Intrahepatic Pancreatic Pseudocysts: A Review of Recent Literature and Case Report
Abstract
Background: Intrahepatic pancreatic pseudocysts (IHPP) are a rare clinical entity which results from migration of amylase rich proteolytic pancreatic fluid along hepatogastric or hepatoduodenal ligaments into the hepatic parenchyma. There are no current management guidelines, and definitive management depends on varying features within each individual case. We report a rare case presenting with features of acute gastric outlet obstruction on a background of chronic pancreatitis. The rapid formation of this IHPP does not appear to have been previously reported in the literature.
Methods: We conducted a comprehensive literature search of both PubMed and the Cochrane library to identify cases of IHPPs in recent literature. This review article aims at comparing the clinical features and management of the reported case with those reported in world literature.
Results: Diagnosis and clinical management of IHPP is challenging. A combination of CT scanning and aspirate sampling are the most useful in establishing a diagnosis. Clinical management includes a conservative approach, percutaneous/endoscopic drainage, ERCP and pancreatic duct stenting. Open surgical management is reserved for cases where serious complications have occurred.
Conclusion: This is the first documented rapid formation of an IHPP in current literature. The most common approach for the management of IHPPs is through radiologically guided percutaneous drainage. Early diagnosis and successful definitive management are probably best determined by the size of the lesion and severity of the clinical presentation.
Keywords
Chronic pancreatitis, Intrahepatic, Pancreas, Pseudocyst
Abbreviations
IHPP: Intrahepatic Pancreatic Pseudocyst; ERCP: Endoscopic Retrograde Pancreatography; CT: Computerised Tomography; US: Ultrasound; EUS: Endoscopic Ultrasound
Introduction
Pancreatic pseudocysts are enclosed collections of pancreatic fluid, which are common sequelae following acute pancreatitis, usually occurring around four weeks after the initial pancreatic injury [1]. Most occur around the pancreas, with only around 22% of pseudocysts found as extra-pancreatic lesions in the mediastinum, pelvis, pleura, spleen and liver [2].
Intrahepatic pancreatic pseudocysts (IHPPs) are thought to be formed by two pathophysiological mechanisms [3,4]. The first involves the accumulation of pancreatic fluid in the pre-renal space where it digests through the parietal peritoneum into the lesser sac. From here it can track along the omentum or hepatogastric ligaments into the liver. The left lobe of the liver is the most common location, likely due to fluid tracking along the hepatogastric ligament [3]. The second mechanism involves tracking along the hepato-duodenal ligament into the porta hepatis which allows for the formation of intra-parenchymal collections [4].
Cases usually tend to present with non-specific abdominal pain or with symptoms similar to pancreatitis [3]. A combination of CT imaging and aspirate sampling provides a definitive diagnosis [5].
There are no current management guidelines for IHPP and each patient is taken on a case-by-case basis depending on factors such as the location and number of cysts, patient symptoms and co-morbidities, and whether a connection persists between the cyst and pancreas [6]. Interventions include aspiration and/or drainage, surgical and conservative approaches.
Case and Timeline
20/12/19 - A 71-year-old male presented with a 3-day history of upper abdominal pain and vomiting following multiple episodes of alcohol-induced pancreatitis, the most recent being 4 months previously. Blood tests showed raised inflammatory markers (CRP 265, white cell count 15.1 × 10*9/L), and he had hyperamylasaemia (315 U/L).
