Acute Necrotizing Ulcerative Gingivitis with Tongue Ulcer
Abstract
We describe our experience with a 21-year-old man who presented with acute necrotizing ulcerative gingivitis with tongue ulcer. The patient underwent urgent gingival debridement to excise the necrotic tissue and remove the dental calculus after ampicillin/sulbactam, metronidazole and chlorhexidine oral rinse. Acute necrotizing ulcerative gingivitis is a rare disease with decreased prevalence. Our understanding of acute necrotizing ulcerative gingivitis remains largely limited and further studies should be needed to explore the exact molecular mechanisms.
Keywords
Acute necrotizing ulcerative gingivitis, Tongue ulcer, Urgent gingival debridement
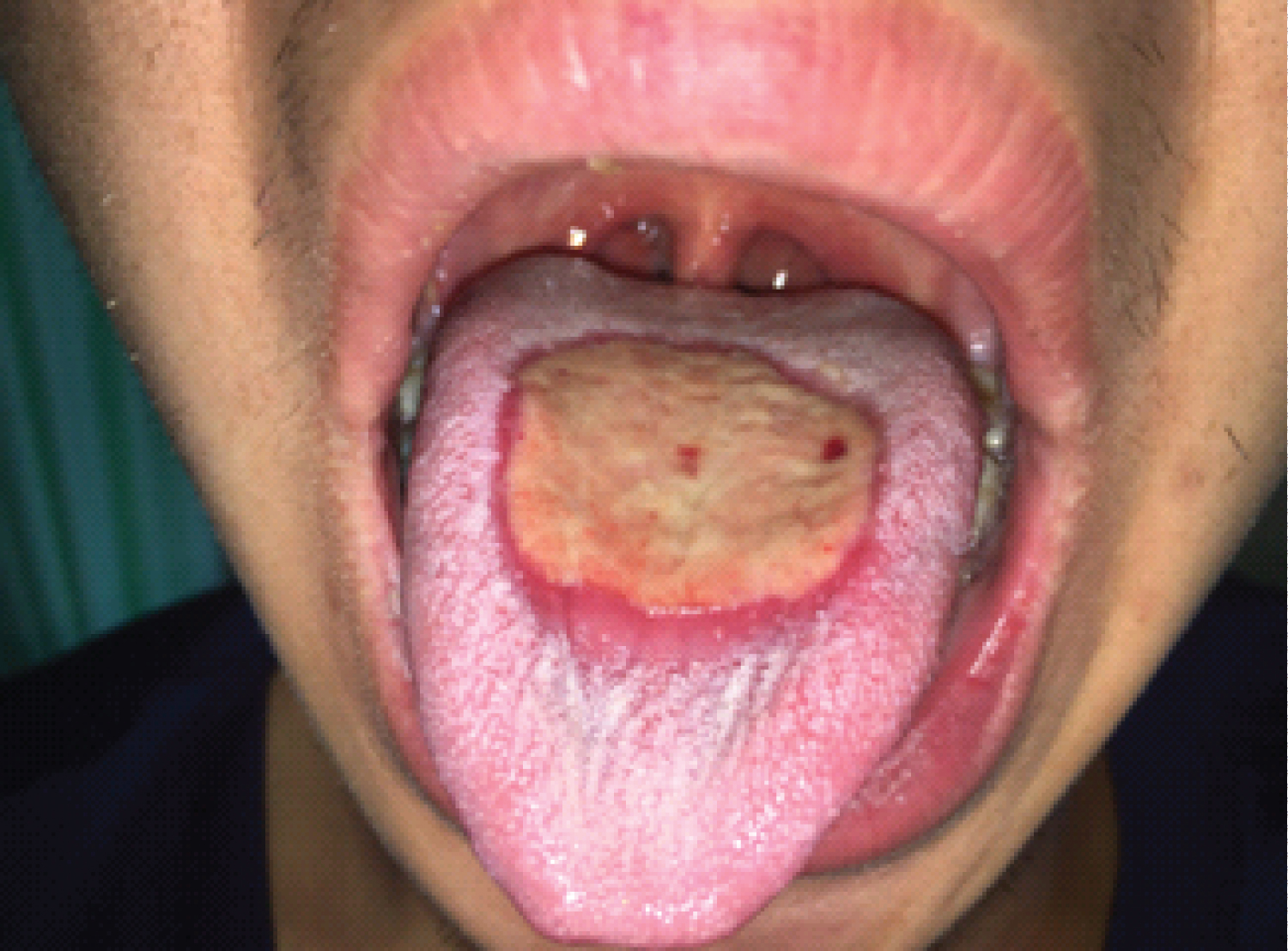
A 21-year-old man presented to the emergency department with a 6-hour history of vomiting, epigastric pain and diarrhea after uncooked seafood consumption. He had no documented medical history. Physical examination revealed normal vital signs and mild epigastric tenderness with hypoactive bowel sounds. The rest of the physical exam was unremarkable. Valuable clues were not found by computed tomography of the abdomen and gastroscopy. Laboratory tests of the blood confirmed a white-cell count of 21,300 per cubic millimeter (reference range, 4000 to 10,000). 3 days after admission, he suffered progressive pharyngalgia and pain of gingival surfaces associated with a soaring temperature and endless drooling of saliva. A physical examination revealed tonsil hypertrophy, pharyngeal edema, dental calculus, and inflammation and necrosis of the lower and upper gingiva with huge tongue ulcer (Figure 1, Figure 2 and Figure 3). Neck and submandibular lymph nodes were not palpable. Direct saliva microbiologic detection and blood cultures were negative for the human immunodeficiency virus, bacterial and fungal pathogens. The patient received a diagnosis of acute necrotizing ulcerative gingivitis (ANUG) with tongue ulcer due to the severe inflammation spread widely from the throat to the soft palate associated with severe gingivitis of both upper and lower gingiva. Further questioning of the patient found that he had never brushed his teeth and denied cigarette smoking, illicit drugs and unsafe sex practices. ANUG is a type of periodontal disease characterized by pain, necrosis, ulceration, and bleeding in gingival surfaces, appeared at much lower rates in the general population, which can cause progressive destruction of the gingivae [1-5]. ANUG is often caused by periodontopathic