Abscessed Gastric Gastrointestinal Stromal Tumor (GIST): A Case Report
Introduction
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors of the gastrointestinal tract. Although GISTs can appear at any gastrointestinal tract location, they are usually found in stomach (60%-70%), followed by small bowel (20%-30%). Less frequently, they can appear in colon, rectum, appendix, esophagus, mesentery, omentum, or retroperitoneum [1,2].
Surgical resection is the main stay in the treatment of gastric non-metastatic GIST. Their peculiar characteristic of growth and poor metastatic tendency make them good prognosis tumors. Whose surgical management may be less aggressive.
This case report describes a patient with a gastric GIST complicated with a big intratumoral abscess.
Case Presentation
A 51-year-old man, who had no relevant medical history, attended the hematology service to study anemia. The protocol included the performance of abdominal ultrasound, which showed a large heterogeneous epigastric mass with a thickened wall, a solid component and a central liquid component.
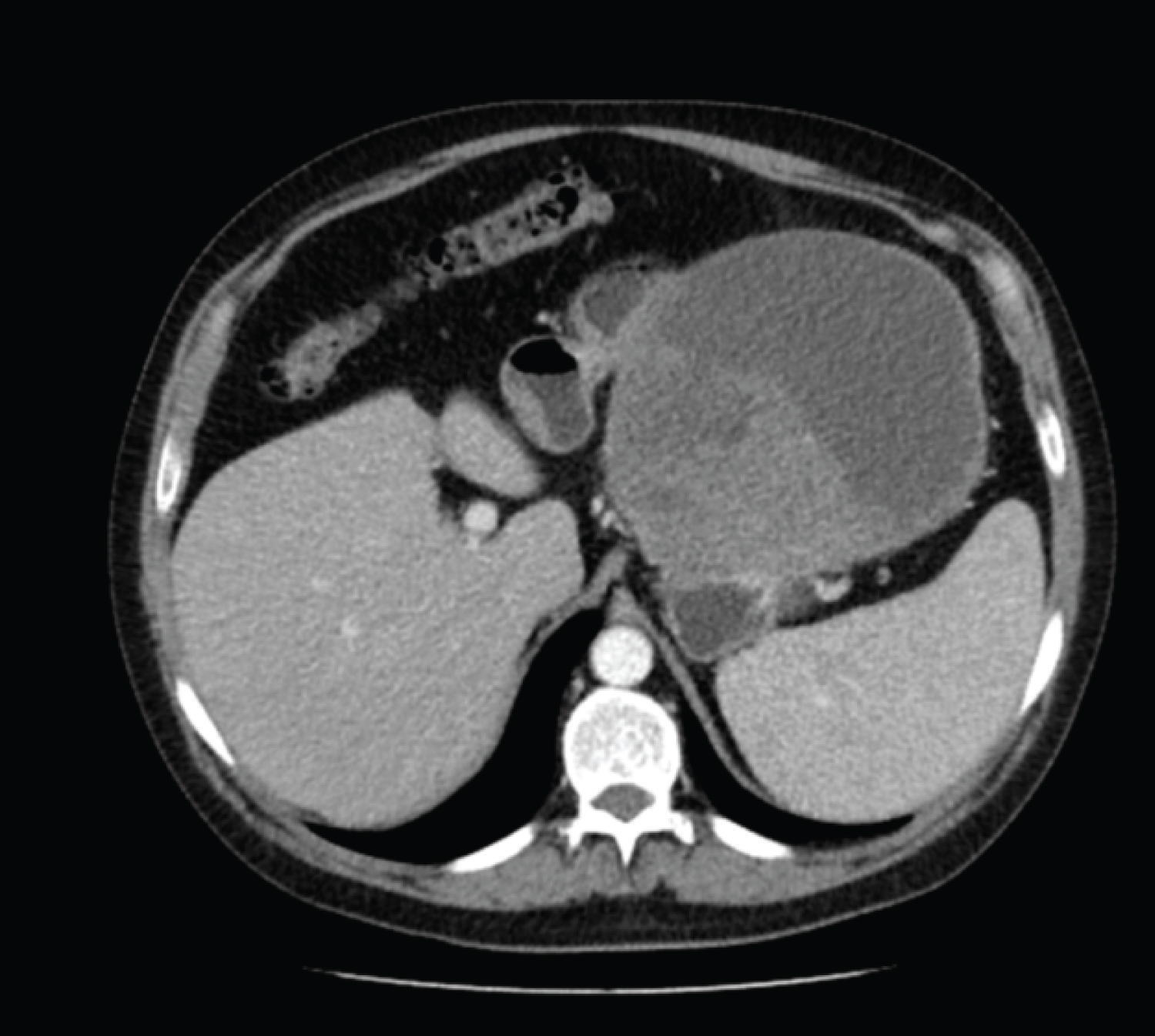
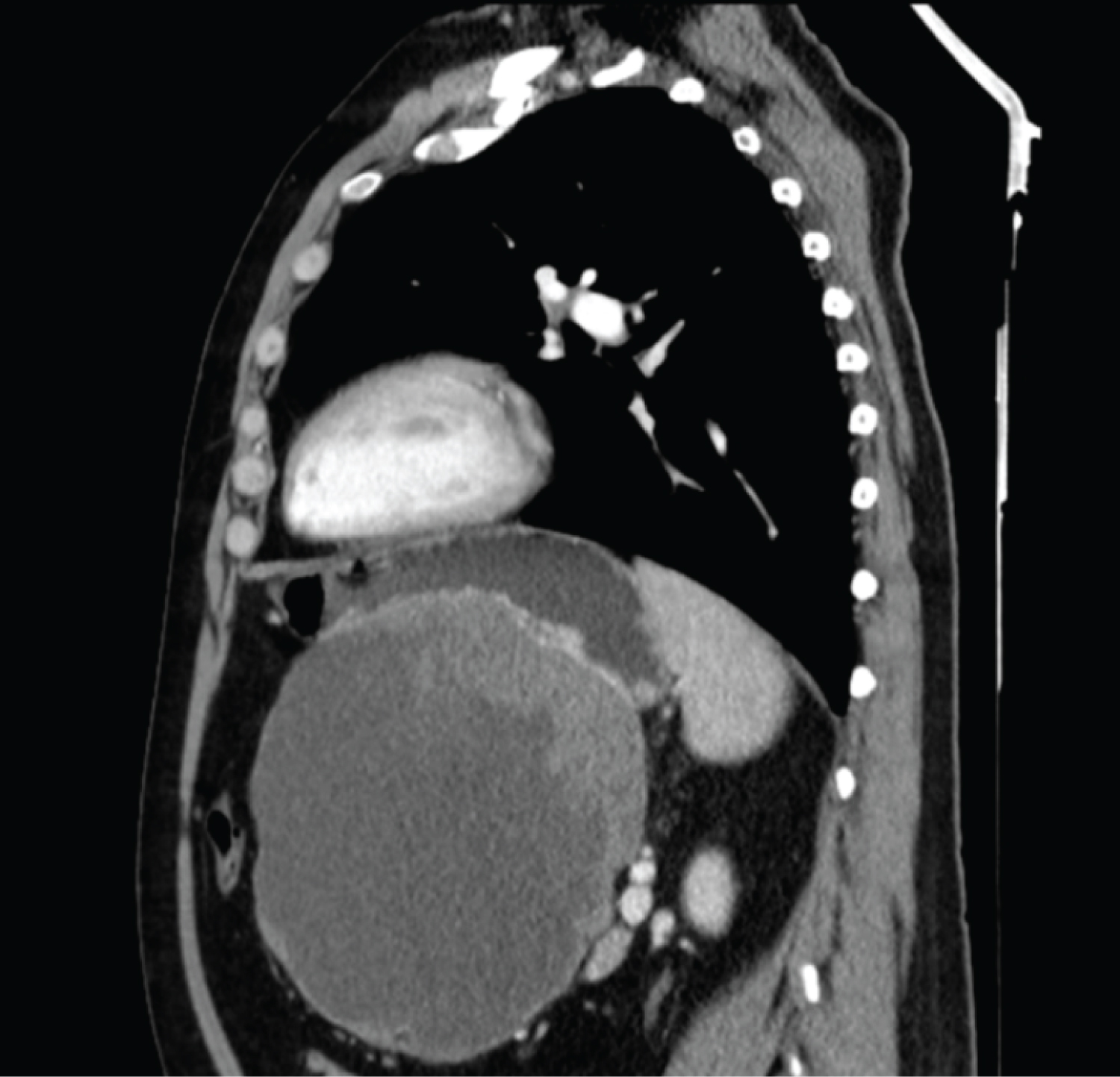
Enhanced Abdomen CT
Epigastrium mass size messurements 17.6 × 15.7 × 8.5 cm (T × AP × CC) that depended on the posterior wall of the gastric body, it presents an exophytic growth, central cavitation partially filled with fluid and with slight enhancement of solid areas (Figure 1 and Figure 2). No other visceral abnormalities were found.
