Unsuspected Radiological Diagnosis in a Child with Recurring Abdominal Pain
Case
A 5-year-old boy with a 4-month history of recurrent epigastric pain lasting several hours that disappears when vomiting undigested food. It appears sporadically, at any time of the day, interferes with night-time sleep and, is not clearly related to specific foods or meals.
The clinical picture persists despite symptomatic analgesic treatment and does not respond to a partial diet low in fermentable products.
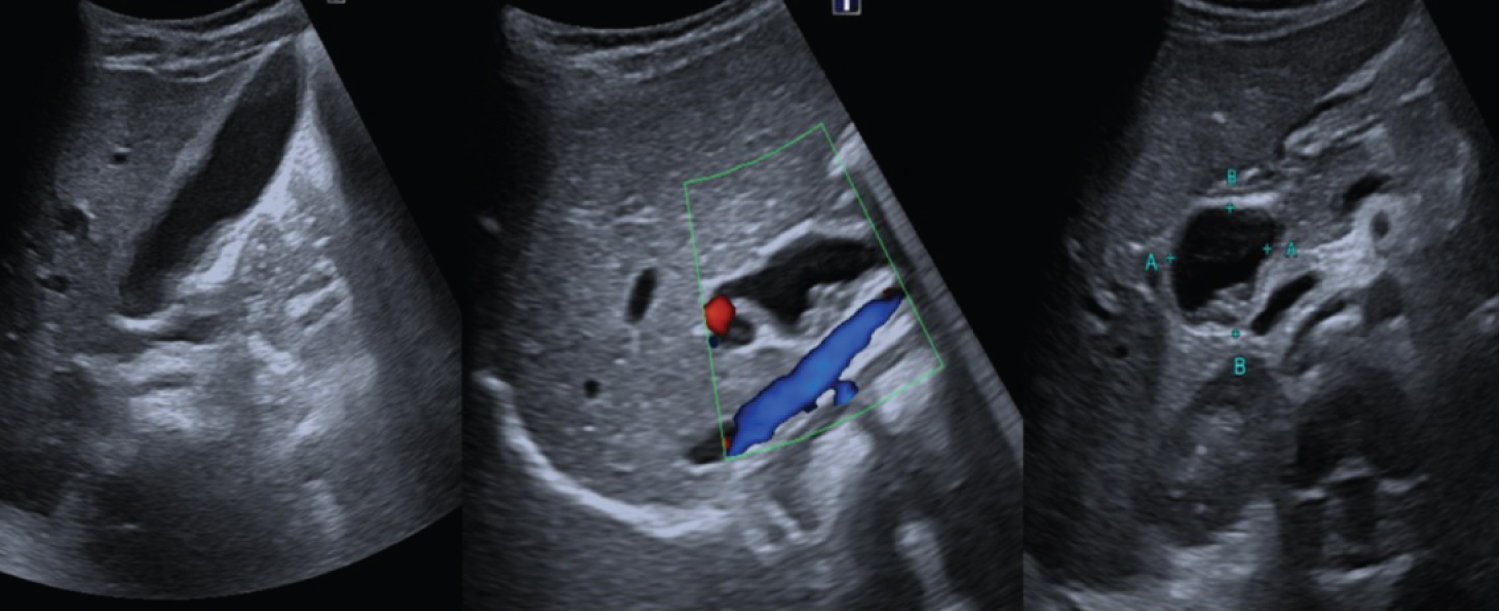
An abdominal ultrasound is requested, which shows cystic dilation of the extrahepatic bile duct, with multiple intracystic stones that associate a distended gallbladder with lithiasis and a diffusely thickened wall that reflects chronic inflammatory changes (Figure 1).
