Intestinal Malrotation as a Cause of Chronic Recurring Abdominal Pain in Adult with Caudal Regression Syndrome
Introduction
The term intestinal malrotation comprises a spectrum of developmental abnormalities of the midgut secondary to an alteration in the rotation of the loops and/or fixation of the mesentery.
During embryological development, the midgut undergoes a process of growth and lengthening, which begins at week 5 of gestation and ends shortly after birth and also includes herniation in the umbilical cord, rotation, reduction and fixation. Rotation occurs counterclockwise around the superior mesenteric artery and ends at week 12, at which time the intestine re-enters the abdominal cavity and is attached to the parietal peritoneum, with different anchor points. If the rotation is not correct, a good fixation is not possible. The second, third, and fourth portions of the duodenum, the ascending and descending colon, attach to the retroperitoneum. The duodenojejunal junction is fixed by the ligament of Treitz and the small intestine by a wide meso that extends from that ligament to the ileocecal valve [1-3].
Malrotation is caused by a malposition of the loops that is accompanied by their malfunction, which generates an increased risk of intestinal obstruction and acute or chronic volvulus [4].
Depending on when the rotation failure occurs, it is classified into:
Non-rotation: The midgut returns to the abdominal cavity when it has only rotated the first 90°. The duodenum-jejunal loop is located to the right of the abdominal cavity, colon and cecum to the left of the abdominal cavity and the distal ileum crosses the middle line from right to left to reach the cecum. It is the most frequent type.
Incomplete intestinal rotation: Failure occurs during the counterclockwise rotation of the last 180° of the small intestine or colon. The intestine occupies an intermediate position between non-rotation and the normal end situation. Aberrant fibrous bands (Ladd's bands) are generated that anchor the malpositioned cecum to the retroperitoneum, passing in front of the duodenum; the proximity of the proximal and distal mesentery attachment points around the mesenteric vessels favors spontaneous volvulation of the small intestine.
Reverse rotation: It is the rarest and constitutes a true malrotation. The posteroarterial segment of the midgut re-enters the abdominal cavity before the prearterial segment, so that the colon is posterior to the superior mesenteric artery and the duodenum is anterior to it [3].
Case Report