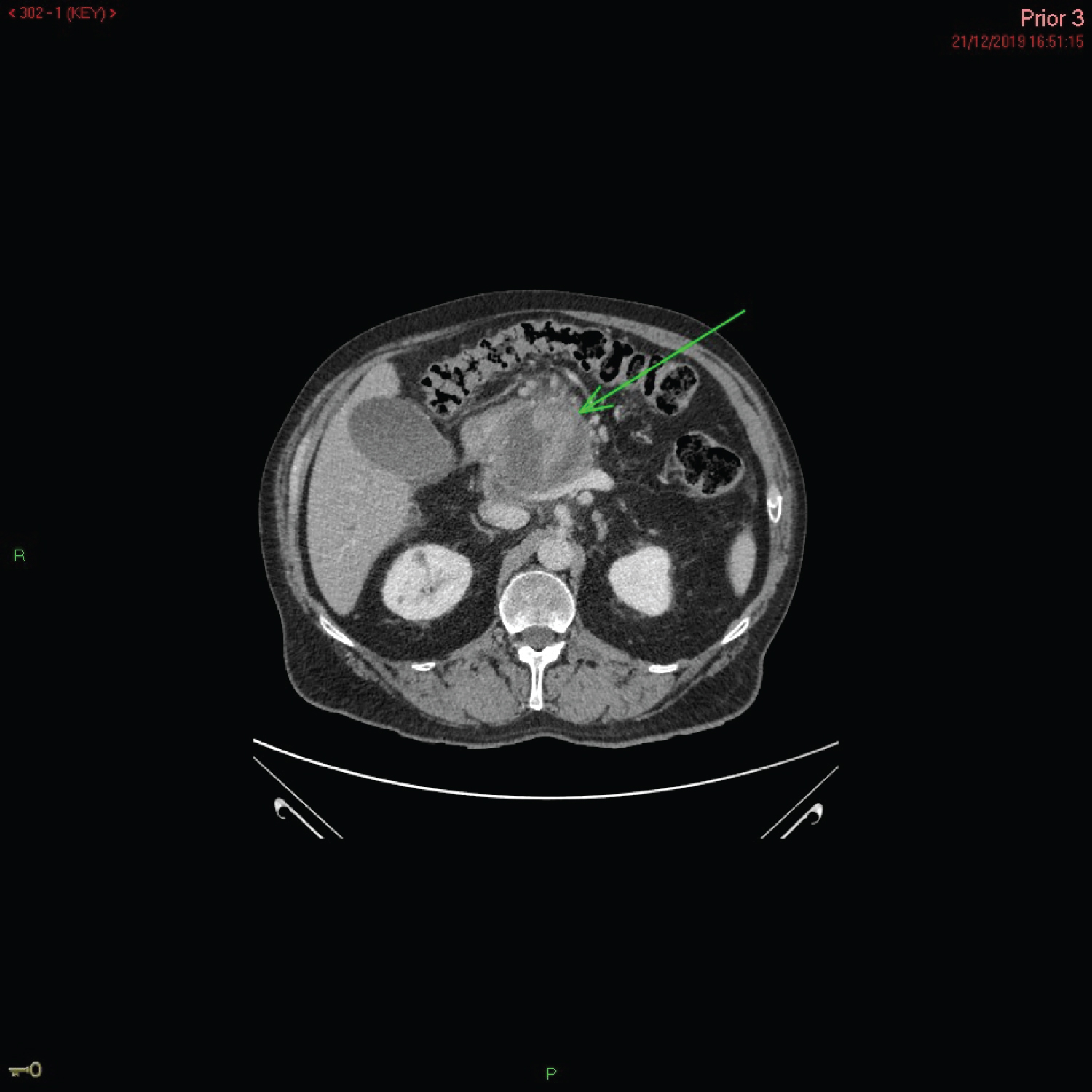
21/12/19 - A CT scan demonstrated evidence acute on chronic pancreatitis as well as enlargement of a known pseudocyst measuring 6.5 × 6.5 cm within the pancreas (Figure 1). The cyst had a high density, suggestive of haemorrhage. The liver was reported as normal in appearance.
