Influence of Concurrently-Existed Factors on Serum N-Terminal Pro-B-Type Natriuretic Peptide Level in Heart Failure
Abstract
The serum level of N-terminal pro-b-type natriuretic peptide (NT-pro BNP) would be affected by some other factors. To recognize the influential factors of serum NT-pro BNP level is very important for making accurate diagnosis and outcome-prediction. The study aimed to evaluate the influence of concurrently-existed factors on serum NT-pro BPN levels among patients with heart failure. This retrospective study was conducted enrolling adult patients with hospitalization-requiring heart failure (HF) from January 2011 to December 2013. The enrolled patients were categorized into four groups according to their initial serum NT-pro BNP level. Then we compared the basic characteristics and clinical parameters, and further clarified the influential factors and their effects on serum NT-pro BNP level. A total of 269 patients were enrolled and categorized into four groups. Several basic and clinical factors were found with significant differences among the four groups and were put into the regression path model. Then we disclosed six factors, including heart rate (HR), left ventricular ejection fraction (LVEF), New York Hospital Association Functional Classification, body mass index, hemoglobin, and estimated glomerular filtration rate which exhibited their direct influences to serum NT-pro BNP level. Besides, hemoglobin, LVEF, and HR also served as mediators leading to indirect effects on serum NT-pro BNP level. In conclusion, the current study identified several factors that could directly or indirectly affect the serum NT-pro BNP level. An index using "multi-factors adjusted serum NT-pro BNP level" may be further developed as a better tool for screening and prognosis-predicting in patients with HF.
Keywords
Body mass index, Estimated glomerular filtration rate, Heart failure, Heart rate, Hemoglobin, Left ventricular ejection fraction, NT-pro BNP
Abbreviations
ACEI: Angiotensin converting enzyme inhibitors; Af: Atrial fibrillation; AGFI: Adjusted Goodness-of-Fit Index; Ald.-blocker: Aldosterone receptor blocker; ANOVA: Analysis of variance; ARB: Angiotensin receptor blocker; BMI: Body mass index; BT: Body temperature; CI: Confidence interval; CFI: Comparative Fit Index; CLD: Chronic lung disease; CMIN/DF: Normal Chi-Square Fit Index; DBP: Diastolic blood pressure; DCM: Dilated cardiomyopathy; DM: Diabetes mellitus; eGFR: Estimated glomerular filtration rate; EKG: Electrocardiogram; GFI: Goodness-of-Fit Index; Hb: Hemoglobin; HCVD: Hypertensive Heart Disease; HF: Heart failure; HFpEF: Heart failure with preserved ejection fraction; HFrEF: Heart failure with reduced ejection fraction; HR: Heart rate; HTN: Hypertension; ICD: International Classification of Diseases; IHD: Ischemic heart disease; K: Potassium; LVEF: Left ventricular ejection fraction; Na: Sodium; NFI: Normed Fit Index or Bentler Bonett Index; NT-pro BNP: N-terminal pro-b-type natriuretic peptide; NYHA Fc: New York Hospital Association Functional Classification functional classification; RMSEA: Root Mean Square Error of Approximation; RR: Respiratory rate; SBP: Systolic blood pressure; SD: Standard deviation; SRMR: Standardized root mean square residua; VHD: Valvular heart disease
Introduction
Heart failure (HF) is an essential clinical entity all over the world, of which both incidence and prevalence rates are increasing when the population is aging [1]. In the United States, approximately 8-16 of every 1,000 persons in the population over 65-years have HF, and 20% of them have ever been hospitalized due to HF [1]. In Taiwan, cardiac disease is among the top three leading causes of death. Cardiac disease and more detailed entity, HF, are accountable for 11% and 2%, respectively, of the total number of deaths in 2012 [2]. HF is a chronic, complicated, and progressive clinical syndrome, in which the whole clinical course is challenging to be explained by a simple definition or mechanism. Currently, N-terminal pro-b-type natriuretic peptide (NT-pro BNP) is peptides secreted by the cardiac ventricles in response to the volume expansion and pressure load and is recommended for the diagnostic tool of HF [3].