We present the case of a 23-year-old woman with paraplegia secondary to caudal regression syndrome and a history of bladder lithiasis related to her neurogenic bladder.
She came to the emergency room due to colicky pain in the right upper quadrant and a recent-onset 39-degree fever. Urinalysis is compatible with urinary tract infection and CRP is elevated (27 measured value).
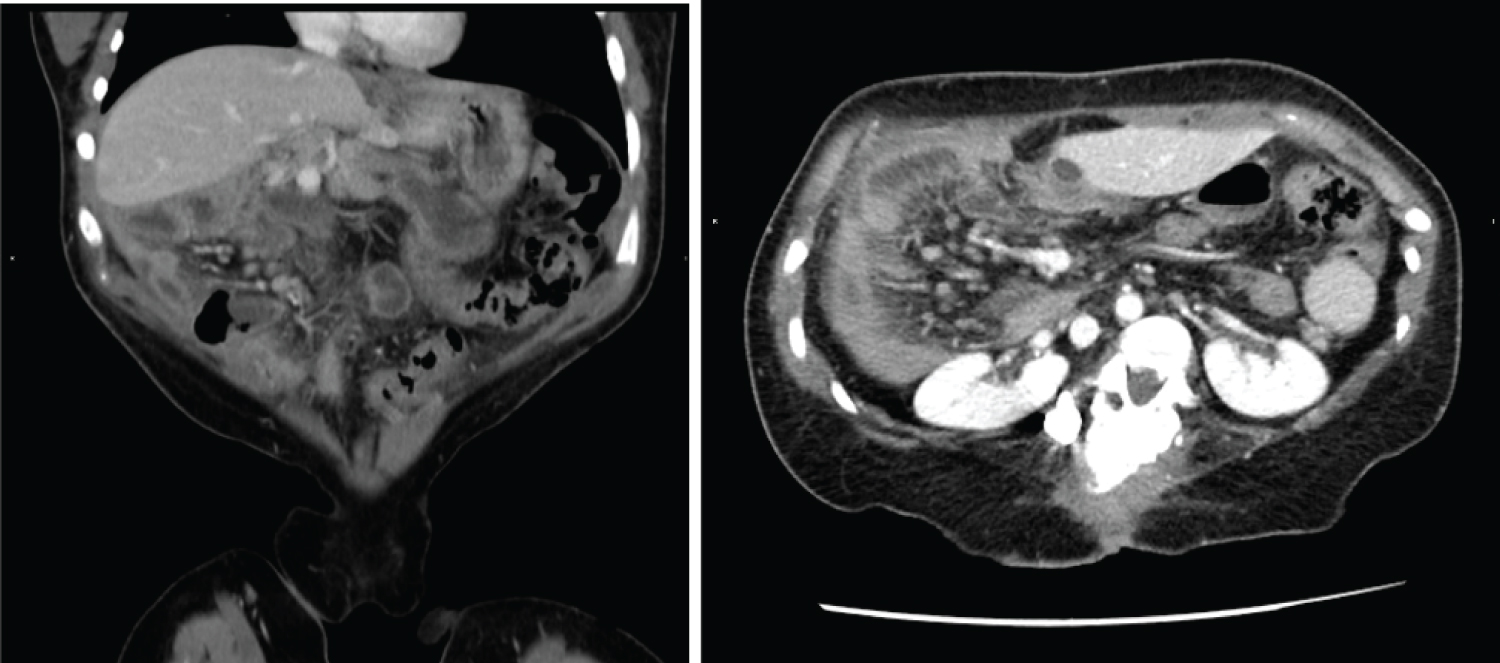
Abdominal CT scan with intravenous contrast administration is requested to rule out pathology of the urinary tract. The study rules out lithiasis in the urinary tract but reveals an abnormal location of the small bowel loops that are grouped in the right hemiabdomen, with abundant liquid content and gauge at the upper limit of normal. The large intestine is located in the left hemiabdomen with the cecum at the hypogastric level. The superior mesenteric vein is located anterior to the superior mesenteric artery and there is significant vascular engorgement of the mesentery (Figure 1, Figure 2 and Figure 3).
As additional findings, the concomitance of polysplenia and the alteration in the rotational axis of both kidneys should be noted.
The patient entered surgery with the diagnosis of pseudo-occlusive symptoms secondary to non-rotation type intestinal malrotation syndrome, with urinary infection associated.
Discussion
Malrotation occurs in approximately 1/500 births, with symptomatic cases in only 1/5000 live births, most of which are diagnosed before the first year of life, 75% of them in the neonatal period. When it occurs in newborns, it does so in the first days-weeks and constitutes a clinical-radiological emergency, if it is associated with intestinal volvulus. The presence of bilious vomiting at 5-7 days after birth in a previously healthy child should be attributed to a midgut volvulus until proven otherwise [3].
It is frequently associated with a wide spectrum of congenital anatomical abnormalities and syndromes including omphalocele, gastroschisis, duodenal atresia/stenosis, congenital heart disease, heterotaxis, Marfan syndrome, Meckel syndrome, Cecum motile syndrome, Prune-Belly syndrome, Berdon syndrome, Caudal regression syndrome... [2,3].
Symptomatic cases outside the neonatal period manifest in an anodyne and insidious way, with chronic or recurrent abdominal pain, which delays the diagnosis and, in many cases, is attributed to other entities such as cholecystitis, pancreatitis, pyelonephritis or psychological disorders. If intestinal volvulus is associated, which can appear at any age, it is presented as an obstructive condition with pain, vomiting and a greater or lesser degree of intestinal ischemia [2].