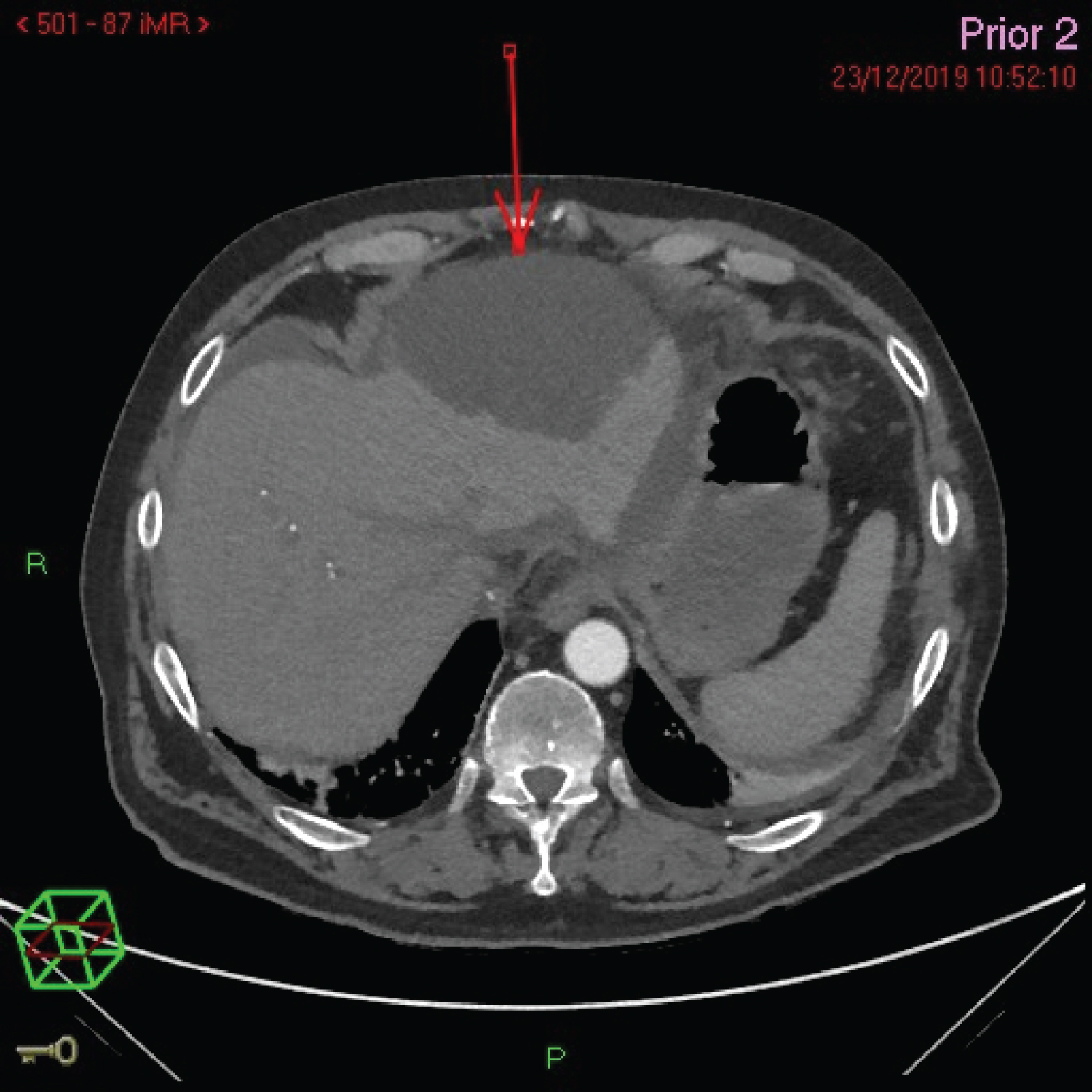
23/12/19 - A subsequent CT was performed 2 days later to exclude active haemorrhage or an underlying pseudoaneurysm. This demonstrated a new 12 × 10 cm subcapsular fluid collection in the left hepatic lobe (Figure 2).
