Postpolypectomy Syndrome Presenting with Small Bowel Obstruction
Abstract
Introduction: Postpolypectomy syndrome (PPS) results from an electrical current that is applied during a polypectomy that extends past the superficial mucosa, into the muscularis propria and serosa, resulting in a transmural burn and subsequent inflammation. PPS has a good prognosis; however, there are exceptions in which complications can arise. This report presents a 71-year-old man who presented with a high grade small bowel obstruction 9 days after colonoscopy with polypectomy was performed. The patient failed conservative management and underwent surgical intervention with an ileocecectomy secondary to a small bowel obstruction at the ileocecal valve. Following surgical intervention, the patient's condition rapidly improved. Therefore, when the PPS occurs at the ileocecal valve, we suggest clinicians consider a diagnosis of small bowel obstruction as a consequence from the transmural and peritoneal inflammation. Patients with this diagnosis should be admitted to the hospital and closely observed to avoid adverse consequences.
Methods and procedures: A 71-year-old male presented to the emergency department with abdominal pain, worsening distention, nausea, and emesis. Denies any bowel movements for 9 days and reports 1 day history of obstipation. Of note, patient had a colonoscopy 9 days prior where a large sessile polyp was removed adjacent to the ileocecal valve. Patient was admitted for management of small bowel obstruction. He subsequently failed conservative management requiring surgical intervention. Intraoperatively, the terminal ileum was densely adhered to the ileocecal valve with friable, fibrinous and exudative tissue surrounding the valve. An ileocecectomy was performed with primary ileocolic anastomosis.
Results: Given the findings on colonoscopy, the patient was a high risk for developing PPS. First, he had a large polyp > 1 cm which increased his risk. Furthermore, the polyp was a sessile polyp. Lastly, the polyp was located in the cecum where the bowel thickness is less than other portions of the bowel. The most important aspect of this case was the location of the polyp on the upper lip of the ileocecal valve. The majority of PPS cases can be managed conservatively with intravenous fluids and antibiotics given that there is no bowel perforation. However, the localized peritoneal inflammation in this case resulted in a high grade small bowel obstruction requiring surgical intervention.
Conclusion: This case highlights the importance of obtaining accurate and specific records when making clinic decisions after a recent procedure. PPS has not been reported to cause small bowel obstruction. However, this case reports demonstrates that if PPS occurs at the ileocecal valve, the subsequent transmural and peritoneal inflammation can result in a high grade small bowel obstruction. Postpolypectomy syndrome (PPS) results from an electrical current that is applied during a polypectomy that extends past the superficial mucosa, into the muscularis propria and serosa, resulting in a transmural burn and subsequent inflammation.
PPS has a good prognosis; however, there are exceptions in which complications can arise. This report presents a 71-year-old man who presented with a high grade small bowel obstruction 9 days after colonoscopy with polypectomy was performed. The patient failed conservative management and underwent surgical intervention with an ileocecectomy secondary to a small bowel obstruction at the ileocecal valve. Following surgical intervention, the patient's condition rapidly improved. Therefore, when the PPS occurs at the ileocecal valve, we suggest clinicians consider a diagnosis of small bowel obstruction as a consequence from the transmural and peritoneal inflammation. Patients with this diagnosis should be admitted to the hospital and closely observed to avoid adverse consequences.
Keywords
Colonoscopy, Postpolypectomy syndrome (PPS), Lower abdominal pain
Introduction
Colonoscopy is a diagnostic-therapeutic procedure recommended every 10 years to anyone over the age of 45 as well as other indications, including but not limited to, lower GI bleeding, abnormal imaging, inflammatory bowel disease, and evaluation of the terminal ileum. The risk of serious complications following colonoscopy is low (0-2%), although over 85% of them occur in the setting of polypectomy [1]. Postpolypectomy syndrome is a rare complication following a colonoscopy where a polyp is removed with electrocautery. Patients present with symptoms including abdominal pain, fever, leukocytosis, and peritoneal inflammation in the absence of bowel perforation. PPS with no further complications can be managed with conservative treatment, typically with intravenous antibiotics and intravenous fluids.