Conventional radiography is not very sensitive and not very specific for the diagnosis of intestinal malrotation since the most common aerial pattern is normal. Even so, it must be performed first to exclude other etiologies and to guide other imaging studies. The right location of the air bubbles in the jejunal frame or the absence of the colonic contour in the right lower quadrant may suggest this. Dilation of the stomach and duodenum with distal air translates an incomplete obstruction, the double bubble a complete obstruction, and pneumatosis and portal gas signs of ischemia.
Gastrointestinal transit is the test of choice to diagnose malrotation, with a sensitivity of 93-100% and a sensitivity of 54% for intestinal volvulus. The location of the duodenum-jejunal junction (Treitz's angle) to the right of the spinal column and below the level of the duodenal bulb is diagnostic.
The opaque enema is currently in disuse and is reserved for cases with doubtful gastroduodenal transit in which it is necessary to demonstrate the anomalous position of the cecum. The position of the cecum is more variable than that of the duodenojejunal junction and can be placed in a normal position in patients with malrotation, so it does not exclude the diagnosis [2,3].
Abdominal ultrasound is less sensitive (67-100%) and specific (75-83%) than duodenal transit to diagnose malrotation, but very useful to detect it early and diagnose its complications, mainly volvulus. The detection of a solid mass representing the airless volvulated loops and the Doppler demonstration of the swirling vessels entering it (vortex sign) is characteristic (sensitivity 92%; specificity 100%). Although there may be an inversion of the situation of the superior mesenteric vein (SMV) and located to the left of the superior mesenteric artery (SMA) or rotating around it, this finding is not pathognomonic and, furthermore, a normal SMA/SMV relationship does not exclude the diagnosis of intestinal malrotation so this finding it must be correlated with the Gastrointestinal transit.
The CT allows to see the abnormal position of the intestinal loops, the SMA/SMV relationship, the swirl sign and the alterations in the perfusion of the loops that can lead to massive ischemia when the turn of the loops occludes the vascular structures. Although it is not a routine study in the diagnosis of malrotation, it is helpful in the diagnosis of this entity in cases where, as in the one presented, it is discovered incidentally [2,3].
Conclusion
Intestinal malrotation can be defined as the failure of normal rotation and fixation of the midgut during fetal development. It is a broad term that includes a wide variety of abnormalities of bowel rotation and fixation.
The clinical picture is very varied, ranging from volvulus and intestinal ischemia to asymptomatic patients.
In adult patients with associated malformations, this entity must be considered in cases of recurrent abdominal pain.
In the case of our patient, who presented with caudal regression syndrome and associated polysplenia and renal malrotation, a detailed history revealed multiple previous episodes of abdominal pain that required an emergency consultation. Imaging tests were not performed in any of them and, given the history of bladder lithiasis, they were labelled as reno-ureteral crisis. In view of the findings described in the CT scan, they were most likely secondary to pseudo-occlusive conditions conditioned by intestinal malrotation.
In the diagnosis, the radiologist plays a fundamental role, especially in the neonatal period in which the existence of an associated intestinal volvulus is an emergency. Gastrointestinal transit continues to be the gold standard for determining the anomalous position of the duodenojejunal junction, but MDCT is very useful for the diagnosis of incidentally discovered malrotations, as in our case.
References
- Berrocal T, Gayá F, de Pablo L (2005) Embryologic, clinical, and radiological aspects of intestinal malrotation. Radiología 47: 237-251.
- Ballesteros GE, Torremadé A, Durán C, et al. (2015) Intestinal malrotation-volvulus: Imaging findings. Radiología 57: 9-21.
- Delgado Carrasco J, Casanova Morcillo A, Marín Rodriguez C El (2010) Vólvulo intestinal: Unaemergencia. De la clínica a la imagen enpediatría. Lo que todoradiólogodebeconocer, 133-140.
- Strouse PJ (2004) Disorders of intestinal rotation and fixation (malrotation). Pediatr Radiol 34: 837-851.
Corresponding Author
Piedad Arias Rodríguez, Radiology Department, University Hospital of Salamanca, Spain
Copyright
© 2020 Rodríguez PA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.