Nonetheless, the serum level of NT-pro BNP would also be affected by, besides HF itself, some other factors such as renal dysfunction, anemia, or obesity [4-10]. To recognize these affecting factors and affected the magnitude of NT-pro BNP is very important regarding the accuracy of diagnosis and outcome-predicting. However, most of the previous studies [4-10] investigating the influence of some factors on serum NT-pro BNP level were conducted in a one-on-one manner that did not take the complicated associations with other influential factors into account. Moreover, this is less likely to be a real-world practice scenario. Thus we conducted this study to evaluate the influence of concurrently-existed factors on serum NT-pro BPN level and further clarify the direct and indirect effects of certain influential factors on affecting serum NT-pro BNP level in the real-world practice situation.
Material and Methods
Ethical approval
The study conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the Institutional Review Board of Camillians Saint Mary's Hospital Luodong (No. SMHIRB-103004). The informed consents were waived since there was neither breach of privacy nor interference with clinical decisions.
Study population
This retrospective study was conducted with a study period from January 1, 2011, to December 31, 2013, in a regional teaching hospital in eastern Taiwan. Adult patients who were hospitalized during the study period were eligible for enrollment if they met the criteria: 1) Having a serum NT-pro BNP test undertaken within 24 hours after admission, and the serum NT-pro BNP level reached the age-related cut-points; 2) Receiving echocardiography examinations in the index hospitalization; and 3) Having HF listed within the first two priorities of final diagnoses at discharge (International Classification of Diseases (ICD)-9 code, 428, 428.0, 428.1, and 428.9). The age-related cut-points which had been proven to identify acute HF patients were defined as serum NT-pro BNP of: 1) > 1800 pg/ml in patients over 75-years; 2) > 900 pg/ml in patients aged 50-75 years; and 3) > 450 pg/ml in patients below 50-years [11]. Exclusion criteria included patients who were less than 18-years of age, who had severe chronic pulmonary diseases (i.e., forced expiratory volume in one second < 1 liter in pulmonary function), decompensated hepatic diseases with as cites, or renal failure requiring renal replacement therapy.
The enrolled patients were categorized into 4 groups by quartile of their initial serum NT-pro BNP levels. The four groups included NT-1 (NT-pro BNP < 2,825 pg/ml), NT-2 (NT-pro BNP 2,825-6,493 pg/ml), NT-3 (NT-pro BNP 6,494-15,317 pg/ml), and NT-4 (NT-pro BNP ≧ 15,318 pg/ml).
The baseline demographic data, comorbidity diseases, etiologies of HF, medications, and clinical variables were documented from patients' medical charts.
After data gathering, we compared the basic characteristics and clinical parameters among the four groups, and further clarified the influential factors and their direct and indirect effect on serum NT-pro BNP level. All the data were analyzed anonymously.
Statistical analysis
The statistical analyses were performed using the Scientific Package for Social Science (PASW Statistics for Windows, Version 22.0, Chicago: SPSS Inc) and Analysis of Moment Structures (AMOS for Windows, Version 22.0, Chicago: SPSS Inc). The categorical variables were shown as numbers (percentages) and analyzed using the Chi-square test. The continuous variables were expressed as mean ± standard deviation (SD) and compared using the analysis of variance (ANOVA). Upon a significant comparison result in ANOVA, the post hoc tests with Scheffé testing and Games-Howell testing were further applied in homogenous and non-homogenous data, respectively, to compare the difference between any two groups. Finally, we put the variables with a significant difference in ANOVA into the regression paths model to investigate the influence of these factors utilizing regression coefficients and p-value. If the regression and correlation paths in both factors are not significant, we will delete the path. Subsequently, all factors with a significant difference in ANOVA would be put into the mediation path model.
By using mediation analysis, we explore how the factors affect serum NT-pro BPN level, and explicate that how independent variable affects a dependent variable through one or more potential intervening variables, or mediators, base on the estimation of the direct effect of exposure on the outcome and indirect effect acting through mediator [12]. The steps of mediation path model include 1) One of all factors taken as independent variable and other factors as mediators; 2) NT-pro BNP set as dependent variable; 3) Mediation analysis; 4) If the independent variable to mediators path are not significant correlation, the mediated path will be deleted; 5) The sum of all mediation paths model and testing model fit index. In all statistical analyses, a two-sided p ≦ 0.05 was considered statistically significant.
