Liver Abscess Secondary to Ingestion of Chicken Bone
Abstract
Ingestion of foreign bodies is very common in routine clinical practice. They are usually secreted spontaneously, but in a small percentage they cause complications such as gastrointestinal perforations that can migrate causing abscesses.
Given the nonspecific symptoms of these patients, it is important to take an anamnesis and complete the clinical suspicion with radiological tests (CT), requiring exploratory laparotomy for definitive diagnostic confirmation.
Introduction
Ingestion of foreign bodies is very common in routine clinical practice. Most of these cases occur in children, but also in a considerable number of psychiatric, disabled, or elderly patients with dentures. 80-90% of foreign bodies are spontaneously excreted without repercussions [1], but at least 1% of cases present complications such as gastrointestinal perforations, with the formation of secondary abscesses infrequent [2,3].
The clinical presentation is nonspecific and is often confused with abdominal inflammatory processes which make early diagnosis difficult [4].
Abdominal CT is the initial test of choice with a sensitivity of 100% [5] requiring exploratory laparotomy for definitive diagnostic confirmation.
Clinical Case
We present the case of a male patient with a history of insulin-dependent type 2 DM and dyslipidaemia. He went to the emergency department due to a week-long fever with a torpid evolution despite antipyretic treatment.
In the initial examination, the patient is bradypsychic, tachypneic, normotensive and with a fever of 40°. Physical examination is unremarkable except for mild epigastric tenderness on palpation.
Laboratory tests show mild neutrophilia with a CRP of 18 mg/l and a slightly altered liver profile LDH: 486 U/l, GOT: 92 IU/l GPT: 60 IU/l, Alkaline Phosphatase: 610 IU/l, GGT: 54 IU/l, the rest being normal analytical parameters. Plain abdominal X-ray shows no abnormalities.
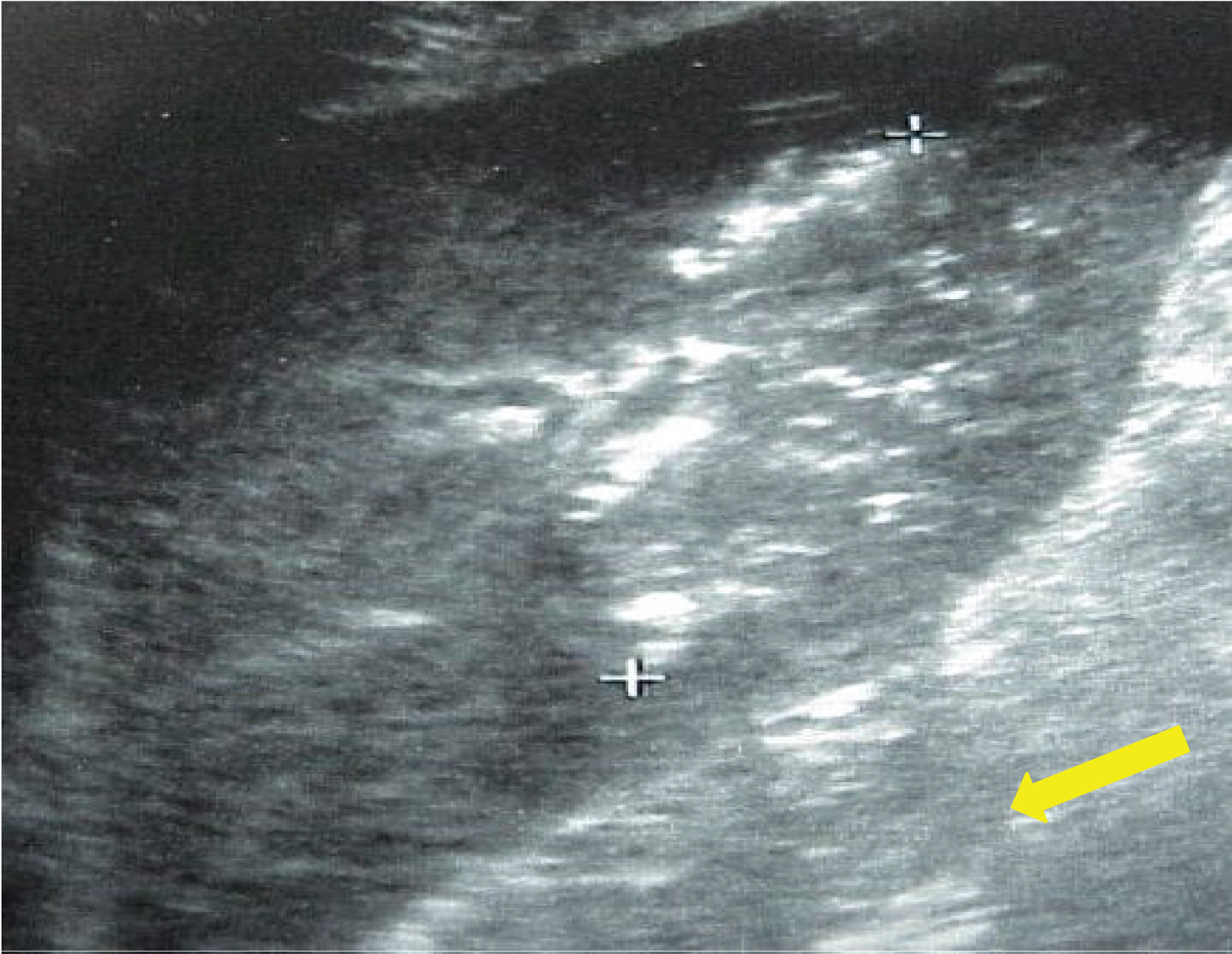
Given the nonspecific abdominal symptoms, an imaging test is requested. Initially, an abdominal ultrasound is performed where multiple echogenic images with a descending ring artifact are observed in the left liver lobe that suggests the presence of gas (Figure 1).
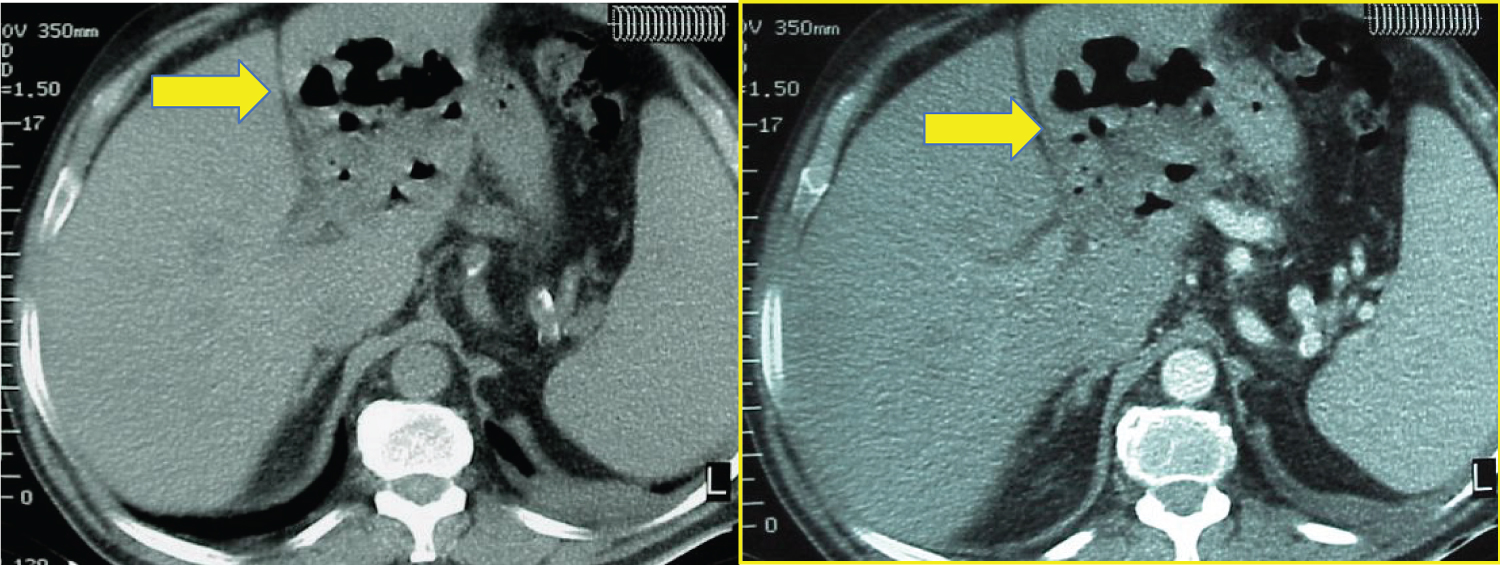
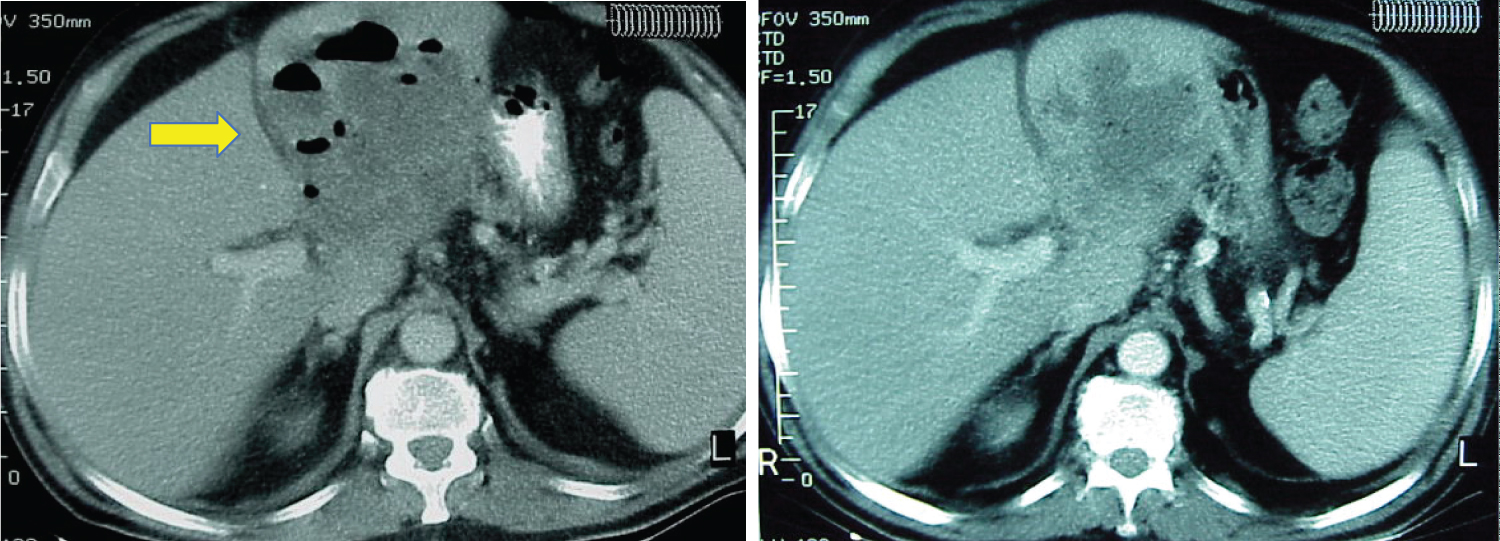