Case Report
This is a 71-year-old male who was scheduled for a screening colonoscopy. He had no prior history of colon polyps or colon cancer. He was asymptomatic at this time. During his screening colonoscopy, he was noted to have a pedunculated polyp in the transverse colon and two sessile polyps in the cecum, one which was one the upper lip of the ileocecal valve. Both cecum polyps were removed with a snare and electrocoagulation. There were no apparent immediate complications and the patient went home in a stable condition. Pathology of the polyps demonstrated a tubular adenoma of the transverse colon polyp and two tubulovillous adenomas with high grade dysplasia in the cecum. Given these findings, a surveillance colonoscope in 6 months was recommended.
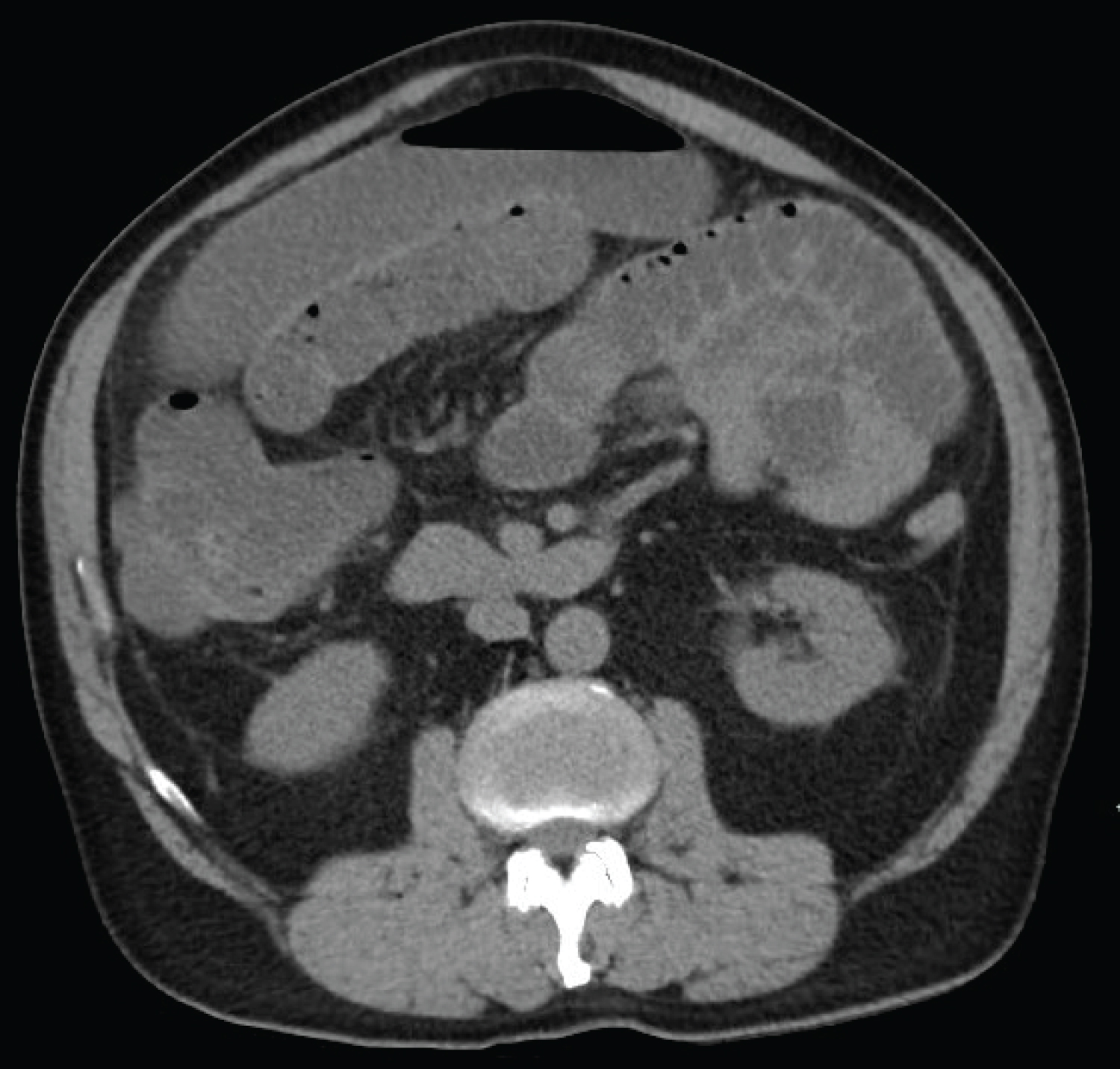
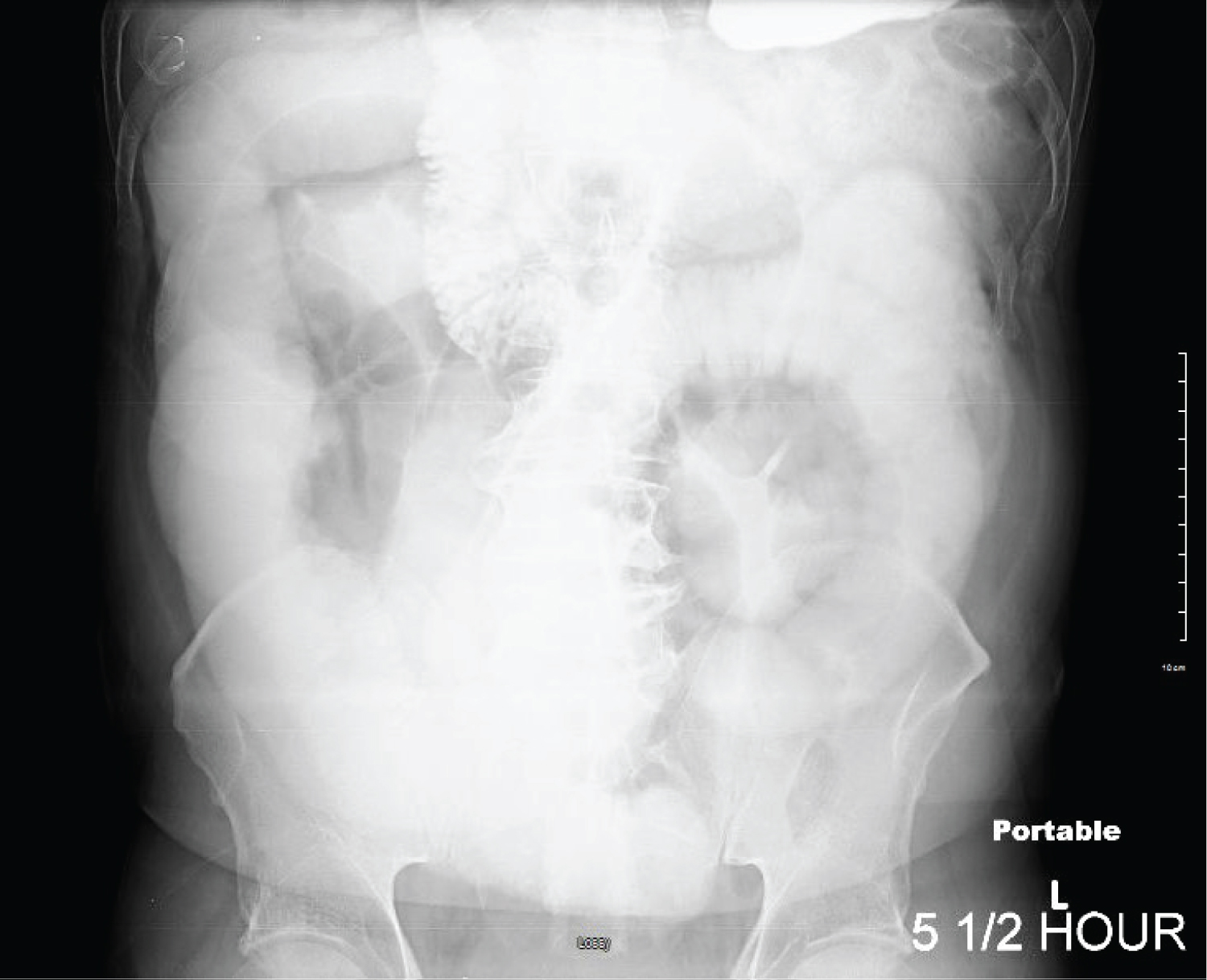
Nine days after his colonoscopy, the patient presented to the emergency room with a one day history of abdominal pain, worsening distention, nausea and emesis. He reports he has not had a bowel movement since his colonoscopy, but reports passing flatus until 1 day ago. His prior surgical history included a radical prostatectomy. His vitals signs were stable, afebrile, and CBC and BMP within normal limits with a normal lactic acid. On exam, his abdomen was soft but moderately distended with diffuse tenderness to deep palpation with no guarding or rebound