The model fit index statistic tests the consistency between the predicted and observed data matrix by the equation. "Normal Chi-Square Fit Index" (CMIN/DF) that chi-square values smaller than 2 or 3 are acceptable. "Goodness-of-Fit Index" (GFI) and "Adjusted Goodness-of-Fit Index" (AGFI) demonstrate that measures equal to or larger than 0.90 signify a 'good' fit. "Normed Fit Index or Bentler Bonett Index" (NFI) reveals 0.90 signifies an optimal fit. "Comparative Fit Index" (CFI) needs to be a minimum of 0.90 to be usable for a model fit. "Root Mean Square Error of Approximation" (RMSEA) and "Standardized root mean square residua" (SRMR) need smaller the 0.05 displays a preferable status and the more optimal fit results [13].
Results
During the study period, 1276 patients were screened. After excluding 990 due to lack of final diagnosis of HF within the first two priorities at discharge, less than 18 years of age, with severe chronic pulmonary diseases, decompensated hepatic diseases with as cites, or renal failure requiring renal replacement therapy, along with 17 due to lack of echocardiography examinations, a total of 269 patients (mean age, 74.45 ± 13.59-years; female, 53.9%) were enrolled. The mean of serum NT-pro BNP level in all patients is 11,530.93 pg/ml (SD 12,062.03), and the median is 6494.00 pg/ml. According to the predefined groups, all patients were categorized into NT-1 (n = 67), NT-2 (n = 67), NT-3 (n = 68), and NT-4 (n = 67) groups. By using the G-Power developed by Erdfelder, et al. to estimate the power of multiple linear regression models with α of 0.05, an effect size of 0.46, and predictors of 6 in our study, the calculated power of our study reached 1.00.
Clinical characteristics and variables
In the comparisons of demographic and basic characteristics among the four groups, only age (p < 0.001) and body mass index (BMI) (p < 0.001) were of statistical significance (Table 1). As to the clinical variables at the initiation of the index hospitalization, body temperature (BT) (p = 0.011), heart rate (HR) (p = 0.039), left ventricular ejection fraction (LVEF) (p = 0.001), and NYHA Fc (p < 0.001), along with hemoglobin (p < 0.001), potassium (p = 0.011), and estimated glomerular filtration rate (eGFR) (p < 0.001) in laboratory tests were of significant differences among the four groups (Table 2).