Taking these findings into account, an abdominal CT scan was performed that shows a 9 × 10 cm collection with air inside and peripheral enhancement that guides the diagnosis of liver abscess (Figure 2 and Figure 3).
Initial conservative treatment was decided with administration of broad spectrum penicillin (Piperacilin-Tazobactam) and metronidazole together with drainage with ultrasound control.
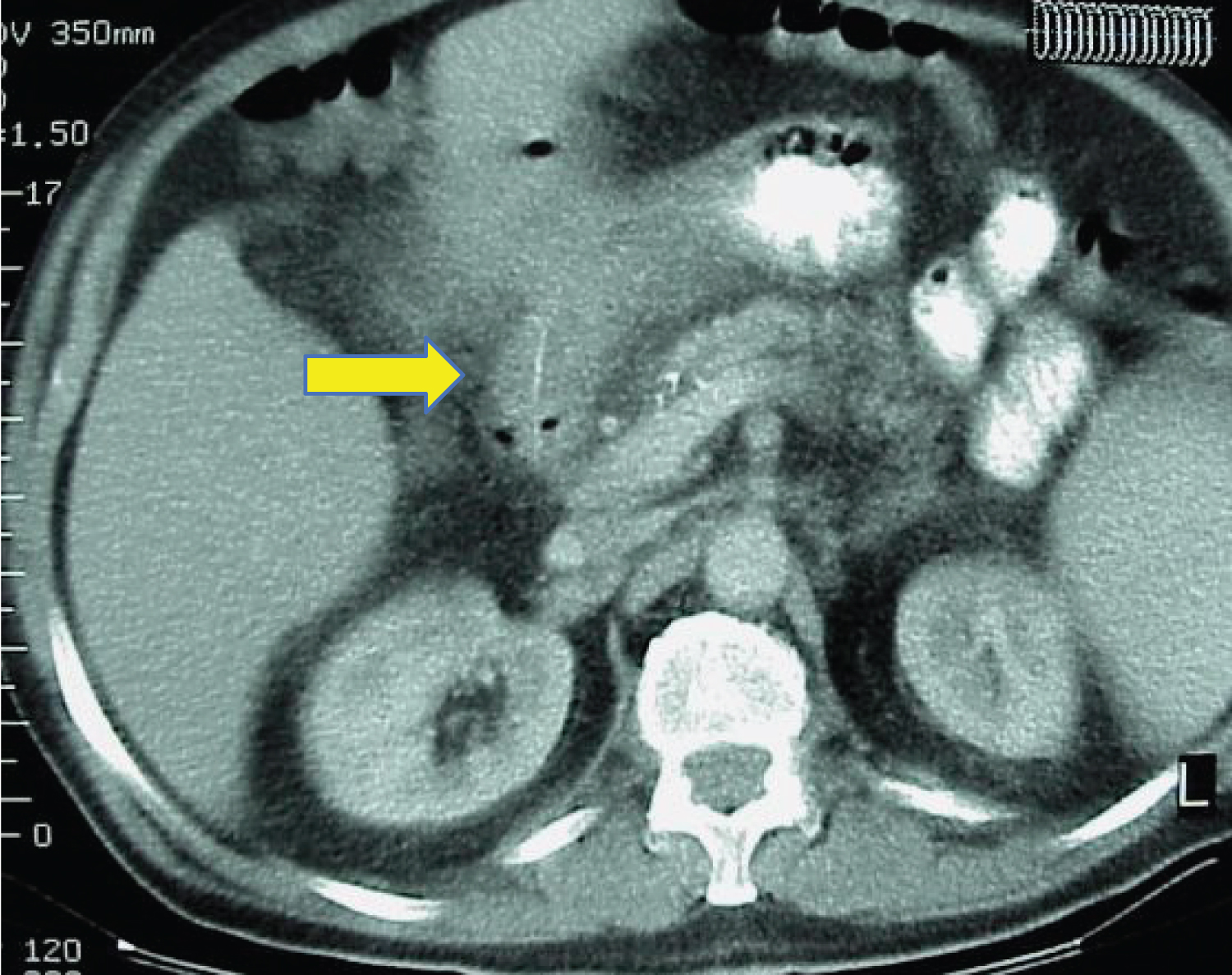
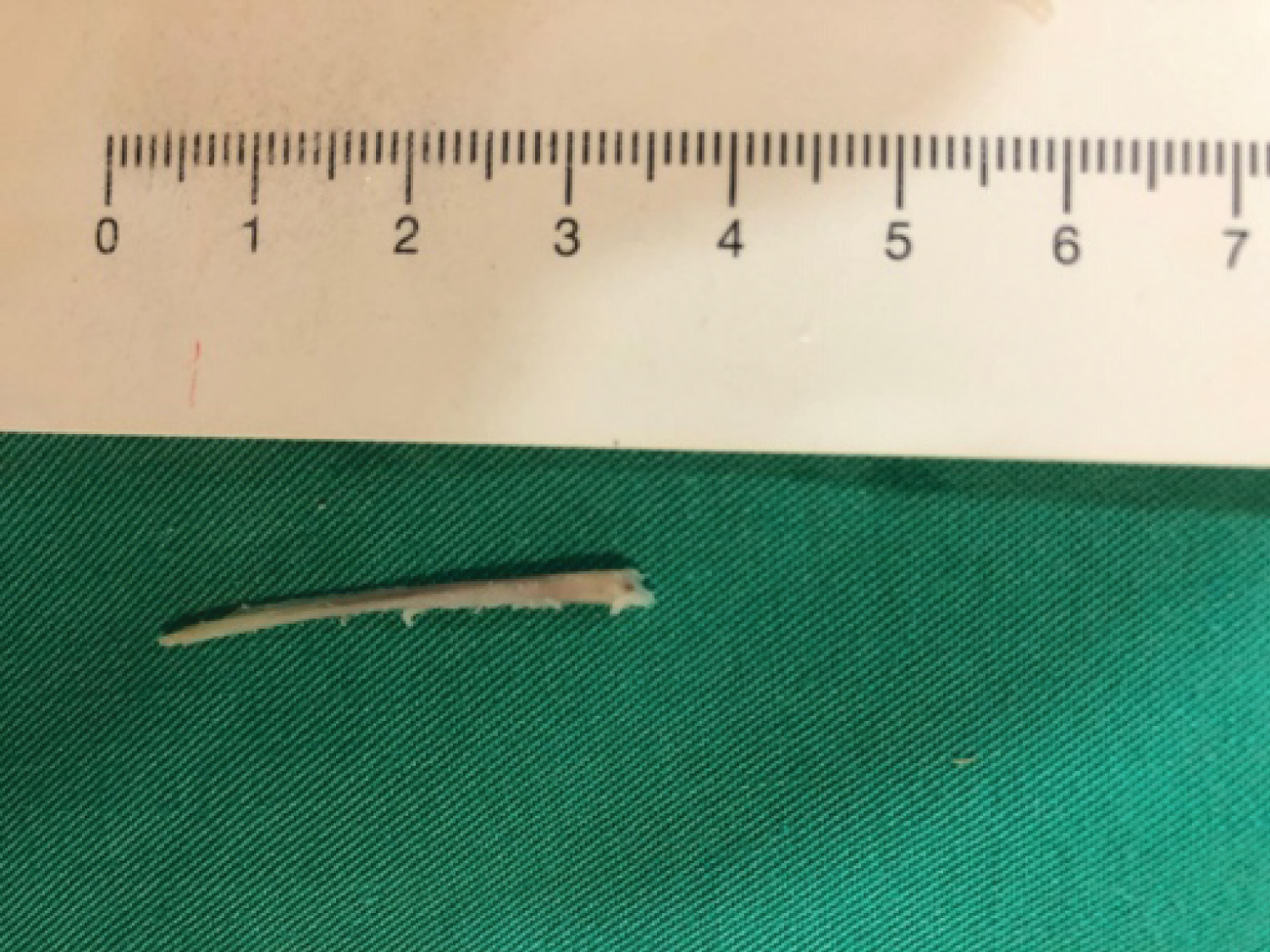
The evolution is torpid with progressive increase of the abscess despite treatment with drainage and antibiotic therapy (Figure 4 and Figure 5), for which an exploratory laparotomy was decided with cleaning of the area, finding as an incidental finding a migrated chicken bone through a perforation produced at the level of the pylorus (Figure 6 and Figure 7).
Discussion
The incidence of intestinal perforation due to foreign body ingestion is less than 1% [2,3]. Sometimes after perforation they can migrate to adjacent organs with the result of fistulization, abscess formation or sepsis.
These perforations are usually produced by fish bones, followed by chicken bones or various bone fragments, in addition to other objects such as toothbrushes, toothpicks or dentures [4].
