Racial Differences in Incidence and Mortality from Non-Variceal Upper Gastrointestinal Hemorrhage: A Nationwide Time Trend Analysis, 2008-2018
Introduction
Non-variceal upper gastrointestinal hemorrhage (NVUGIH) is a common reason for hospital admissions and carries 2-10% mortality. Mortality trends from NVUGIB over the last two decades were shown to be decreasing previously (1989-2009) [1]. However, there is limited literature addressing racial differences in longitudinal incidence and related mortality trends from NVUGIH [2]. We studied racial differences in incidence and mortality from NVUGIH in the USA between 2008-2018.
Keywords
Mortality, Gastrointestinal hemorrhage, Racial groups, Healthcare disparities, Minority health
Methods
This is a retrospective longitudinal trend analysis using national inpatient sample [3]. All adult patients (≥18 years old) with NVUGIH were identified using International Classification of Diseases (ICD), Ninth &Tenth revision codes for the corresponding years (Supplement 1). Multivariate linear or logistic regression was performed when appropriate. The yearly hospitalization rate per 100,000 was calculated by the US population estimate on July 1 of the corresponding year obtained from the US Census Bureau. Stata (v.14.2) was used to perform analyses considering two-sided P < 0.05 as statistically significant. The institutional review board approval was sought, but the study was deemed exempt due to the use of de-identified publicly available data.
Results
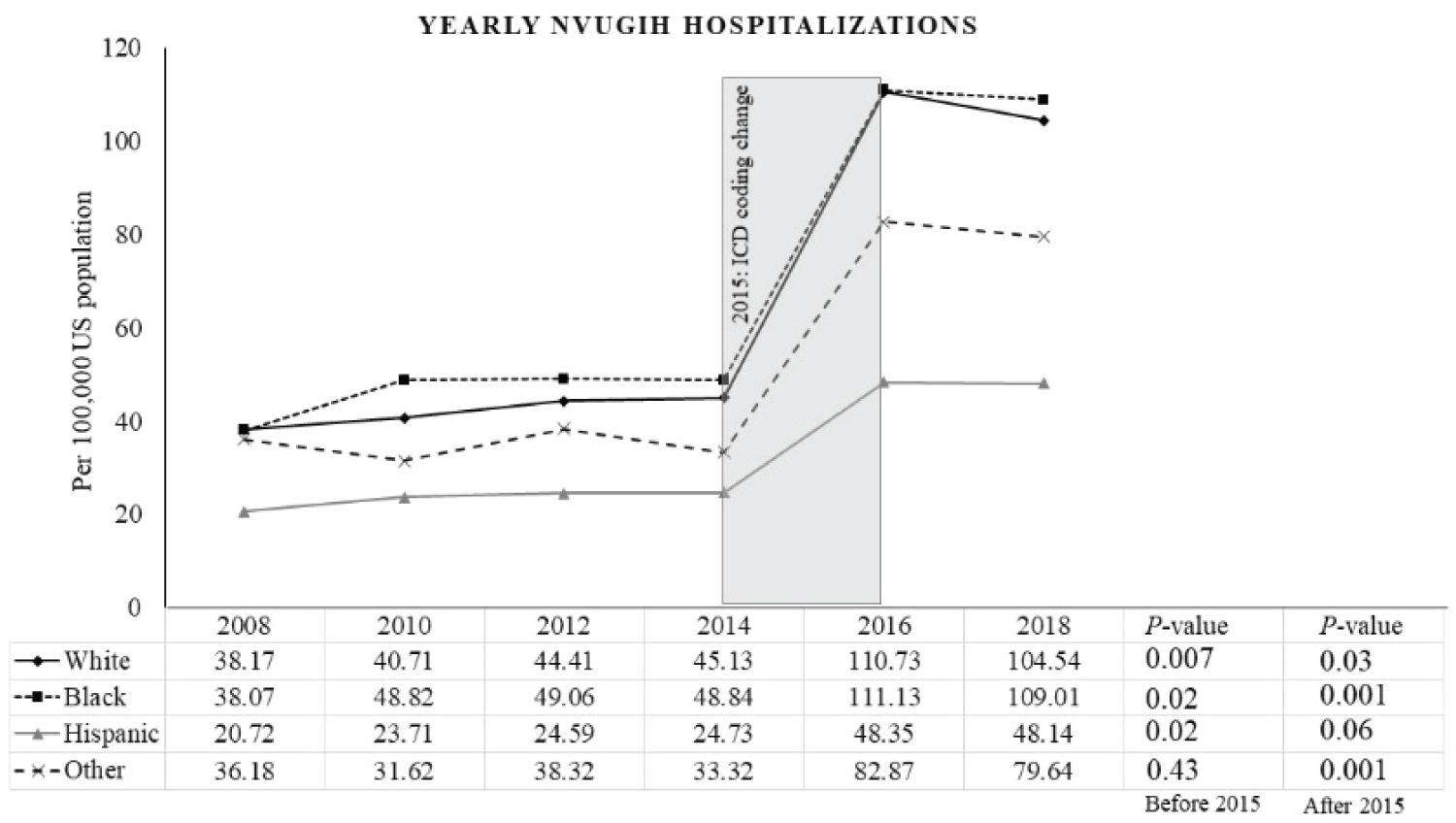
A total of 1.17 million adult hospitalizations with NVUGIH were included in the analysis. Baseline characteristics are summarized in (Table 1) (Supplement 1). Overall, 536,483 hospitalizations were captured before 2015, which increased to over 638,564 after the ICD coding change. Men had more hospitalization than women for entire cohort (52.59 - 55.61% vs 44.39 - 47.41% with P < 0.05). The average hospital length of stay was similar (ranging 4.17 - 4.28 days). Before 2015, the incidence (per 100,000 persons) increased from 30.89 in 2008 to 41.01 in 2014 (P < 0.001). Trends for each racial category from 2008 to 2014 were found to be 38.17 to 45.13 in Whites, 38.07 to 48.84 in Blacks, 20.72 to 24.73 in Hispanics, and 36.18 to 33.32 in others, respectively (Figure 1). Following 2015, the incidence decreased from 97.76 in 2016 to 93.07 in 2018 (P < 0.001). Significant racial trends from 2016 to 2018 were; 110.73 to 104.54 in Whites, 111.13 to 109.01 in Blacks, and 82.87 to 79.64 in others, while hispanics showed no difference (48.35 to 48.14, P = 0.06). Between the years 2008 through 2018, overall adjusted mortality from NVUGIH ranged from 1.82 - 2.46%. Mortality rates (in percentage) for each group were noted as 1.80 to 2.49 in Whites, 1.72 to 2.34 in Blacks, 1.47 to 2.76 in Hispanics, and 1.15 to 2.78 in others. No difference in mortality was seen among various races on longitudinal analysis before and after 2015 (interaction P-value 0.78 and 0.07, respectively). Mortality trends in each racial group were stable across the years before and after 2015 (P-value > 0.05).
