the fact that most CTO patients were either referred for surgical revascularization (particularly those with multivessel disease) or left on medical therapy, and then not included in our study. Furthermore, only 1/5 of CTO patients enrolled underwent a PCI attempt for their CTO. Although CTO was associated with incomplete revascularization in univariate analysis, it did not appear in the multivariate model.
In the ARTS-II trial, Sarno, et al. found no significant difference in 5-year survival without MACE between patients with complete and incomplete revascularization undergoing PCI (with first-generation sirolimus DES) or CABG [25]. Interestingly, in patients incompletely revascularized by PCI, the authors revealed a significantly lower MACE survival in the higher SS tertile compared with the low (HR 0.56, 95% CI 0.32-0.96, p = 0.04) and intermediate (HR 0.50, 95% CI 0.28-0.91, p = 0.02) tertiles, while survival between the low and intermediate SS tertiles was not significantly different.
The Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial could be considered as the ultimate trial of incomplete revascularization in SCAD patients [26]. Although this trial failed to show a clinical benefit for routine PCI in these low risk patients, its nuclear substudy highlighted the prognostic impact of the residual ischemic burden [27]. Indeed, ≥ 10% reversible ischemia was associated with adverse 5-year mortality when left on medical therapy alone.
Nowadays in the era of second-and third-generation DES, MACE driven by TLR considerably decreased [13]. This tends to encourage interventional cardiologists to target more complete revascularization in their patients.
In our study, incomplete revascularization was associated with significantly lower survival free from MACE and cardiovascular death. These findings were in accordance with the results of a meta-analysis of 35 randomized and observational studies including 89,883 PCI and CABG patients [22]. Complete revascularization was associated with lower long-term mortality, MI and repeat coronary revascularization [22]. Interestingly, ST was more often experienced by our incompletely revascularized patients. Intuitively, complete revascularization tends to require more and longer stents. In our study, no difference was found between G4 and all incomplete revascularization subgroups in terms of stent numbers and length (all p NS). Hence, the higher rate of ST in patients with incomplete revascularization might be due to the higher complexity (length, calcifications, tortuosity) of their treated lesions preventing optimal stent apposition.
Initially applied using rSS [28], the concept of reasonable incomplete revascularization has been extended to the SRI. In patients with de novo 3-vessel CAD or unprotected LM disease, Généreux et al. found that 5-year outcomes were inversely proportional to the SRI [10]. The Youden index identified an SRI cut-off of < 70% for prediction of 5-year all-cause mortality (HR: 4.13, 95% CI 2.79-6.11; p < 0.0001). Hence, an SRI ≥ 70% was considered as a reasonable goal for patients with complex CAD in whom complete revascularization is not always possible.
In our study SRI was also found to satisfactorily predict 1-year cardiovascular outcome (AUC = 0.627; p = 0.036). Our data showed that although no difference was observed in terms of MACE, MI, ST and hospitalization for cardiovascular reason, patients with 70 ≤ SRI < 100% (G3) tend to have lower survival free from CV death (p = 0.081) and significantly higher rate of non-TLR unplanned revascularization (7% vs. 1.6%; p = 0.046). Hence, the cut-off of 70% (generated in a complex CAD North-American and European cohort) could not be applicable to our Tunisian all-comer population.
In our cohort, ROC curve analysis identified 75% as the ideal SRI cutoff (sensitivity = 0.721; specificity = 0.520). Importantly, SRI ≥ 75% (i.e. complete and reasonable incomplete revascularization) protected against 1-year MACE (HR: 0.41, 95%CI 0.16-0.99; p = 0.048), while complete revascularization (by itself) did not appear to independently predict 1-year MACE on multivariate Cox analysis. The other predictors of mid-outcome were prior stroke, LVEF ≤ 40%, ACS and SS II ≥ 25 as reported in previous studies [29-32].
In the Registry to Evaluate Safety and Effectiveness of Everolimus Drug Eluting Stent for Coronary Revascularization (SEEDS), Xu, et al. evaluated the impact of the revascularization degree on 2-year MACE in Asian complex CAD patients [11]. In accordance with our results, 2-year mortality and MACE were higher in lower SRI subgroup (< 50%) [11]. The SRI predicted mortality and MACE at 2 years and the optimal SRI cut-off in this latter population was as high as 85% [11]. This difference in SRI cut-offs came mainly from the fact that our population had considerably less complex and extensive CAD than the SEEDS population. Indeed, when restricted to patients with low SS, the optimal SRI cut-off of the SEEDS registry decreased to 70-75% [11].
In our study, reasonable incomplete revascularization (75 ≤ SRI < 100) was compared with complete revascularization in 4 different clinical scenarios: diabetes, elderly patients, impaired LVEF and high-risk patients (as assessed by SS II).
In our population, in both diabetic and non-diabetic patients, complete revascularization did not provide any clinical benefit at 1-year follow-up. A post hoc nonrandomized analysis of the completeness of revascularization included 751 patients treated by either CABG or PCI (264 and 487, respectively) [29]. No difference was observed in diabetic patients receiving reasonable incomplete revascularization vs. those completely revascularized (HR: 1.51, 95%CI 0.93-2.47, p NS) [29]. Hence, in diabetic patients treated by PCI, complete revascularization seemed to not have a clinical benefit in comparison with reasonable incomplete revascularization, allowing the assumption of leaving a "reasonable'' ischemic burden on medical therapy alone, especially in case of extensive and diffuse CAD.
