Acute Pancreatitis Secondary to Congenital Duodenal Web
Introduction
The duodenum at 30-60 days of gestation is a solid tube that is later recanalized. When this process is interrupted, there may be a total absence of recanalization leading to duodenal atresia (50% of cases) or incomplete recanalization leading to duodenal stenosis (10% of cases). When this process is interrupted, duodenal atresia (absence of recanalization) occurs in 50% of cases or duodenal stenosis in 10% (incomplete recanalization). The causal mechanism is unknown, although it is believed that the entry of the pancreatic and bile ducts may affect recanalization, which would explain the location of the stenosis at the level of the ampulla of Vater [1].
Duodenal obstruction is the most frequent cause of upper obstruction in newborns and the diagnosis generally occurs in the first days of life with a picture of food vomiting and sometimes abdominal distension and a "double bubble" image (dilated stomach and duodenum) on the abdominal X-ray. The presence of polyhydramnios and the dilation of the stomach and duodenum seen in the ultrasound study allows for prenatal diagnosis.
The duodenal membrane constitutes 40% of cases of stenosis and can be complete or more frequently incomplete. This means that in many cases the course is long and the diagnosis late.
In 50% of cases of duodenal stenosis there are other associated congenital anomalies, anorectal, biliary, cardiac and genitourinary among others [2-4].
Case Report
A 16-month-old infant came to the emergency room for vomiting and colicky abdominal pain. In the laboratory analysis, a lipase elevation more than three times the normal value (641 u/l) stood out, for which reason he was admitted with suspicion of acute pancreatitis.
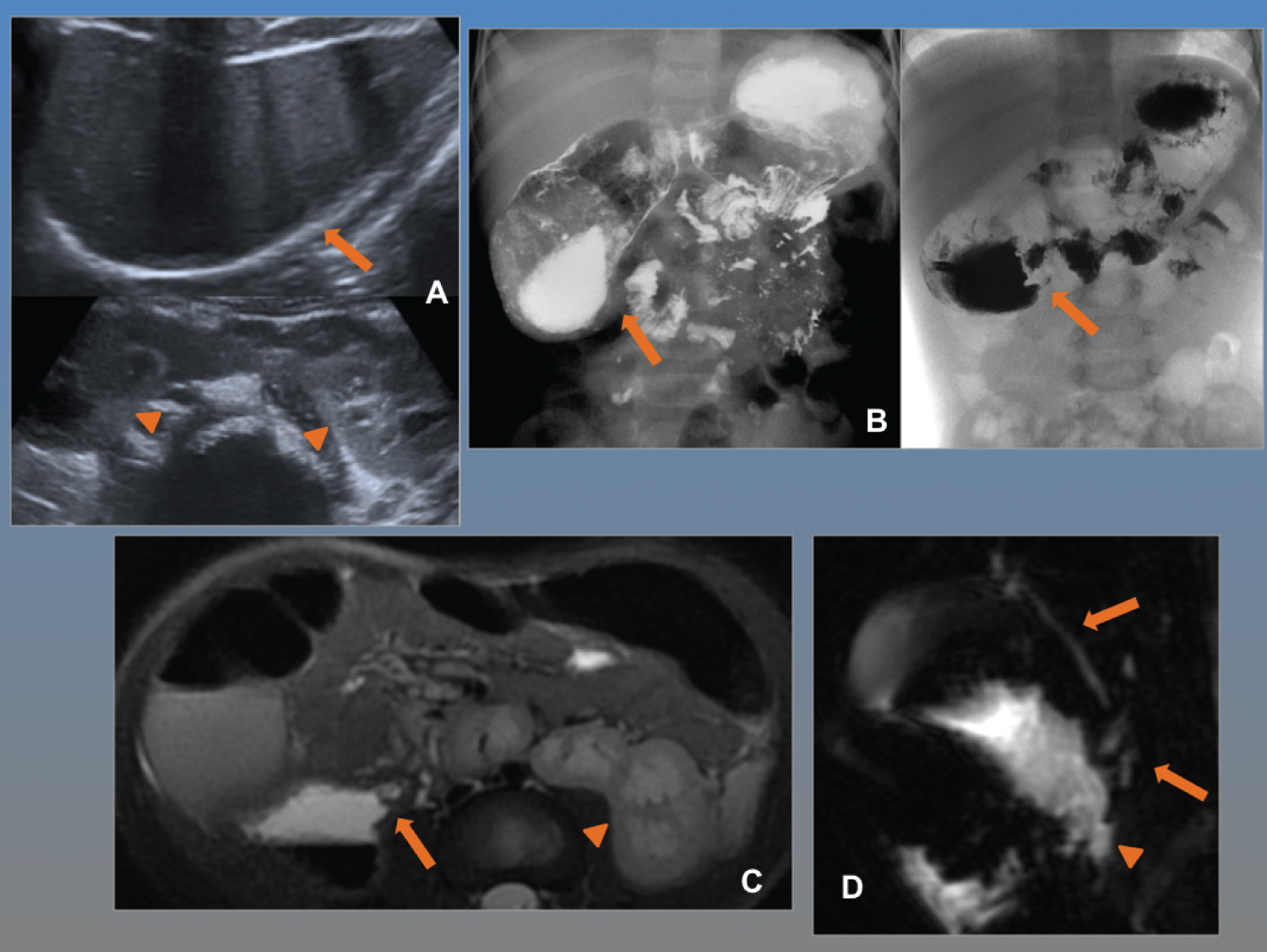
The abdominal ultrasound performed to rule out pancreatic complications shows a pancreas with normal echo structure without intra- or peripancreatic collections. There is no lithiasis or dilation of the bile duct. In the midline, in gastro duodenal topography, an image of cystic appearance is observed, with liquid content and layered wall of enteric appearance that raises differential diagnosis with gastric duplication cyst or dilated duodenum. A horseshoe kidney was found as an additional finding (Figure 1A).
The gastroduodenal study is performed with administration of oral contrast that shows a stomach of normal morphology, with slow emptying to a duodenum that is severely progressively dilated (and corresponds to the image visualized in the ultrasound study), due to incomplete stenosis in the junction of the second-third portion of the duodenum. Contrast slowly passes to the rest of the intestinal loops, which retain normal morphology and the duodenojejunal junction is in a normal position, which rules out associated intestinal malrotation (Figure 1B).
