Current and Future Treatments, Prevention, Diagnosis on Peptic Ulcer
Abstract
Peptic ulcer was one of the most common diseases that affect the sub mucosal layer in the stomach and duodenum. They are mainly of two types acute and chronic. Certain factors also affect peptic ulcers such as Helicobacter pylori infection, NSAID medications, stress, alcohol, smoking, diet, genetics, and hormones. There are some tests for the diagnosis of peptic ulcer such as endoscopy, CT scan, stool blood test, MRI etc. And drugs like antacids, H2 blockers, acid pump inhibitors, and antibiotics may be prescribed to treat peptic ulcers. For the risk of peptic ulcer and its prevention, people should avoid the consumption of tobacco products and alcohol, use of aspirin and NSAIDs.
Keywords
Peptic ulcer, Sign and symptoms, Diagnosis, Prevention, Treatment etc
Introduction
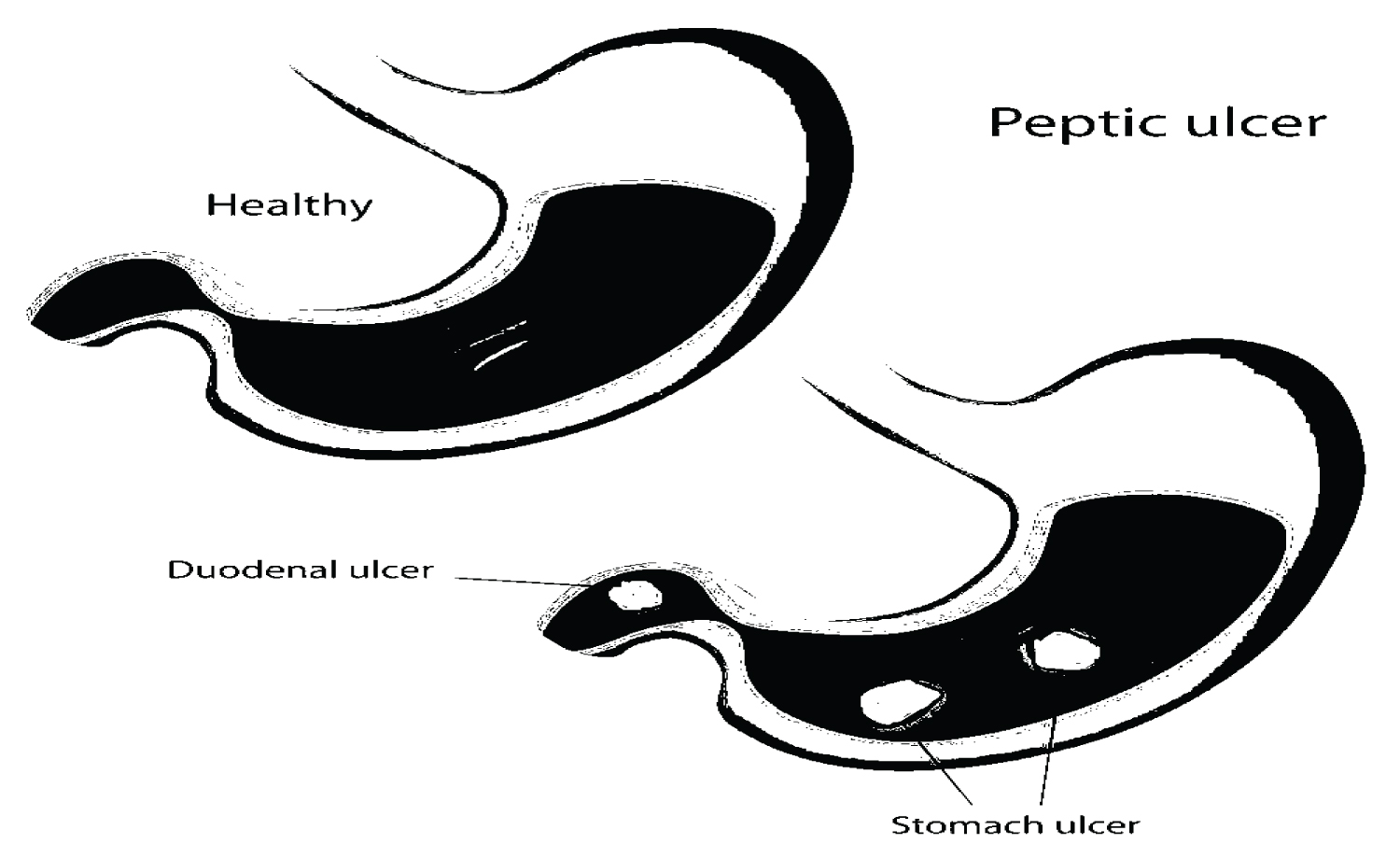
Peptic ulcers are the areas of degeneration and necrosis of gastrointestinal mucosa exposed to acid-peptic secretions. Though they can occur at any level of the alimentary tract that is exposed to hydrochloric acid and pepsin, they occur most commonly (98-99%) in either the duodenum or the stomach in the ratio of 4:1. Each of the two main types may be acute or chronic. Peptic ulcer was one of the most common diseases which affects the sub-mucosal layer in the stomach and the duodenum; it was mainly associated with H. Pylori infection and excessive use of NSAID (non-steroidal anti-inflammatory drugs) [1]. Nowadays and in the last 20-30 years, the incidence of the disease has shown a sharp decrease, and this phenomenon has been associated with the improvement of drug therapy and the increase of hospital facilities [2]. The path physiology of peptic ulcers in addition to the risk factors and epidemiology [3-5]. We will discuss the diagnosing procedure hand to hand with the management plan for peptic ulcers and its complication. Most cases of peptic ulcer disease are associated with Helicobacter pylori infection or the use of nonsteroidal anti-inflammatory drugs (NSAIDs), or both. Pylori, and discuss the latest evidence in the management of complications related to peptic ulcer disease, including endoscopic intervention for peptic ulcer-related bleeding [6] (Figure 1).