In a substudy of the SHINANO registry including elderly patients (mean age of 81 years), Harada et al. reported a 51.2% complete revascularization rate [30]. The investigators found that MACE incidence by survival analysis was significantly higher in the incomplete revascularization group (21.1% vs. 7.4%, p < 0.001) at 1-year, concluding that complete revascularization appears to suppress midterm ischemic events in elderly patients. Differently, in 502 ACS patients aged ≥ 75 (with a complete revascularization rate of 40.4%), Chen, et al. [33] did not find significant differences in cumulative survival and event-free survival rates between incomplete and complete revascularization. The impact of reasonable incomplete revascularization was not assessed in the 2 latter studies. In our patients aged more than 75 years (n = 41), we obtained complete revascularization in 48.7% of cases. Reasonable incomplete revascularization showed the same performance than complete revascularization in terms of MACE and cardiovascular death at 1-year. Indeed, in elderly patients, treating all lesions can be challenging not only due to the complexity of CAD but also to the associated comorbidities. Furthermore, this subset of patients has generally a relatively decreased physical activity status. Thus, only targeting lesions with prognostic importance (subtending large myocardial territories) in a reasonable incomplete revascularization fashion, could represent a valuable approach to balance the benefit/risk ratio.
In our population, 40(13.1%) patients had a LVEF ≤ 40%. Complete revascularization was achieved in 60% of these cases. No difference in unplanned revascularization was observed between complete and reasonable incomplete revascularization (HR 0.34, 95%CI 0.03-3.31, p = 3.55). Conversely, we showed that in the presence of mildly impaired or preserved LVEF (> 40%), complete revascularization should be targeted as it protected against cardiovascular death in comparison with reasonable incomplete revascularization. Similarly, when the risk was low (SSII < 25), complete revascularization remains the most appropriate strategy to reduce mid-term cardiovascular mortality, while no benefit of complete revascularization was demonstrated in high risk patients, emphasizing the safety and efficiency of a reasonable incomplete revascularization approach in high risk patients (SS II ≥ 25).
Study limitations
Our study has some limitations. First, its single-center design and the relatively limited number of patients do not allow the generalization of the results. Nonetheless, it represents the first study in North Africa focusing on the impact of the degree of coronary revascularization. Second, in the absence of FFR assessment, only an anatomical definition was used to evaluate the revascularization completeness. Third, coronary lesions faced in our study were less complex than in other reports (as assessed by SS). However, it reflects a "real life" Tunisian CAD population treated in our everyday cathlab practice. Fourth, the impact of prescribed medical therapy as well as patient's compliance (particularly to DAPT), was not assessed. Fifth, assessing the effects of the revascularization degree on symptoms and quality of life was beyond the scope of the current study. Sixth, the low number of subjects in the evaluated subgroups makes difficult to generalize the results. Finally, longer outcome is required to better understand the real impact of coronary revascularization degree on cardiovascular outcome.
Conclusion
Our results further confirm the importance of complete revascularization in CAD patients in insuring a better cardiovascular outcome. However, when such a target is not achievable, the concept of reasonable incomplete revascularization relying on SRI (≥ 75%) appears to be a valuable option, particularly in the setting of diabetes, age ≥ 75, LVEF ≤ 40% and SS II ≥ 25. Larger multicenter studies with longer follow up are needed to better identify the impact of a reasonable incomplete coronary revascularization in particular subsets in whom complete revascularization can be challenging.
Conflicts of Interest
None to declare.
References
- Ong AT, Serruys PW, Mohr FW, et al. (2006) The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) study: Design, rationale, and run-in phase. Am Heart J 151: 1194-1204.
- van den Brand MJ, Rensing BJ, Morel MA, et al. (2002) The effect of completeness of revascularization on event-free survival at one year in the ARTS trial. J Am Coll Cardiol 39: 559-564.
- Iqbal J, Serruys PW, Taggart DP (2013) Optimal revascularization for complex coronary artery disease. Nat Rev Cardiol 10: 635-647.
- Genereux P, Campos CM, Yadav M, et al. (2015) Reasonable incomplete revascularisation after percutaneous coronary intervention: The SYNTAX Revascularisation Index. EuroIntervention 11: 634-642.
- Sorajja P, Gersh BJ, Cox DA, et al. (2007) Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur Heart J 28: 1709-1716.
- Nagaraja V, Ooi SY, Nolan J, et al. (2016) Impact of incomplete percutaneous revascularization in patients with multivessel coronary artery disease: A systematic review and meta-analysis. J Am Heart Assoc 5: e004598.
- Genereux P, Kumsars I, Lesiak M, et al. (2015) A randomized trial of a dedicated bifurcation stent versus provisional stenting in the treatment of coronary bifurcation lesions. J Am Coll Cardiol 65: 533-543.