tenderness. Given his history and clinically findings, the diagnosis of a small bowel obstruction was made. A CT scan of the abdomen and pelvis (Figure 1) was obtained demonstrating dilated loops of small bowel and a possible transition point near the ileocecal valve. The patient was admitted and conservative management was initially pursued with nasogastric tube decompression, strict NPO, and intravenous fluids. The following morning, a small bowel follow through was obtained which demonstrated a high grade small bowel obstruction with no contrast in the colon after 5 hours (Figure 2). Given these findings, he was taken to the operating room for a diagnostic laparoscopy.
In the operating room, a diagnostic laparoscopy was performed noting diffusely distended and edematous small bowel with decompressed colon. The small bowel was run from the ligament of Treitz to the ileocecal valve where fibrinous and exudative tissue surrounding the ileocecal valve was encountered. The terminal ileum was densely adhered to the ileocecal valve and cecum requiring conversion to an open exploratory laparotomy. Upon dissecting the terminal ileum and ileocecal valve, the ileocecal valve was inflamed and friable with exudative tissue surrounding the ileocecal valve. There was no gross perforation. Given the state of the bowel, we proceeded with an ileocecectomy with primary ileocolic side to side functional end to end anastomosis. The patient was extubated and sent to the floors for postoperative management. Pathology from our specimen demonstrated an ulcerated mucosal lesion in the cecum adjacent to the ileocecal valve with active serositis and inflammatory exudate consistent with abscess. Over the next 5 days, the patient's diet was advanced and he was discharged in a stable condition.
Discussion
Postpolypectomy syndrome (PPS) is a rare complication of polypectomy electrocoagulation, which may present with hemorrhage and perforation. The pathophysiology behind the syndrome occurs when electrical current applied during a polypectomy extends past the mucosa into the muscularis propria and serosa. This results in a transmural burn and peritoneal inflammation, without colonic perforation. Most patients develop symptoms within 12 hours of the procedure but may occur up to 7 days later. PPS has not been reported to cause small bowel obstruction, although this case report demonstrates that if PPS occurs at the ileocecal valve, the subsequent transmural and peritoneal inflammation can result in a high-grade small bowel obstruction.
In previous reports, the incidence varied between 0-2% of colonoscopies with polypectomies resulting in PPS, and even fewer, if any, resulting in a small bowel obstruction. In a large multicenter study including 47,083 patients, PPS occurred in 34 patients (0.07 percent) [2].