bacteria, mainly spirochetes and oral anaerobes, which may eventually result in cancrum or is if left untreated, a severe form with gangrenous orofacial lesions [6-10]. Empiric antibiotics were changed to ampicillin/sulbactam, metronidazole and chlorhexidine oral rinse on day three of hospitalisation. The patient underwent urgent gingival debridement to excise the necrotic tissue and remove the dental calculus. Since he received ampicillin/sulbactam and metronidazole for a total of 7 days without side effects and oral manifestations improved, the patient denied gingival pain and was discharged home on chlorhexidine oral rinse.
Acknowledgements
Funding
This work was supported by National Natural Science Foundation of China (31600134).
Conflicts of Interest
The authors have no conflicts of interest to declare.
Ethical Statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this "letter".
References
- Hu J, Kent P, Lennon JM, et al. (2015) Acute necrotising ulcerative gingivitis in an immunocompromised young adult. BMJ Case Rep.
- Folayan MO (2004) The epidemiology, etiology, and pathophysiology of acute necrotizing ulcerative gingivitis associated with malnutrition. J Contemp Dent Pract 5: 28-41.
- Kato H, Imamura A (2017) Unexpected acute necrotizing ulcerative gingivitis in a well-controlled hiv-infected case. Intern Med 56: 2223-2227.
- Melnick SL, Roseman JM, Engel D, et al. (1988) Epidemiology of acute necrotizing ulcerative gingivitis. Epidemiol Rev 10: 191-211.
- Rowland RW (1999) Necrotizing ulcerative gingivitis. Ann Periodontol 4: 65-73.
- Bolivar I, Whiteson K, Stadelmann B, et al. (2012) Bacterial diversity in oral samples of children in niger with acute noma, acute necrotizing gingivitis, and healthy controls. PLoS Negl Trop Dis 6: e1556.
- Dufty J, Gkranias N, Donos N (2017) Necrotising ulcerative gingivitis: A literature review. Oral Health Prev Dent 15: 321-327.
- Wade DN, Kerns DG (1998) Acute necrotizing ulcerative gingivitis-periodontitis: A literature review. Mil Med 163: 337-342.
- Johnson BD, Engel D (1986) Acute necrotizing ulcerative gingivitis. A review of diagnosis, etiology and treatment. J Periodontol 57: 141-150.
- Lopez R, Fernandez O, Jara G, et al. (2002) Epidemiology of necrotizing ulcerative gingival lesions in adolescents. J Periodontal Res 37: 439-444.
Corresponding Author
Wei Liu, Ph.D., Institute of Digestive Disease, China Three Gorges University, 8 Daxue Road, Yichang 443000, China.
Copyright
© 2020 Ai-Chao S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.