Acute Peptic (Stress) Ulcers
Acute peptic ulcers or stress ulcers are multiple, small mucosal erosions, seen most commonly in the stomach but occasionally involving the duodenum.
Etiology
These ulcers occur following severe stress. The causes are as follows:
a) Psychological stress
b) Physiological stress as in the following:
• Shock
• Severe trauma
• Septicaemia
• Extensive burns (Curling’s ulcers in the posterior aspect of the first part of the duodenum).
• Intracranial lesions (Cushing’s ulcers developing from hyperacidity following excessive vagal stimulation).
• Drug intake (e.g. aspirin, steroids, butazolidine and indomethacin).
• Local irritants (e.g. alcohol, smoking, coffee etc).
Pathogenesis
It is not clear how the mucosal erosions occur in stress ulcers because actual hyper secretion of gastric acid is demonstrable in only Cushing’s ulcers occurring from intracranial conditions such as due to brain trauma, intracranial surgery and brain tumours. In all other etiologic factors, gastric acid secretion is normal or below normal. In these conditions, the possible hypotheses for genesis of stress ulcers are as under:
1. Ischaemic hypoxic injury to the mucosal cells.
2. Depletion of the gastric mucus ‘barrier’ rendering the mucosa susceptible to attack by acid-peptic secretions.
Chronic Peptic Ulcers (Gastric and Duodenal Ulcers)
If not specified, chronic peptic ulcers would mean gastric and duodenal ulcers, the two major forms of ‘peptic ulcer disease’ of the upper GI tract in which the acid-pepsin secretions are implicated in their pathogenesis. Peptic ulcers are common in the present-day life of the industrialised and civilised world. Gastric and duodenal ulcers represent two distinct diseases as far as their etiology, pathogenesis and clinical features are concerned. However, morphological findings in both are similar and quite diagnostic.