Regression path model on factors affecting serum NT-pro BNP level
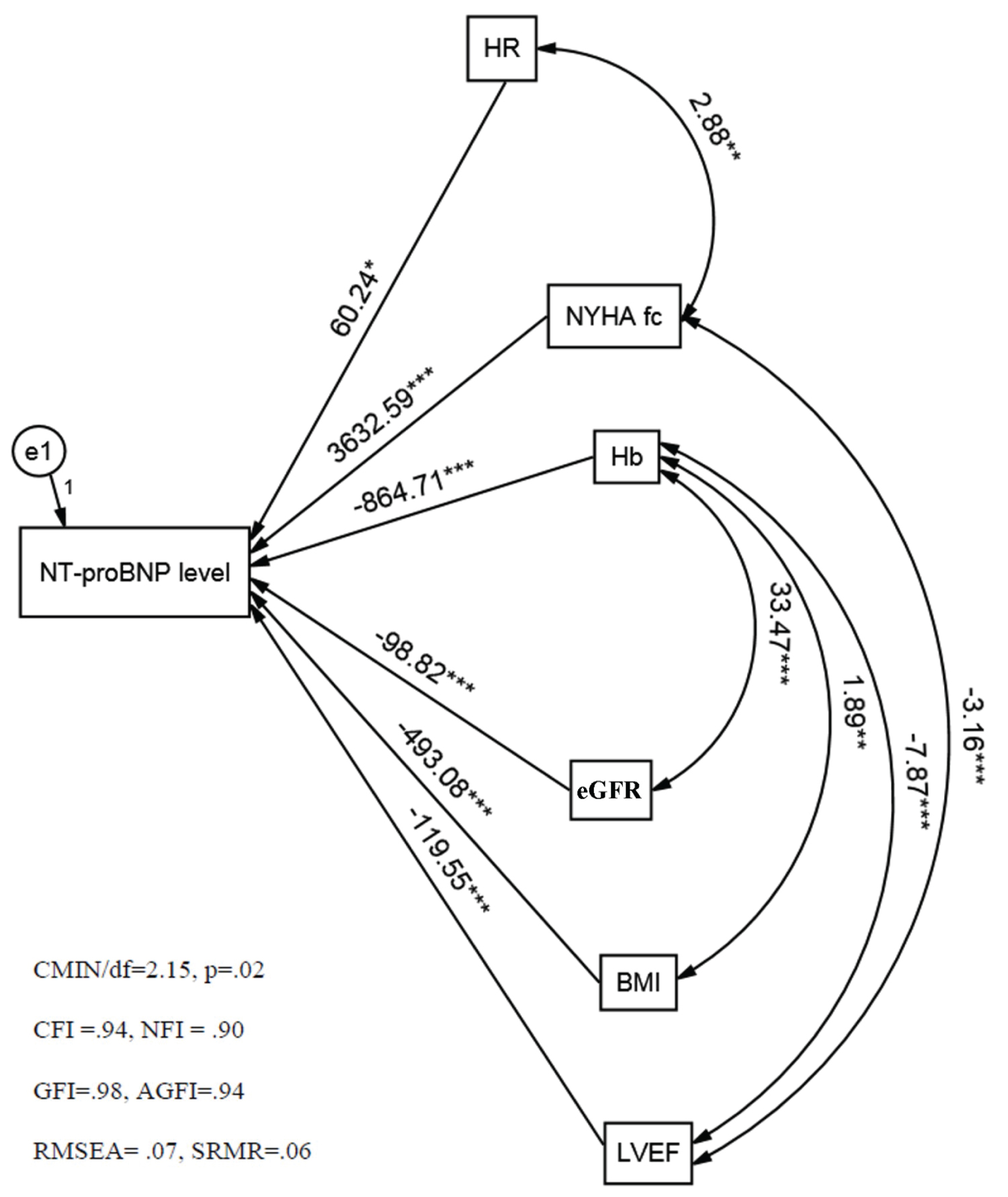
After putting the nine factors which were significantly associated with NT-pro BNP level into the regression path model, six factors, including HR, LVEF, NYHA Fc, BMI, hemoglobin, and eGFR persistently exhibited the influences on serum NT-pro BNP level after adjustment (Figure1).
Mediation path model on factors affecting serum NT pro BNP level
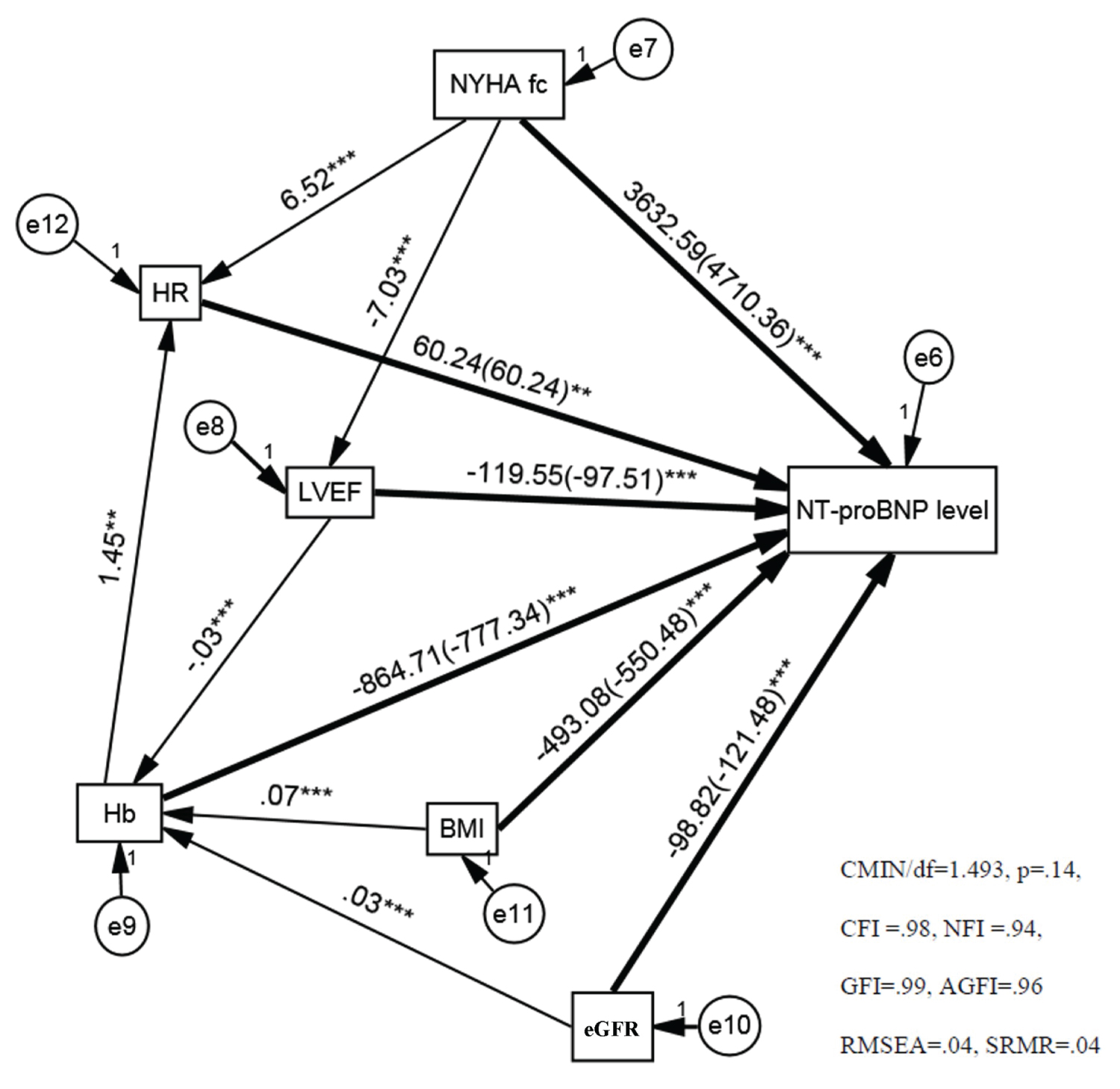
By using the mediation path model, we further evaluated the total, direct, and indirect mediation effects of the six factors. Besides affecting serum NT-pro BNP themselves, hemoglobin, LVEF, and HR also served as mediators leading to indirect effects on serum NT-pro BNP level. The quality of the model fit in this mediation model was also good (Table 3 and Figure 2).
Discussion
To the best of our knowledge, the current study is the first one to evaluate both the direct and indirect effects of influential factors on serum NT-pro BPN level under a situation with concurrently-existed factors in HF patients. We found that BMI, LVEF, NYHF Fc, hemoglobin, HR, and eGFR could influence serum NT-pro BNP level, and further clarified that hemoglobin, HR and LVEF could not only directly affect serum NT-pro BNP level but also indirectly influence other factor as mediators that lead to partial mediation, to affecting serum NT-pro BNP level in patients with HF.