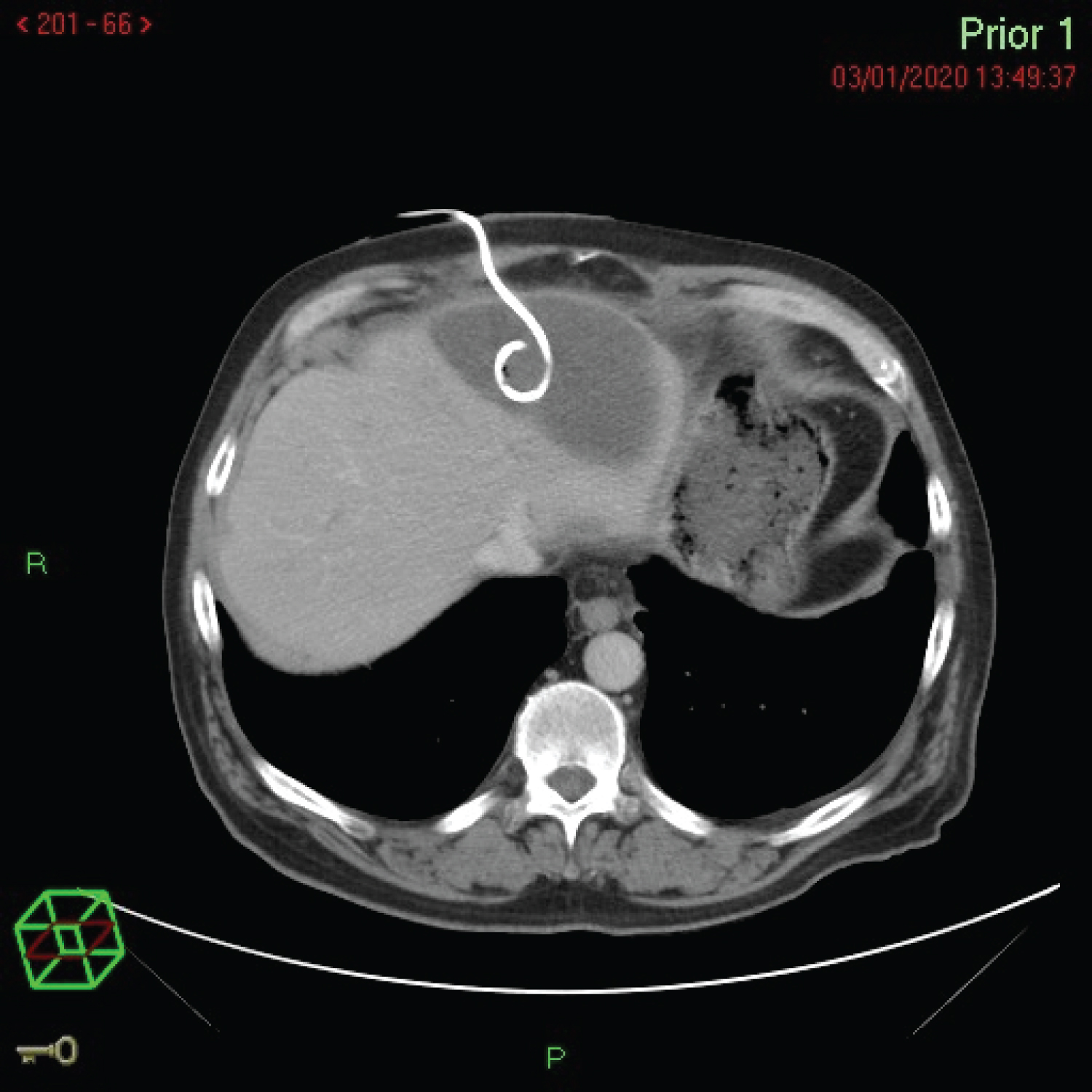
30/12/19 - This was managed by the insertion of ultrasound (US)-guided percutaneous drainage with pigtail catheter insertion on Figure 3. The fluid drained had an amylase of > 7500 U/L confirming the origin of the IHPP.
The rapid development and location of this novel cyst suggest it is likely the fluid breached through a barrier and spread to the left hepatic lobe via the first mechanism described above. A CT scan 2 weeks later reported a significant reduction in the size of the pseudocyst and the drain was subsequently removed.