Incidence
Peptic ulcers are more frequent in middle-aged adults. The peak incidence for duodenal ulcer is 5 th decade, while for gastric ulcer it is a decade later (6 th decade). Duodenal as well as gastric ulcers are more common in males than in females. Duodenal ulcer is almost four times more common than gastric ulcer; the overall incidence of gastro duodenal ulcers being approximately 10% of the male population.
Etiology
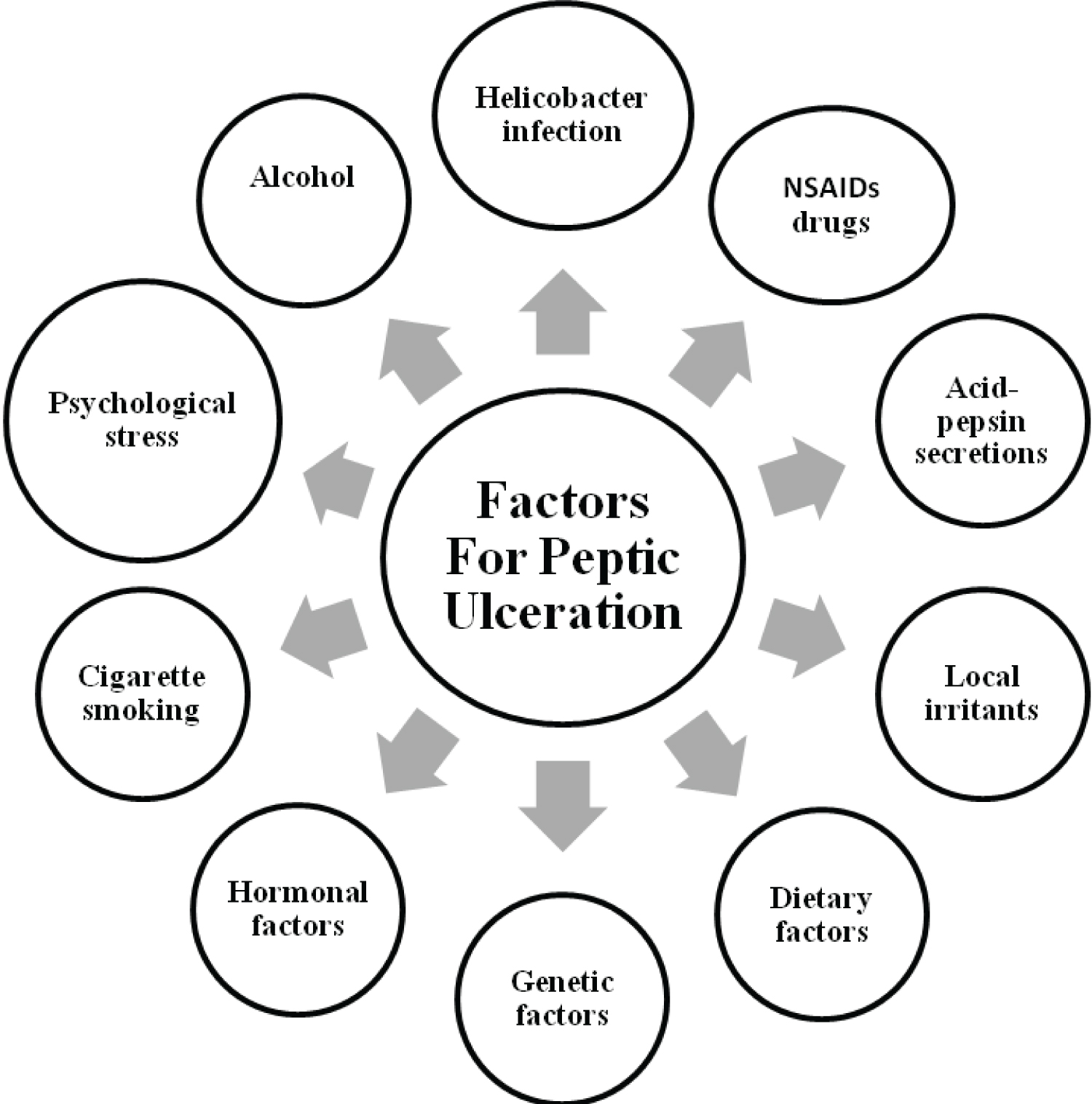
The immediate cause of peptic ulcer disease is disturbance in normal protective mucosal ‘barrier’ by acidpepsin, resulting in digestion of the mucosa. However, in contrast to duodenal ulcers, the patients of gastric ulcer have low-to-normal gastric acid secretions, though true achlorhydria in response to stimulants never occurs in benign gastric ulcer. Besides, 10-20% patients of gastric ulcer may have coexistent duodenal ulcer as well. Thus, the etiology of peptic ulcers possibly may not be explained on the basis of a single factor but is multifactorial. These factors are discussed below but the first two- H. Pylori gastritis and NSAIDs-induced injury are considered most important.