Discussion
Blacks were found to have a higher incidence of NVUGIH despite constituting only 13% of the US population [4]. In contrast to other races, the incidence of NVUGIH did not decrease in Hispanics after 2015. This could occur due to differences in the prevalence of risk factors, including H. pylori infection, smoking, alcohol consumption, platelet inhibition and anticoagulant use, comorbidities, or disproportionate access to healthcare [2]. The specificity of ICD-10 coding resulted in better capturing and an apparent sharp increase in the incidence of NVUGIB after 2015. Before ICD coding change, trends were obtained uniformly by the ICD-9 coding system and represent true incidence variations. There was no mortality difference among different races for NVUGIH in this cohort. Furthermore, contrary to previous studies, mortality trends have plateaued, and the length of stay remains the same. Nationwide strategies are needed to decrease hospital stay and reduce mortality. Recent endoscopic advances, including over-the-scope clips for hemostasis, are very promising [5]. Limitation of this survey is the coding aberrations stemming from NIS relying on ICD codes. However, the current study reflects disproportionate racial trends in incidence for NVUGIH and calls for a constant need to develop strategies to lower the plateaued mortality trends.
Author Contributions
Study concept and design: UF, ED; Acquisition of data: UF; Analysis and interpretation of data: UF, MA, ED; Drafting of the manuscript: All authors; Critical revision of the manuscript for important intellectual content: ED, VT; Statistical analysis: UF, MA; Study supervision: ED, VT.
Financial Supports
None
Submission Declaration
This manuscript has not been previously submitted or being considered for publication in any other journal.
Conflict of Interest
None of the authors have any financial, industrial or commercial conflict of interest to disclose.
Data Access
All the authors have access to the data and participated in writing the manuscript.
References
- Abougergi M S, Travis A C, Saltzman J R (2015) The in-hospital mortality rate for upper GI hemorrhage has decreased over 2 decades in the United States: A nationwide analysis. Gastrointest Endosc 81: 882-888.e1.
- Wollenman C S, Chason R, Reisch J S, et al. (2014) Impact of ethnicity in upper gastrointestinal hemorrhage. J Clin Gastroenterol 48: 343-350.
- ICD-10-CM/PCS Resources. (2020) Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality, Rockville, MD.
- (2021) U S Census Bureau Quickfacts: United States.
- Jensen D M, Kovacs T, Ghassemi, et al. (2021) Randomized controlled trial of over-the-scope clip as initial treatment of severe nonvariceal upper gastrointestinal bleeding. Clin Gastroenterol Hepatol 19: 2315-2323.e2.
Corresponding Author
Umer Farooq, Department of Internal Medicine, Loyola Medicine/MacNeal Hospital, Berwyn, IL, USA.
Copyright
© 2022 Farrukh A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.