Perforation tends to affect bowel segments with greater angulation, the most common being the ileocecal junction and the rectosigmoid region.
The symptoms are usually nonspecific, presenting as abdominal pain, intestinal obstruction or renoureteral colic, [5] and it can have a variable duration, reaching months after ingestion [6].
The abdominal X-ray is generally nonspecific and on many occasions, the abdominal CT does not initially detect the foreign body, although it does retrospectively as it happened in our case. The sensitivity of abdominal CT is conditioned by the index of suspicion and can sometimes be confused with other structures such as a blood vessel [5].
Exploratory laparotomy allows the final diagnosis.
Conclusion
Liver abscess due to perforation after ingestion of a foreign body is very rare and the symptoms are usually nonspecific. This makes a high clinical suspicion necessary after a detailed anamnesis, even more so when the symptoms can take months to appear after ingestion of the foreign body. In many cases, exploratory laparotomy is essential for the diagnosis.
References
- Wang Z, Du Z, Zhou X, et al. (2020) Misdiagnosis of peripheral abscess caused by duodenal foreing body: A case report and literature review. BMC Gastroenterology 20: 236.
- Radicic K, Dorsey JT, Greco R (2019) Gastric perforation after chicken bone ingestion. Case Rep Gastrointest Med 2019.
- Sidiqi MM, Sharma S, Muhammed AH (2019) Endoscopic management of gastric perforation secondary to chcken bone: A report of 2 cases. Int J Surg Case Rep 65: 305-308.
- Kuzmich S, Burke CJ, Harvey CJ, et al. (2015) Perforation of gastrointestinal tract by poorly conspicuous ingested foreign bodies: Radiological diagnosis. Br J Radiol 88.
- Sibanda T, Pakkiri P, Ndlovu A (2020) Fish bone perforation mimicking colon cancer: A case report. SA J Radiol 24: 1885.
- Chi Li, Chee-Chien Yong, Domelle Dave Encarnación (2019) Duodenal perforation nine months after accidental foreign body ingestion, a case report. BMC Surgery 19: 132.
Corresponding Author
Garzón Guiteria P, Emergency Service, Ourense University Hospital Complex, CHUO, Ramón Puga 52, 32005, Ourense, Spain
Copyright
© 2020 Garzón GP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.