1. Helicobacter pylori gastritis: About 15-20% cases infected with pylori in the antrum develop duodenal ulcer in their life time while gastric colonisation by H. pylori never develops ulceration and remain asymptomatic. H. pylori can be identified in mucosal samples by histologic examination, culture and serology as discussed on page 548.
2. NSAIDs-induced mucosal injury: Non-steroidal anti-inflammatory drugs are most commonly used medications in the developed countries and are responsible for direct toxicity, endothelial damage and epithelial injury to both gastric as well as duodenal mucosa.
3. Acid-pepsin secretions: There is conclusive evidence that some level of acid-pepsin secretion is essential for the development of duodenal as well as gastric ulcer. Peptic ulcers never occur in association with pernicious anaemia in which there are no acid and pepsin-secreting parietal and chief cells respectively.
4. Gastritis: Some degree of gastritis is always present in the region of gastric ulcer, though it is not clear whether it is the cause or the effect of ulcer. Besides, the population distribution pattern of gastric ulcer is similar to that of chronic gastritis.
5. Other local irritants: Pyloric antrum and lesser curvature of the stomach are the sites most exposed for longer periods to local irritants and thus are the common sites for occurrence of gastric ulcers. Some of the local irritating substances implicated in the etiology of peptic ulcers are heavily spiced foods, alcohol, cigarette smoking, unbuffered aspirin.
6. Dietary factors: Nutritional deficiencies have been regarded as etiologic factors in peptic ulcers e.g. occurrence of gastric ulcer in poor socioeconomic strata, higher incidence of duodenal ulcer in parts of South India.
7. Psychological factors: Psychological stress, anxiety, fatigue and ulcer-type personality may exacerbate as well as predispose to peptic ulcer disease.
8. Genetic factors: People with blood group O appear to be more prone to develop peptic ulcers than those with other blood groups. Genetic influences appear to have greater role in duodenal ulcers as evidenced by their occurrence in families, monozygotic twins and association with HLA-B5 antigen.
9. Hormonal factors: Secretion of certain hormones by tumours is associated with peptic ulceration e.g. elaboration of gastrin by islet-cell tumour in Zollinger-Ellison syndrome, endocrine secretions in hyperplasia and adenomas of parathyroid glands, adrenal cortex and anterior pituitary.
10. Miscellaneous: Duodenal ulcers have been observed to occur in association with various other conditions such as alcoholic cirrhosis, chronic renal failure, hyperparathyroidism, chronic obstructive pulmonary disease, and chronic pancreatitis (Figure 2).
Pathogenesis
Although the role of various etiologic factors just described is well known in ulcerogenesis, two most important factors in peptic ulcer are as under: Exposure of mucosa to gastric acid and pepsin secretion. Strong etiologic association with H. pylori infection. There are distinct differences in the pathogenetic mechanisms involved in duodenal and gastric ulcers as under:
Diagnosis
Physical examination and thorough medical history, plus one or more of the following procedures: Endoscopic exam of the stomach (gastroscopy) or the upper bowel (esophago gastro duodenoscopy), including tissue biopsy, to detect H. pylori bacteria.