Anemia, defined hemoglobin < 13 mg/dl in men and hemoglobin < 12 mg/dl in women, occurs commonly in HF patients with a prevalence rate of 9% to 25% [14]. The severity of anemia may also affect disease progression and mortality [15]. As to the correlation between serum NT-pro BNP level and hemoglobin, Desai, et al. [4] demonstrated an inverse correlation between hemoglobin and blood NT-pro BNP. Besides, when hemoglobin decreases by 1 mg/dl, serum NT-pro BNP level would increase by 9%. Inconsistent with the findings of Desai, et al. [4], our study disclosed that hemoglobin was negatively correlated with serum NT-pro BNP level, and when hemoglobin decreased by 1 mg/dl, serum NT-pro BNP level increased by 864.71 pg/ml.
Furthermore, the patients with HF often suffer from malnutrition (cachexia) because energy alienation and the malnutrition condition worsens the prognosis, which is called the obesity paradox [8]. BMI is commonly used to determine body mass. As regards the relationship between BMI and NT-pro BNP, Bayes-Genis, et al. [16] found that the serum NT-pro BNP level of patients with BMI < 25 kg/m2 is significantly higher than that of those with BMI > 25 kg/m2. When BMI decreases by 1 kg/m2, serum NT-pro BNP level increases by 4%. In our study, more than 50% of patients with lower NT-pro BNP levels (NT-1) were over-weighted, while most of the patients with higher NT-pro BNP levels (NT-4) were under-weighted (Table 1). Also, once BMI decreases by 1 kg/m2, serum NT-pro BNP level increases by 493.08 pg/ml. The tendency that a lower BMI indicates a higher serum NT-pro BNP level was similar to that of Bayes-Genis, et al. [16].
On the other hand, they mostly suffer from renal dysfunction, and renal function is also an influential factor in serum NT-pro BNP level. Inadequate renal function not only results in decreased renal clearance of NT- pro-BNP and subsequent increment of serum NT- pro BNP level, but also causes body fluid retention, which further increases the pressure of the left ventricle [10]. Vickery, et al. [17] expressed serum NT-pro BNP level increased by 20.6% per 10-mL/min/1.73 m2 (0.17-mL/s) reduction in eGFR. Our results consisted of that of Vickery, et al. [17] and showed that eGFR was an inverse relationship with serum NT- pro BNP level, increased by 98.82 pg/ml pre 1 ml/min/1.73 m2 reduction in eGFR.