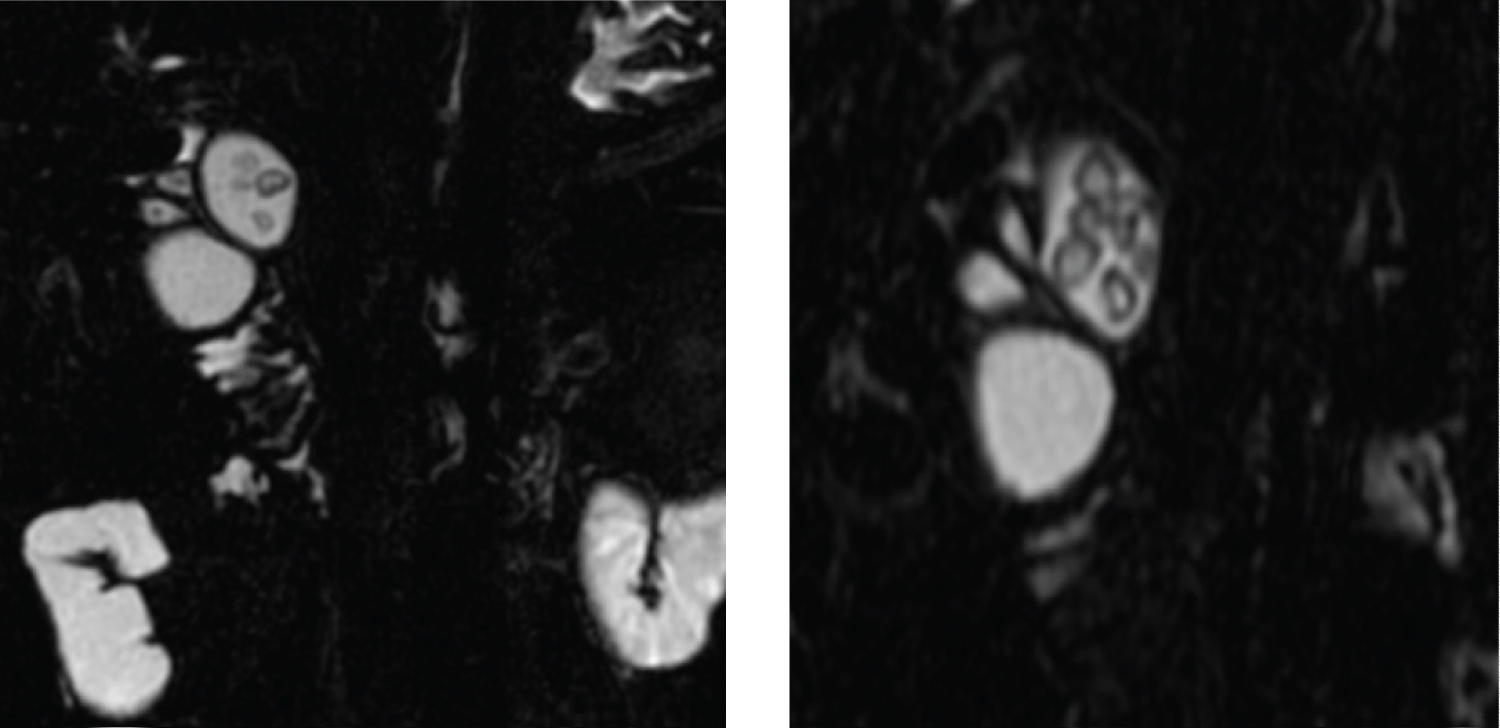
The study is completed with MR Cholangiopancreatography (MRCP) that confirms the diagnosis of Ic type common bile duct cyst with fusiform dilation of the common bile duct and liver and secondarily of the intrahepatic bile duct. As a significant finding in our case, it is worth highlighting the presence of multiple lithiases in the cyst as well as in the cystic duct, infundibulum and gallbladder (Figure 2).
Discussion
Choledochal cysts are rare congenital anomalies characterized by dilatation of the biliary tree.