The study is completed with abdominal resonance and cholangioresonance to adequately assess the pancreatic ducts and rule out other congenital alterations added to the renal anomaly. Duodenal stenosis is confirmed, immediately after the ampulla of Vater, where the normal bile duct and pancreatic duct drain, considering this anatomical confluence as a cause of pancreatitis due to compressive effect and/or possible reflux of contents to the pancreatic duct (Figure 1C and Figure 1D).
The patient underwent surgery performing a duodenojejunostomy with the diagnosis of duodenal membrane stenosis, with a favourable clinical evolution.
Discussion
Acute pancreatitis is an inflammatory condition of the pancreas affected by interstitial edema, necrosis, and haemorrhage in different degrees, potentially reversible. It is rare in the pediatric age, although in the last decade, there has been an increase in incidence with an approximate annual percentage of 1-13 cases per 100,000.
According to the INSPPIRE (International Study Group of Pediatric Pancreatitis: In Search for a Cure) criteria, the diagnosis of pediatric acute pancreatitis is made when at least two of the following are present: (1) Abdominal pain that suggests or is compatible with acute pancreatitis, (2) Serum amylase and/or lipase at least three times the upper limit of normal (IU/ml), and (3) Imaging findings characteristic of or consistent with acute pancreatitis (using any modality) [5,6].
Both the etiology and the clinical course and prognosis are different compared to the adult population. Abdominal trauma is the most frequent cause (10-40%). Generally, they are due to a direct hit with the bicycle handlebar that injures the main pancreatic duct, favoured by the low amount of abdominal fat that prevents cushioning, and less frequently by accident of traffic. Non-accidental trauma accounts for a third of cases and should be considered when there is no justifying cause in the medical history.
Gallstones account for 3-30% of cases. Drug toxicity, autoimmunity, infections, and multisystemic diseases are possible etiologies. Congenital pancreaticobiliary abnormalities such as abnormal pancreaticobiliary junction, annular pancreas, pancreas divisum are rare, and the duodenal membrane is a rare cause and is generally associated with recurrent acute pancreatitis or chronic pancreatitis.
The main symptom is abdominal pain and secondly nausea and vomiting. In infants, abdominal distension, malaise, and irritability are associated with vomiting and fever predominating. The imaging techniques commonly used in the diagnosis are abdominal ultrasound, as an initial study, which allows assessing the echo structure of the pancreatic parenchyma, the presence of liquid collections at this level, or peripancreatic and gallstones.