Methods
A comprehensive review of the literature was recently reported by Demeusy, et al., 2016, [6] but here we further summarise knowledge by systematically reviewing recently reported cases.
PubMed and the Cochrane library were searched using the terms "pseudocyst" AND ("pancreas" OR "pancreatic") AND "intrahepatic" in the title or abstract, and studies published in English language were included. We reviewed the full texts and assessed for eligibility using two reviewers independently (HRE &TP), and we also reviewed references and citations for all publications. This search resulted in 70 results; we excluded papers published before 2016 there were a total of 10 publications comprising 11 cases.
Results
Including this current case, a total of 9 (75%) were male. In the cases identified only one was in a child (aged 10 years), who had a history of pancreatitis symptoms following blunt trauma to the abdomen. The remaining 11 cases had a mean age of 55 years with only 2 (18%) having no history of alcohol misuse. The exact location of the IHPP was not reported in three cases. Table 1 [7-13] provides a summary of the findings.
The case reported by Patidar, et al., 2018 was the only example to be managed fully conservatively, though it can be noted the cyst was relatively small compared with other studies.
Of those where the management was reported [11], 7 (64%) were managed with percutaneous drainage/aspiration and of these 5 were completed with US guidance. EUS-guided trans-gastric drainage accounted for 2 (18%) cases, however in the Kim, et al., 2017 study, postoperative perititonism lead to the suspicion of a rupture, which meant an emergency left hemi-hepatectomy was performed. In this case and that of Di and Carlos, 2016 who also had emergency surgery, no long-term complications were reported after 28 months and 6 years respectively.
Of the 4 cases that measured the length of time for complete resolution following US/CT-guided percutaneous insertion of a pigtail catheter, all reported complete resolution by 2 weeks [1,4,8,9].
Discussion
Patients with a history of alcohol-related pancreatitis appear more likely to develop IHPPs compared with gallstone related pancreatitis [14], and men are more likely to develop IHPPs (3:1) compared with women [7].
IHPPs can be frequently misdiagnosed or have their diagnosis delayed as there are more common differential diagnoses such as hydatid cysts, biliary dilatation, malignancy/metastasis or hepatic abscesses [5,13]. MRI may be better for identifying vascular complications such as pseudoaneurysms or venous thrombosis [10]. IHPPs can have atypical appearances on US due to haemorrhage or debris [13] and so CT is the imaging modality of choice [1].
Aspiration is useful to confirm diagnosis and rule out important differential diagnoses such as malignancy. Aspirates can be tested for amylase which allows for a definitive diagnosis [5] and a study of the cellularity can be used to rule out neoplasms [3].
Before the advancement of current radiological image-aided drainage, many patients underwent laparotomy [6], though in recent years this has shifted to percutaneous drainage which is less invasive and usually tolerated well with minimal complications. Recently, endoscopic retrograde pancreatography (ERCP) has allowed a further avenue of management options [6].
US-guided percutaneous drainage was the preferred management modality in recent studies we reviewed, with surgical intervention reserved for cases where complications are suspected. Percutaneous drainage pseudocysts have 3 distinct advantages over an endoscopic approach: allowing close monitoring of drainage; enabling manipulation of the catheter position; and, facilitating analysis of drained cystic contents [15].
Conservative management may still result in complete resolution in some cases, although complications often require further interventional management.
Generally, operative intervention for IHPPs is reserved for cases where there is suspected significant infection or rupture [5,6,12]. Of the new cases reported in this article, there were no reported deaths, but the previous case series showed 4 reported deaths [6]. The size of IHPP and initial WBC count correlated with the duration of therapy and the number of interventions [6].