Practically, HF can be classified into HF with reduced ejection fraction (HFrEF) and HF with preserved ejection fraction (HFpEF) according to the LVEF. Januzzi, et al. [11] demonstrated that the serum NT-pro BNP level of patients in the HFpEF group (3,070 pg/ml) is less than that of the HFrEF group (6,536 pg/ml) (p < 0.001). Besides, Kallistratos, et al. [5] found serum NT-pro BNP level is inversely correlated with LVEF (r = -0.59, p < 0.001). In our study, only NT-4 (LVEF, 43.01%) could be classified as HFrEF according to their mean LVEF, and the mean LVEF of patients in NT-2 (54.10%) was significantly higher than that in NT-4 (43.01%), whereas the mean LVEF among NT-1~NT-3 were of no significant difference. Although some of our findings were consistent with that from Januzzi, et al. [11] and Kallistratos, et al. [5], we further suggested that the serum NT-pro BNP level cut-off point of most patients was 15,318 pg/ml in the HFpEF and HFrEF groups. The serum NT-pro BNP level increased by 119.55 pg/ml per 1% reduction in LVEF.
Besides classification by LVEF, HF can also be classified according to the expression of clinical symptoms, of which NYHA Fc is used most frequently [18]. Song, et al. [9] demonstrated the serum NT-pro BNP of patients of NYHF Fc-II, -III, and -IV were 992.8 pg/ml, 2,937.9 pg/ml, 12,127.8 pg/ml, respectively. Moreover, NYHF is positively correlated with the serum NT-pro BNP level. Similarly, we found that the serum NT-pro BNP level of most patients of NYHF Fc-II was < 2,825 pg/ml, and that of most patients of NYHF Fc-III was > 2,825 pg/ml. The serum NT-pro BNP of most patients of NYHF Fc-IV was > 15,318 pg/ml. NYHF Fc was positively correlated with NT-pro BNP. For each level increased, the serum NT-pro BNP level increased by 4,032.32 pg/ml. Besides, we found that the serum NT-pro BNP level was positively associated with HR, which was consisted of the findings of Cao, et al. [19] and James, et al. [20].
Clinically, the patients with HF concurrently have multiple factors that may be mutually mediated and could affect serum NT-pro BNP level during hospitalization. The serum NT-pro BNP level is influenced by the sum of both direct effects from certain factors and indirect effects, which may be induced by mediators. In the current study, we clarified the mediating role of affecting serum NT-pro BNP levels of some factors, namely, hemoglobin, HR, and LVEF. Hemoglobin augmented the substantial effect on serum NT-pro BNP level of eGFR and BMI but suppressed the influence of LVEF. Besides, HR suppressed the substantial effect of hemoglobin and NYHA Fc, while LVEF suppressed the substantial effect of NYHA Fc.
Limitations
There were several limitations. First, because of the retrospective manner, the data obtained in our study were limited by the completeness and accuracy of medical records, which is the major limitation of the current study. Second, the investigation was mainly limited to the influence on serum NT-pro BNP level, without exploring the mutual relationship between serum NT-pro BNP level and clinical prognosis.
Further prospective researches to investigate the factors affecting the serum NT-pro BNP level in HF patients and explore the relationship between serum NT-pro BNP level and clinical prognosis of acute HF is encouraged. Besides, based on the findings of the current study, investigators could further use "multi-factors adjusted serum NT-pro BNP level" to develop a scoring index. Probably this index could serve as a better tool for screening and prognosis-predicting in patients with HF.
Conclusion
The current study identified several factors that could, directly and indirectly, affect the serum NT-pro BNP level. Based on these findings, an index using "multi-factors adjusted serum NT-pro BNP level" may be further developed as a better tool for screening and prognosis-predicting in patients with HF.
Acknowledgment
The authors thank Dr. Woung-Ru Tang and Hsueh-Erh Liu for their constructive suggestions in this study, and the team of Camillian Saint Mary's Hospital Luodong for proving the research environment and data management.
Funding
None declared.
Declaration of Conflict of Interest
None.