CT is useful in cases of poor evolution to rule out complications and magnetic resonance imaging for a correct anatomical view of the bile and pancreatic ducts [4].
As mentioned above, the duodenal membrane is frequently incomplete, which determines a larvae clinic, with sporadic vomiting or nonspecific abdominal pain, which makes the diagnosis of this entity difficult. In the case of our patient, a meticulous anamnesis revealed 7 previous visits from the first month of life, for self-limited episodes of vomiting, which on some occasions associated dehydration and transient acute renal failure and which were attributed to gastro paresis. An increase in the same was also observed, with the increase in the number of feedings according to the child's growth, which in recent months associated rejection of the intake, with the consequent decrease in weight-bearing growth and antalgic sleeping position (fetal position with legs and trunk flexed).
It is a rare cause of acute pancreatitis, but in cases such as the one presented, in which the duodenal dilation is severe and the stenosis is located immediately after the ampulla of Vater, it can be caused by compressive effect and/or reflux of intestinal contents into the duct pancreatic.
When the onset is suspected, an abdominal X-ray can be performed, which will show findings similar to those of atresia, with a double-bubble image, when the obstruction is complete, or a retained stomach or duodenal dilation when it is incomplete.
Ultrasound also allows us to assess this finding, as in our case, since duodenal dilation is evident thanks to its liquid content and with dynamic assessment, the area of stenosis can sometimes be determined. It is useful in the assessment of associated congenital anomalies, the most frequent of which are renal, including polycystic disease, renal agenesis, or, as in our case, the horseshoe kidney. It is a starting point for the indication of a gastroduodenal study that will make it possible to assess the obstruction and locate the duodenojejunal junction and rule out associated malrotation [2].
Abdominal MRI with cholangioresonance allows assessment of associated congenital anomalies and, in our case, confirmation of pancreatitis, assessment of the morphology and arrangement of the pancreatic ducts and the biliary tree, as well as associated complications.
Conclusion
• Acute pancreatitis is rare in children, although the incidence has increased in the last decade. The etiology is varied, being abdominal trauma the most frequent cause and gallstones the pharmacological toxicity, autoimmunity, infections and multisystemic diseases other possible etiologies. Congenital anomalies, although rare, should always be considered.
• The duodenal membrane is a rare cause of acute pancreatitis caused by compression effect and/or reflux of intestinal contents into the pancreatic duct.
• The radiological study of choice is the gastro duodenal one that allows confirming the obstruction and ruling out intestinal malrotation. Abdominal ultrasound as an initial study provides great information on the morphology of the intestinal loops, the disposition of the mesenteric vessels, and the assessment of associated congenital anomalies, and constitutes a starting point for scheduling the rest of the imaging studies.
• Cholangioresonance allows assessing common bile duct, toilet blister, pancreatic ducts and their anatomical relationship with the duodenal membrane.
• This entity should be considered in the face of repetitive episodes of self-limited vomiting, especially in children with associated congenital anomalies, in which a correct and detailed anamnesis constitutes a key point in the diagnosis.
References
- Boyden EA, Cope JB, Bill AH (1967) Anatomy and embryology of congenital intrinsic obstruction of duodenum. Am J Surg 114: 190-202.
- Berrocal T, Gaya F, De Pablo L (2005) Aspects of embryologic clinical and radiological intestinal malrotation. Radiologic 47: 237-251.
- Cano Munoz I, Montoya Mendoza N (2011) Obstruction duodenal of patient's pediatrics. Annals of Radiologic Mexico 4: 258-273.
- Sofia C, Loreley G, Damian P (2019) Desnutrición crónica como manifestación de membrana duodenal congénita. Arch Pediatr Urug 90: 210-214.
- Artunduaga M, Grover AS, Callahan MJ (2021) Acute pancreatitis in children: A review with clinical perspectives to enhance imaging interpretation. Pediatr Radiol 51: 1970-1982.
- Morinville VD, Husain SZ, Bai H, et al. (2012) Definitions of pediatric pancreatitis and survey of present clinical practices. J Pediatr Gastroenterol Nutr 55: 261-265.
Corresponding Author
Maria Teresa Garzón Guiteria, Pediatric Radiology Department, University Hospital of Salamanca, Spain.
Copyright
© 2022 Guiteria MTG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.