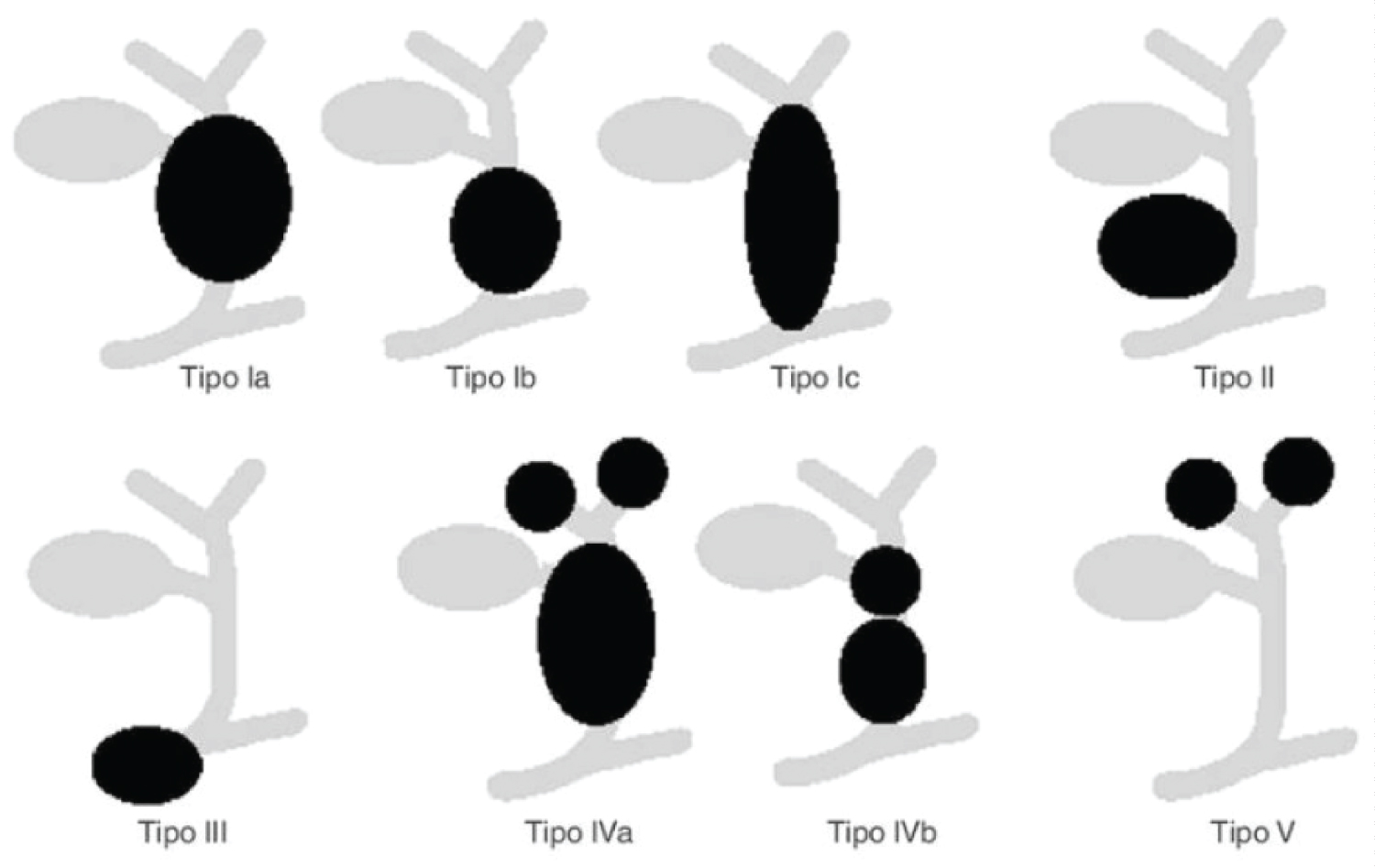
The Todani Classification establishes five types, according to the anatomical distribution of dilation (Figure 3) [1].
• Type I: Dilatation of the extrahepatic biliary tree (80%)
Ia- Proximal dilation. The gallbladder arises from the cyst itself.
Ib- Dilatation of the distal common bile duct.
Ic- Fusiform dilation of common bile duct and liver.
• Type II: Saccular diverticulum in common bile duct
• Type III: Dilation of the intraduodenal portion of the common bile duct (Choledochocele)
• Type IV: Multiple cysts of the biliary tree (20%)
IVa- multiple intra and extrahepatic cysts.
IVb- multiple extrahepatic cysts.
• Type V: Simple or multiple dilations of the intrahepatic bile ducts without dilatation of the common bile duct. (Caroli disease).
80% are diagnosed before the age of 10, 30% in the first year of life and, only 20% in adulthood [2] although the etiology is unknown, the anomaly in the biliopancreatic junction is the most accepted theory.