- Mehran R, Claessen BE, Godino C, et al. (2011) Long-term outcome of percutaneous coronary intervention for chronic total occlusions. JACC Cardiovasc Interv 4: 952-961.
- Genereux P, Madhavan MV, Mintz GS, et al. (2014) Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes. Pooled analysis from the HORIZONS-AMI (Harmonizing outcomes with revascularization and stents in acute myocardial infarction) and ACUITY (Acute catheterization and urgent intervention triage strategy) TRIALS. J Am Coll Cardiol 63: 1845-1854.
- Genereux P, Campos CM, Farooq V, et al. (2015) Validation of the SYNTAX revascularization index to quantify reasonable level of incomplete revascularization after percutaneous coronary intervention. Am J Cardiol 116: 174-186.
- Xu B, Bettinger N, Guan C, et al. (2017) Impact of completeness of revascularization in complex coronary artery disease as measured with the SYNTAX revascularization index: An SEEDS Substudy. Catheter Cardiovasc Interv 89: 541-548.
- Ben Romdhane H, Ali SB, Aissi W, et al. (2014) Prevalence of diabetes in Northern African countries: the case of Tunisia. BMC Public Health14: 86.
- Authors/Task Force m, Windecker S, Kolh P, et al. (2014) 2014 ESC/EACTS Guidelines on myocardial revascularization The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Euro Heart J 35: 2541-2619.
- Sianos G, Morel M, Kappetein A, et al. (2005) The SYNTAX Score: An angiographic tool grading the complexity of coronary artery disease. 1: 219-227.
- Malkin CJ, George V, Ghobrial MS, et al. (2013) Residual SYNTAX score after PCI for triple vessel coronary artery disease: Quantifying the adverse effect of incomplete revascularisation. EuroIntervention 8: 1286-1295.
- Farooq V, van Klaveren D, Steyerberg EW, et al. (2013) Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet 381: 639-650.
- Thygesen K, Alpert JS, Jaffe AS, et al. (2012) Third universal definition of myocardial infarction. J Am Coll Cardiol 60: 1581-1598.
- Claessen BE, Henriques JPS, Jaffer FA, et al. (2014) Stent thrombosis. A clinical perspective. JACC Cardiovasc Interv 7: 1081-1092.
- Cutlip DE, Windecker S, Mehran R, et al. (2007) Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 115: 2344-2351.
- Jager KJ, van Dijk PC, Zoccali C, et al. (2008) The analysis of survival data: The Kaplan-Meier method. Kidney Int 74: 560-565.
- Hajian-Tilaki K (2013) Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med 4: 627-635.
- Garcia S, Sandoval Y, Roukoz H, et al. (2013) Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: A meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol 62: 1421-1431.
- Head SJ, Mack MJ, Holmes JDR, et al. (2012) Incidence, predictors and outcomes of incomplete revascularization after percutaneous coronary intervention and coronary artery bypass grafting: A subgroup analysis of 3-year SYNTAX data†. Eur J CardioThorac Surg 41: 535-541.
- Sianos G, Werner GS, Galassi AR, et al. (2012) Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention 8: 139-145.
- Sarno G, Garg S, Onuma Y, et al. (2010) Impact of completeness of revascularization on the five-year outcome in percutaneous coronary intervention and coronary artery bypass graft patients (from the ARTS-II study). Am J Cardiol 106: 1369-1375.
- Boden WE, O'Rourke RA, Teo KK, et al. (2007) Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 356: 1503-1516.
- Shaw LJ, Berman DS, Maron DJ, et al. (2008) Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: Results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 117: 1283-12891.
- Farooq V, Serruys PW, Bourantas CV, et al. (2013) Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation 128: 141-151.
- Schwartz L, Bertolet M, Feit F, et al. (2012) Impact of completeness of revascularization on long-term cardiovascular outcomes in patients with type 2 diabetes mellitus: results from the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D). Circ Cardiovasc Interv 5: 166-173.
- Harada M, Miura T, Kobayashi T, et al. (2017) Clinical impact of complete revascularization in elderly patients with multi-vessel coronary artery disease undergoing percutaneous coronary intervention: A sub-analysis of the SHINANO registry. Int J Cardiol 230: 413-419.
- Sohn GH, Yang JH, Choi S-H, et al. (2014) Long-term outcomes of complete versus incomplete revascularization for patients with multivessel coronary artery disease and left ventricular systolic dysfunction in drug-eluting stent era. J Korean Med Sci 29: 1501-1506.
- Salvatore A, Boukhris M, Giubilato S, et al. (2016) Usefulness of SYNTAX score II in complex percutaneous coronary interventions in the setting of acute coronary syndrome. J Saudi Heart Assoc 28: 63-72.
- Chen J, Xue Q, Bai J, et al. (2012) Incomplete revascularization in the drug eluting stent era permits meaningful long-term (12-78 months) outcomes in patients = 75 years with acute coronary syndrome. J Geriatr Cardiol 9: 336-343.
Corresponding Author
Marouane Boukhris MD, FESC, Faculty of Medicine of Tunis, University Tunis El Manar, Tunis, Tunisia; CHU Dupuytren, Limoges, France.
Copyright
© 2022 Najar H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.