There were a few exceptional findings in our case that should be noted. Firstly, the patient's signs of obstruction arose 9 days post-polypectomy, outside the normal 12 hour-7 day window. This patient denied any bowel movements for 9 days and reported a 1 day history of obstipation prior to this admission. Secondly, our report is of a small bowel obstruction, which has rarely been reported in previous case reports. This obstruction occurred secondary to peritoneal inflammation at the location of the polypectomy at the upper lip of the ileocecal valve.
The risk factors for PPS and subsequent small bowel obstruction in this case are the following: (I) This patient had a large polyp > 1 cm; (II) The polyp was a sessile polyp; (III) the polyp was located in the cecum where the bowel thickness is less than other portions of the bowel.
The most important aspect of this case was the location of the polyp on the upper lip of the ileocecal valve. According to a multicenter case-control study; hypertension, large lesion size, and non-polypoid configuration of the lesion are independently associated with PPS [3]. Patients with larger (> 2 cm) sessile polyps, especially in the right side of the colon with the thinness of the colon wall, have a significantly higher tendency of developing PPS after resection [4]. Given the findings on colonoscopy, such patients should be classified as "high-risk patients".
Techniques that may reduce the risk of bowel injury during polypectomy include performing a hot snare polypectomy technique, focusing on removing 1-2 mm of normal tissue surrounding the polyp as well as sub mucosal fluid injections for larger polyp removal, applied to decrease the risk of transmural burn through increasing the thickness of the sub mucosal layer [5].
The majority of PPS cases can be managed conservatively with intravenous fluids and antibiotics given that there is no bowel perforation. This patient subsequently failed conservative management requiring surgical intervention secondary to the peritoneal inflammation causing the small bowel obstruction. Intraoperatively, the terminal ileum was densely adhered to the ileocecal valve with friable, fibrinous and exudative tissue surrounding the valve. An ileocecectomy was performed with primary ileocolic anastomosis.
This is a rare and severe presentation of PPS with small bowel obstruction in the absence of a previous small intestine surgical history. The patient recovered due to prompt imaging and surgical intervention. This case highlights the importance of obtaining accurate and specific records when making clinic decisions after a recent procedure. Small bowel obstruction should be considered in a case of post-polypectomy abdominal pain, distention, and obstipation to avoid further complications such as perforation and peritonitis [6-8].
Author Disclosure
Casey Huckabee nor Drs. Casey Huckabee or Penelope Mash burn have any conflicts of interest or financial ties to disclose.
References
- Linda Lee MD (2021) Overview of colonoscopy in adults. Retrieved from Up-to-date.
- Kim HW (2014) What is different between postpolypectomy fever and postpolypectomy coagulation syndrome? Clin Endosc 47.
- Cha JM, Lim KS, Lee SH, et al. (2013) Clinical outcomes and risk factors of post-polypectomy coagulation syndrome: A multicenter, retrospective, case-control study. Endoscopy 45: 202-207.
- Hirasawa K, Sato C, Makazu M, et al. (2015) Coagulation syndrome: Delayed perforation after colorectal endoscopic treatments. World J Gastrointest Endosc 7: 1055-1061.
- Brooks D, Cash M (2021) Postpolypectomy coagulation syndrome. Retrieved from UpToDate.
- Bari Z, Fakheri H, Sardarian H (2015) Large bowel obstruction after colonoscopy; a case report. Middle East J Dig Dis 7: 253-256.
- Nivatvongs S (1986) Complications in colonoscopic polypectomy. An experience with 1,555 polypectomies. Dis Colon Rectum 29: 825-830.
- Zhuang Z-F, Ye Z-H, Zhong Z-S, et al. (2020) A case report of a post-polypectomy syndrome with severe sepsis and organ dysfunction. Ann Palliat Med 9: 488-492.
Corresponding Author
Casey Huckabee, American University of Antigua, 1801 Phoenix Pl, Niles, OH 44446, USA
Copyright
© 2022 Huckabee C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.