The development of a biliopancreatic duct that is longer than normal conditions chronic reflux of pancreatic secretions into the bile duct (the pressure of the pancreatic duct exceeds that of the bile duct) that cause inflammation and fibrosis of the same and, secondarily, its dilation [3-6].
In a small group of infants, choledochal cysts are part of a spectrum of childhood obstructive cholangiopathies that includes neonatal hepatitis and biliary atresia.
The clinical spectrum varies depending on the age range. Patients under one year of age usually present with obstructive jaundice and abdominal mass with symptoms, sometimes severe, in the neonatal period. In older patients, symptoms are often nonspecific, the usual symptoms are abdominal pain, with or without cholestasis, and may be accompanied by vomiting, frank jaundice, and/or cholangitis.
The classic triad of jaundice, abdominal pain, and palpable mass occurs in only one-third of older patients [3,4].
Pancreatitis, uncommon in pediatric age, can be the clinical presentation in both age ranges. Possible complications include recurrent pancreatitis, stone formation in the cyst, peritonitis secondary to rupture of the cyst and, cholangiocarcinoma [3,6,7].
Ultrasound is the initial diagnostic test of choice. A cystic mass in the porta hepatis, separated from the gallbladder, into which the common bile duct empties, confirms the diagnosis [6,8]. The differential diagnosis should be made with the intestinal duplication cyst by identifying the typical characteristic layered wall, similar to the normal intestinal wall.
Scintigraphy confirms communication with the biliary tree in cases of doubt and is useful in newborns to exclude airway atresia if its association is suspected. Endoscopic cholangiopancreatography (ERCP) and MR cholangiopancreatography (MRCP) make it possible to determine the anatomical connections, which are of great importance for the surgical approach [1,7-9].
MRCP can replace ERCP since, although sedation is necessary in most cases to perform it, it is a non-invasive test that does not produce complications and does not radiate.
Treatment depends on the type of cyst. Complete resection is recommended, whenever possible, in type I. In type IV, an attempt should be made to remove at least those from the extrahepatic route. Cyst resection does not eliminate the possibility of developing carcinoma in the intrahepatic ducts, so long-term follow-up is necessary [6,10].
In the presented case, ultrasound was very useful in the initial diagnosis, allowing to assess the thickening of the gallbladder wall in response to chronic inflammatory changes. The RC allowed to confirm the diagnosis of the cyst and to typify it according to the Todani classification as well as to reveal the relationship with the rest of the anatomical structures and to demonstrate the presence of lithiasis, a rare finding.
References
- Giha S, Redondo Y, Quintero G (2016) Choledochal cyst: Intraoperative diagnosis and management. Pediatric 49: 64-67.
- Kim H, Chung HJ, Choi BG (1995) Imaging of the choledocal cyst. Radiographics 15: 69-88.
- Emery KH (2010) Cross-sectional imaging of pediatric biliary disorders. Pediatric Radiology 40: 438-441.
- Topazian M D Biliary cyst.
- Iwai N, Yanagihara J, Tokiwa K, et al. (1992) Congenital choledochal dilatation with emphasis on pathophysiology of the biliary tract. Ann Surg 215: 27-30.
- Palmer-Becerra J D, Ulloa- Patino P (2010) Treatment of choledochal cysts in children. A 24 year review. Acta Pediatrica de Mexico 31: 11-15.
- Bedregal-Mendoza T, Matos-Rojas IA, Diaz Gonzales JE, et al. (2015) Acute pancreatitis in childhood by choledocal stone in a choledocal cyst. Case report. Rev Gastroenterol Peru 35: 173-178.
- Donnelly LF (2009) Pediatric Imaging. The fundamentals. Chapter 5.
- Darge K, Anupindi S (2009) Pancreatitis and the role of US, MRCP and ERCP. Pediatr Radiol 39: S153-S157.
- Todani T (1997) Congenital choledochal dilatation: Classification, clinical features, and long-term results. Journal of Hepato-Biliary-Pancreatic Surgery 4: 276-282.
Corresponding Author
Maria Teresa Garzon Guiteria, Pediatric Radiology Department, University Hospital of Salamanca, Spain
Copyright
© 2022 Guiteria MTG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.