To locate the source of gastrointestinal bleeding, the doctor may order one or more of the following:
Stool blood test
Complete blood count
Prothrombin time blood test
Angiogram
Sigmoidoscopy or colonoscopy
Scintigraphic studies
CAT (CT) scan
Magnetic resonance imaging (MRI) scan
Prevention
To reduce your risk of developing a peptic ulcer:
Avoid tobacco products
Avoid alcohol
Use caution with aspirin and/or NSAIDs
Don’t ignore your ulcer symptoms
Protect yourself from infections by washing hands regularly and consuming foods that have been cooked thoroughly [7].
Treatment
Several types of drugs are typically incorporated into treatment:
Non-prescription antacids, taken intermittently to neutralize excess stomach acid and relieve abdominal pain.
H2 blockers (cimetidine, rantidine, famotidine), which reduce acid production in the digestive tract.
Antibiotics, if diagnostic tests reveal the presence of pylori .
Acid pump inhibitors (omeprazole).
Mucosal protective agents (sucralfate, misoprostol) [8].
Method & Material
We conducted this review paper by observing the different types of reviews and researches, as well as conducting and evaluating literature review papers.
Conclusion
Lastly, in our review, we were able to conclude that Peptic ulcer was one of the most common diseases that affects the sub mucosal layer in the stomach and duodenum. They are mainly of two types acute and chronic. Certain factors also affect peptic ulcers such as Helicobacter pylori infection, NSAID medications, stress, alcohol, smoking, diet, genetics, and hormones. There are some tests for the diagnosis of peptic ulcer such as endoscopy, CT scan, stool blood test, MRI etc. And drugs like antacids, H2 blockers, acid pump inhibitors, and antibiotics may be prescribed to treat peptic ulcers. For the risk of peptic ulcer and its prevention, people should avoid the consumption of tobacco products and alcohol, use of aspirin and NSAIDs.
Future Aspect
Drugs which abolish acid secretion and promise improved ulcer healing rates have produced dysplasia and tumours in experimental animals given large doses for long periods. Antioxidants help in scavenging the free radicals and controlling the oxidative stress responsible for the progression of peptic ulcer.
Acknowledgment
We grateful thanks to all the sincere and extremely helping friends for their support and help for the completion of work. Last but not the least, we thankful to all those who cooperated and helped me directly or indirectly to carry out this work.
Ethical Approval
Ethical approval was not required for this letter. All data used is publicly accessible.
Funding
There were no external sources of funding for this research.
Financial Support and Sponsorship
Nil.
Declaration of Competing Interest
All authors are, do not report any conflicts of interest in the writing of this letter.
References
- Lanas A, Chan FKL (2017) Peptic ulcer disease. Lancet 390: 613-624.
- Solanki N, Patel Y (2019) Drug utilization pattern and drug interaction study of antibiotics prescribed to orthopedic patients in private hospital. Archives of Pharmacy Practice 10: 114-117.
- Sardari M, Esmaeili R, Ravesh NN, Nasiri M (2019) The impact of pressure ulcer training program on nurses’ performance. Journal of Advanced Pharmacy and Education Research 9: 145-149.
- Althaiban M (2018) Antiulcer potential of olive leaves extract in gastric ulcer induced by indomethacin in male rats: Antioxidant and anti-inflammatory effects. Pharmacophore 9: 57-66.
- Mohammed AK, Al-Qadhi HI, Alkhalidi NM, Fawzi HA (2020) Effectiveness of infliximab and adalimumab in iraqi patients with ulcerative colitis - real world data. Journal of Advanced Pharmacy and Education Research 10: 46-51.
- Kavitt RT, Lipowska AM, Anyane-Yeboa A, Gralnek IM (2019) Diagnosis and treatment of peptic ulcer disease. Am J Med 132: 447-456.
- https://hunterdongastro.com/peptic-ulcers/
- https://www.healthychildren.org/English/health issues/conditions/abdominal/Pages/Peptic-Ulcers.aspx
Corresponding Author
Ashwin Singh Chouhan, Jai Narain Vyas University (New Campus), Jodhpur, Rajasthan, India.
Copyright
© 2023 Chouhan AS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.