Conclusion
IHPPs are rarely included as a differential in a patient complaining of abdominal pain, though they should be considered in patients who recently had an episode of acute pancreatitis. We report the rapid development of an IHPP 2 days following a CT which reported a liver that was normal in appearance. We believe this is the first case to report such a developing cyst within the current literature. CT is the imaging modality of choice to correctly identify the size and location of IHPPs and should be combined with fine-needle aspiration to confirm the diagnosis and rule out more sinister causes. Conservative management can be successful however management is usually via US or CT guided percutaneous drainage which is generally well-tolerated and seems to provide complete a resolution within 2 weeks. There are still no published guidelines for IHPPs, and this is likely due to their sparsity within the literature. However, longitudinal follow up studies are needed to determine optimal management and whether there are any associations with longer-term outcomes.
Competing Interests
The authors declare that they have no competing interest.
Authors' Contributions
• HRE - Conception and design, acquisition, analysis & interpretation of data, drafting of work and final approval.
• TP - Conception and design, acquisition, drafting of work and final approval.
• AM - Conception and design, drafting of work and final approval.
Informed Consent
Informed consent was obtained from the patient.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Chaturvedi A, Gaba S, Gupta M, et al. (2018) Intrahepatic pseudocyst following acute pancreatitis. Med J Dr. D.Y. Patil Vidyapeeth 11: 548-550.
- Hamm B, Franzen N (1993) Atypisch Lokalisierte Pankreaspseudozysten in Leber, Milz, Magenwand Und Mediastinum: Ct-Diagnostik, RoFo Fortschritte Auf Dem Gebiete Der Rontgenstrahlen Und Der Neuen Bildgeb. Verfahren 159: 522-527.
- Guesmi F, Zoghlami A, Saidi Y, et al. (2009) Pancreatic pseudocysts located in the liver: A systematic review of literature. Tunis Med 87: 801-804.
- Topno N, Ghosh S, Baruah A (2016) A rare case report of hepatic subcapsular pseudocyst of pancreas. J Clin Diagn Res 10: PD18-PD19.
- Kim HJ, Jun CH, Park CH, et al. (2017) Intrahepatic pancreatic pseudocyst complicated by pancreatitis: A case report. Korean J Gastroenterol 70: 202-207.
- Demeusy A, Hosseini M, Sill AM, et al. (2016) Intrahepatic pancreatic pseudocyst: A review of the world literature. World J Hepatol 8: 1576-1583.
- Di G, Carlos J (2016) Bilateral Intrahepatic Pancreatic Pseudocyst § ' tico intrahepa Seudoquiste pancreas. 4: 541-543.
- Gupta D, Pipaliya N, Pandav N, et al. (2016) Intrahepatic pancreatic pseudocyst: Case series. 17: 410-413.
- Edmonds PJ, Arroyo JP, Morales A, et al. (2017) Intrahepatic pancreatic pseudocyst: A rare complication of pancreatitis. J Gastrointest Liver Dis 26: 222.
- Sanjib PB, Das K, Acharya I, et al. (2017) A rare case of chronic calcific pancreatitis with intrahepatic and splenic pseudocysts. Imaging Med 9: 85-87.
- Patidar Y, Sureka B, Singh VP, et al. (2018) Spontaneous rupture of intrahepatic pseudocyst into the inferior vena cava. Gastroenterol Rep 6: 225-227.
- Angsubhakorn N, Laub L, Keenan JC (2019) ERCP-associated infected intrahepatic pancreatic pseudocyst. IDCases 15: e00507.
- Tomar S, Ghasi RG, Agarwal J (2019) Multiple intrahepatic pancreatic pseudocyst (MIHPPs): An overlooked and misdiagnosed entity. Gastroenterol Hepatol Bed bench12: 263-266.
- Cho JH, Kim TN, Kim SB (2015) Comparison of clinical course and outcome of acute pancreatitis according to the two main etiologies: Alcohol and gallstone. BMC Gastroenterol 15: 87.
- Zerem E (2014) Treatment of severe acute pancreatitis and its complications, World J Gastroenterol 20: 13879-13892.
Corresponding Author
Hamish Reed-Embleton, Department of Surgery, University Hospital Hairmyres, East Kilbride, G75 8RG, Scotland, UK, Tel: +44-1412011100.
Copyright
© 2021 Reed-Embleton H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.