Endoscopic FNA
It showed gastrointestinal stromal tumor (GIST). IHC study: C-kit +, Dog-1 +, CD34 +, actin -, S100 -, desmin-. Proliferative index (ki-67) < 1%.
Treatment
Supraumbilical median laparotomy: It showed a large tumor (approximately 20 cm) which depended on the stomach, of a cystic nature with malodorous content, which was fistulizing with the posterior gastric side, and contacted the pancreatic capsule and transverse colon.
Aspiration of abscessed content was performed with a total of 5 liters, and once it was completely emptied, a fragile cerebriform tumor was found in contact with the posterior gastric face.
It is not observed that this mass depends on the stomach (intraoperative gastroscopy).
Total gastrectomy is performed after dissection of the wall of the esophageal section with endogia and Roux-en-Y reconstruction.
Histological postoperative
Cavitated and fistulized gastrointestinal stromal tumor (GIST) to the gastric mucosa with central necrosis. It measured 22 × 20 cm. 10% risk of progression, spindle cell pattern and a mitotic index of 1 mitoses per 5 high power fields, were also described. Immunophenotype analysis revealed CD117 +, DOG1 +, CD34 +, actina -, desmina -, S100 -. Fourty tumor free lymph nodes were analyzed.
Microbiological analysis
It grew Streptococcus constellatus.
The postoperative evolution was uneventful and the patient was discharged seven days after surgery.
Discussion
GIST are rare tumors of the gastrointestinal tract, accounting for less than 1% of all gastrointestinal tract tumors. It most commonly arises in the stomach (60%) and the small intestine (30%). Less frequently, they can occur in the colon, rectum, appendix, esophagus, mesentery, omentum, orretroperitoneum [1,2].
Often show an exophytic growth pattern, so they tend to be asymptomatic until they grow large. The clinical presentation of the GISTs is highly variable. The most frequent symptoms are gastrointestinal bleeding, abdominal pain, a palpable mass, weight loss, and fever. Infrequently, GISTs cause acute abdomen such as bowel obstruction, hemoperitoneum secondary to tumor rupture, and peritonitis secondary to tumor perforation. Cases with intratumoral abscess formation are also rare.
When an abscess bearing a thick and hypervascularized wall is observed at contrast-enhanced CT scan, as in our case, an intratumoral abscess should be suspected. GISTs should be listed as a differential diagnosis.
The mechanism of intratumoral abscess formation is considered to comprise enteric bacteria entering through the fistula infected with necrotic tissue inside the tumor and developing into an intratumoral abscess. Streptococci, Staphylococci, E. coli, Haemophilus influenzae, Proteus and Closttridium are the most common pathogens.
Complete surgical resection is the only potential curative treatment for GISTs. Whereas small GISTs (5 cm or less) can be treated by gastric resection, larger tumors may require subtotal or total gastrectomy, including omentectomy. Gentle handling is necessary because injury of the pseudocapsule may cause dissemination of the tumor cells. In cases with intratumoral abscess, dissection with extreme care is necessary because the pseudocapsule is expected to be fragile with inflammation. Metastatic or unresectable GISTs are treated with Imanitib mesylate (STI571), a small molecular tyrosine kinase inhibitor of KIT [3,4].
References
- Ito S, Tsuchitani Y, Kim Y (2018) A gastrointestinal stromal tumor of the jejunum presenting with an intratumoral abscess: A case report and a literature review. Int J Surg Case Rep 48: 65-68.
- Osada T, Nagahara A, Kodani T, et al. (2007) Gastrointestinal stromal tumor of the stomach with a giant abscess penetrating the gastric lumen. World J Gastroenterol 13: 2385-2387.
- Demetri GD, Mehren MV, Antonescu CR, et al. (2010) NCCN task force report: Update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw 8: S1-S41.
- Lai ECH, Lau SHY, Lau WY (2012) Current management of gastrointestinal stromal tumors--a comprehensive review. Int J Surg 10: 334-340.
Corresponding Author
Sonia Yáñez Castaño, MD, Department of Radiology, Salamanca University Hospital, Paseo de San Vicente, 182, 37007 Salamanca, Castilla y León, Spain, Tel: +34-669837883.
Copyright
© 2021 Castaño SY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.