References
- McMurray JJ, Stewart S (2000) Epidemiology, aetiology, and prognosis of heart failure. Heart 83: 596-602.
- Welfare MoHa (2013) Causes of death in Taiwan, 2012. In: Welfare MoHa.
- Bayes-Genis A, Santalo-Bel M, Zapico-Muniz E, et al. (2004) N-terminal probrain natriuretic peptide (NT-proBNP) in the emergency diagnosis and in-hospital monitoring of patients with dyspnoea and ventricular dysfunction. Eur J Heart Fail 6: 301-308.
- Desai AS, Bibbins-Domingo K, Shlipak MG, et al. (2007) Association between anaemia and N-terminal pro-B-type natriuretic peptide (NT-proBNP): findings from the Heart and Soul Study. Eur J Heart Fail 9: 886-891.
- Kallistratos MS, Dritsas A, Laoutaris ID et al. (2008) Incremental value of N-terminal pro-brain natriuretic peptide over left ventricle ejection fraction and aerobic capacity for estimating prognosis in heart failure patients. J Heart Lung Transplant 27: 1251-1256.
- Krauser DG, Lloyd-Jones DM, Chae CU, et al. (2005) Effect of body mass index on natriuretic peptide levels in patients with acute congestive heart failure: A ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) substudy. Am Heart J 149: 744-750.
- Luchner A, Hengstenberg C, Lowel H, et al. (2005) Effect of compensated renal dysfunction on approved heart failure markers: Direct comparison of brain natriuretic peptide (BNP) and N-terminal pro-BNP. Hypertension 46: 118-123.
- Morse SA, Gulati R, Reisin E (2010) The obesity paradox and cardiovascular disease. Curr Hypertens Rep 12: 120-126.
- Song BG, Jeon ES, Kim YH, et al. (2005) Correlation between levels of N-terminal pro-B-type natriuretic peptide and degrees of heart failure. Korean J Intern Med 20: 26-32.
- Steiner J, Guglin M (2008) BNP or NTproBNP? A clinician's perspective. Int J Cardiol 129: 5-14.
- Januzzi JL, van Kimmenade R, Lainchbury J, et al. (2006) NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur Heart J 27: 330-337.
- Vander Weele TJ (2009) Introduction to Statistical Mediation Analysis by MACKINNON, D.P. Biometrics 65: 998-1000.
- Markus KA (2012) Principles and Practice of Structural Equation Modeling by Rex B. Kline. Structural Equation Modeling: A Multidisciplinary Journal 19: 509-512.
- Virani SA, Khosla A, Levin A (2008) Chronic kidney disease, heart failure and anemia. The Canadian Journal of Cardiology 24: 22-24.
- Tang YD, Katz SD (2006) Anemia in chronic heart failure: Prevalence, etiology, clinical correlates, and treatment options. Circulation 113: 2454-2461.
- Bayes-Genis A, Lloyd-Jones DM, van Kimmenade RR, et al. (2007) Effect of body mass index on diagnostic and prognostic usefulness of amino-terminal pro-brain natriuretic peptide in patients with acute dyspnea. Arch Intern Med 167: 400-407.
- Vickery S, Price CP, John RI, et al. (2005) B-type natriuretic peptide (BNP) and amino-terminal proBNP in patients with CKD: Relationship to renal function and left ventricular hypertrophy. Am J Kidney Dis 46: 610-620.
- Miller-Davis C, Marden S, Leidy NK (2006) The New York Heart Association Classes and functional status: what are we really measuring? Heart Lung 35: 217-224.
- Cao R, Bai Y, Xu R, et al. (2015) Association between resting heart rate and N-terminal pro-brain natriuretic peptide in a community-based population study in Beijing. Clin Interv Aging 10: 55-60.
- James SK, Lindahl B, Siegbahn A, et al. (2003) N-terminal pro-brain natriuretic peptide and other risk markers for the separate prediction of mortality and subsequent myocardial infarction in patients with unstable coronary artery disease: A Global Utilization of Strategies To Open occluded arteries (GUSTO)-IV substudy. Circulation 108: 275-281.
Corresponding Author
Chih-Chung Shiao, Division of Nephrology, Department of Internal Medicine, Camillian Saint Mary's Hospital Luodong, 160 Chong-Cheng South Road, Loudong 265, Yilan, Taiwan, Tel: +886-3-9544106#7951, Fax: +886-3-9544106#7954
Copyright
© 2021 Huang MS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.