Colon Mass and Liver Lesions: What Else Could it be?
Abstract
Background
Choriocarcinoma is a rare malignant tumor of trophoblastic cells that usually occurs after molar and non-molar pregnancies. It most commonly arises in the placenta, but other primary sites have been described. Metastatic disease occurs in ~30% of cases given the aggressive nature of the choriocarcinoma.
Patient/Results
Although metastatic lesions to the gastrointestinal tract have been reported, there have not been previous reports of primary uterine choriocarcinoma directly extending to and invading the colon. We report a case of a uterine choriocarcinoma with direct colonic invasion mimicking a primary colonic adenocarcinoma with liver metastases.
Conclusion
Choriocarcinoma should always be on the differential diagnosis of colon masses, especially in younger patients who present with gynecologic complaints.
Keywords
Choriocarcinoma, Colon mass, Liver metastases
Introduction
Choriocarcinoma is a rare malignant tumor of trophoblastic cells that usually arises in the placenta. It is characterized by early vascular invasion and widespread metastasis. Hematogenous spread has been reported in a large extent to the lungs (75%) and vagina (50%) and to a lesser extent to the ovaries, brain, bowel and ureters [1,2]. Metastases to the liver are relatively uncommon affecting only 10% of patients. Histologically, choriocarcinoma is among the most aggressive of the gestational trophoblastic neoplasia. Macroscopically, it is highly vascular and it usually invades adjacent structures at the time of diagnosis. Less commonly, non-gestational choriocarcinoma have been reported [3]. Theses can arise in the ovaries or uterus in females, the testes in males, or have a primary extra-gonadal choriocarcinoma [3]. In this case report, we report an unusual diagnosis of a non-gestational uterine choriocarcinoma presenting as a colonic mass due to direct external invasion into the colon with liver metastases.
Patient Report
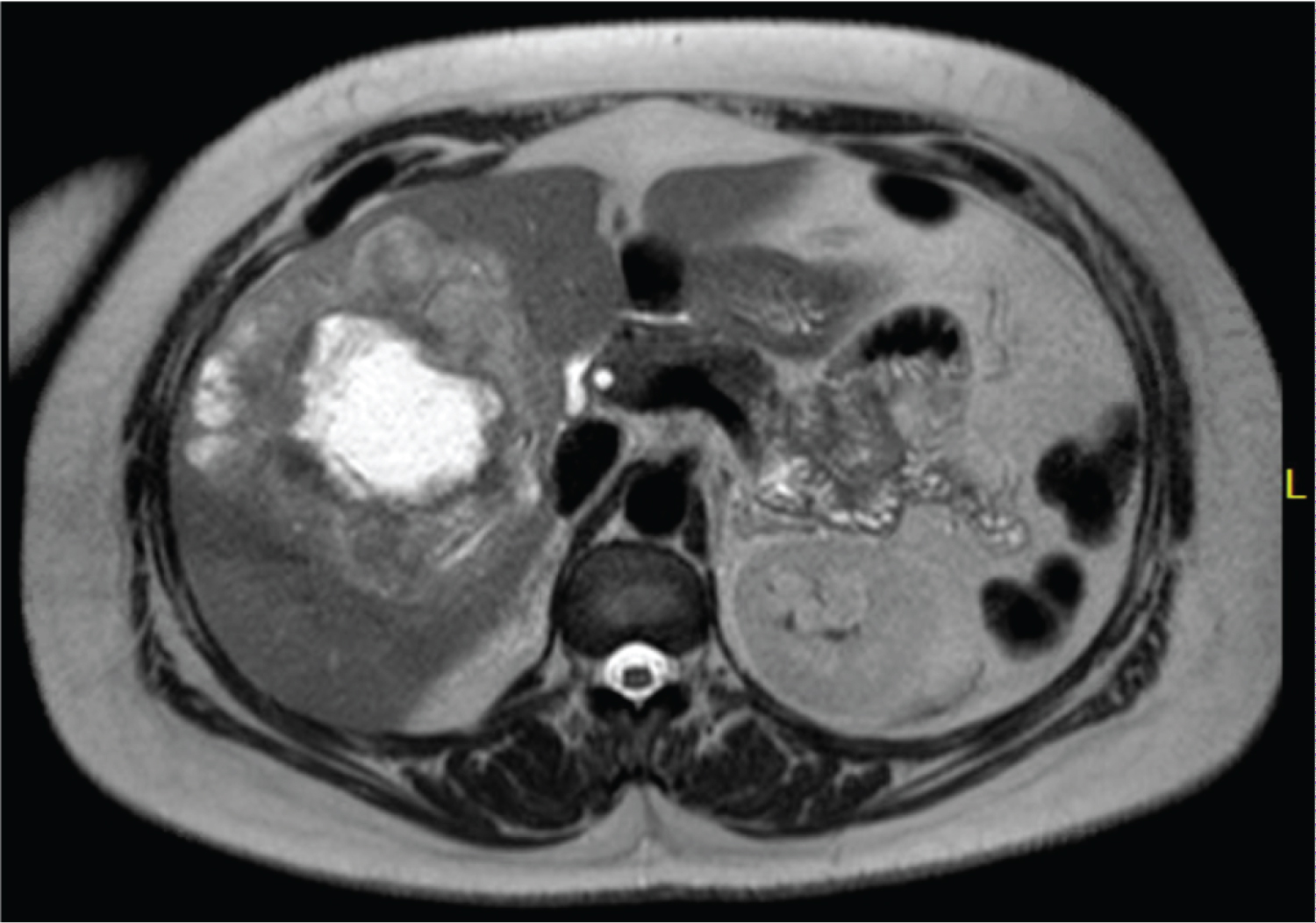
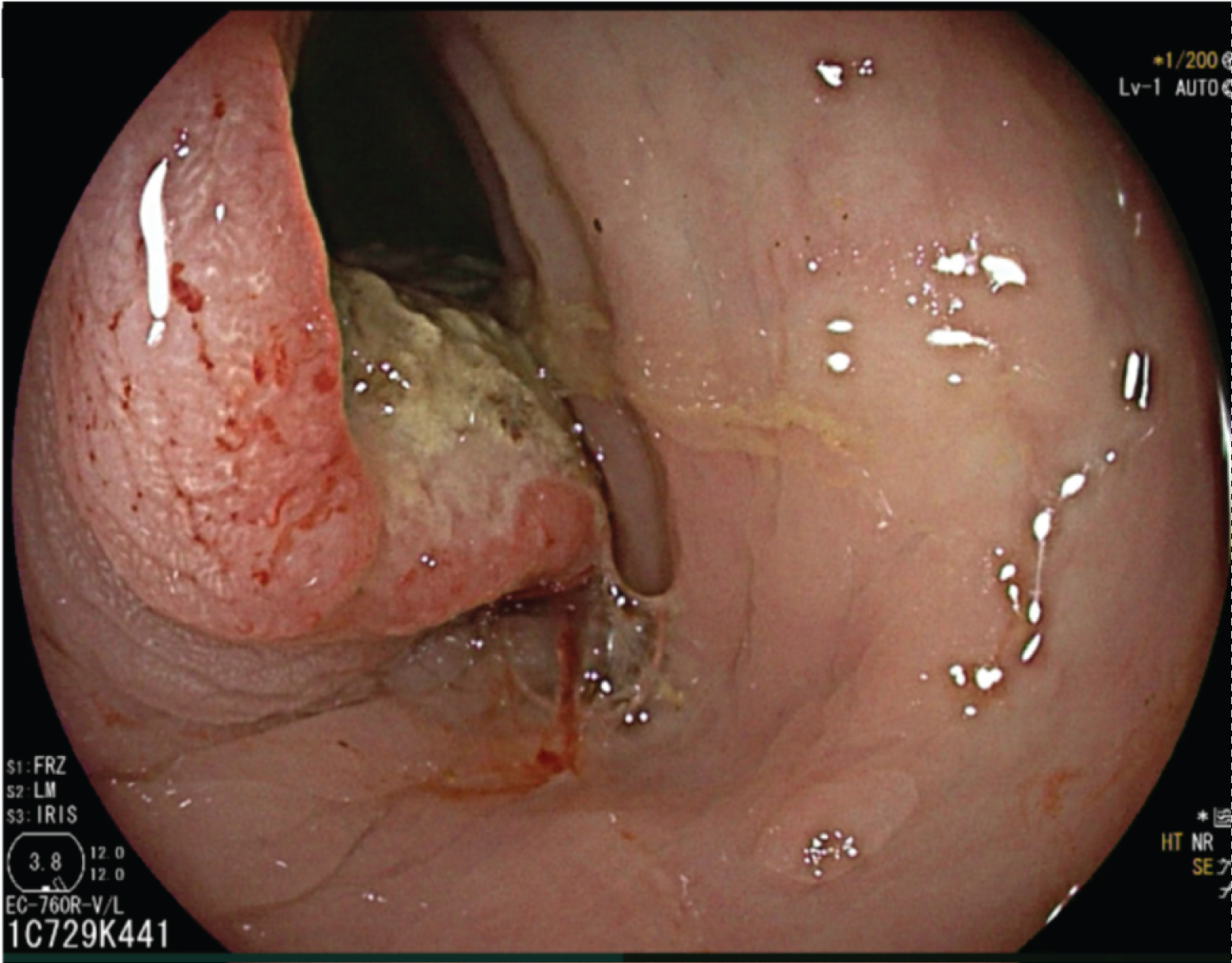
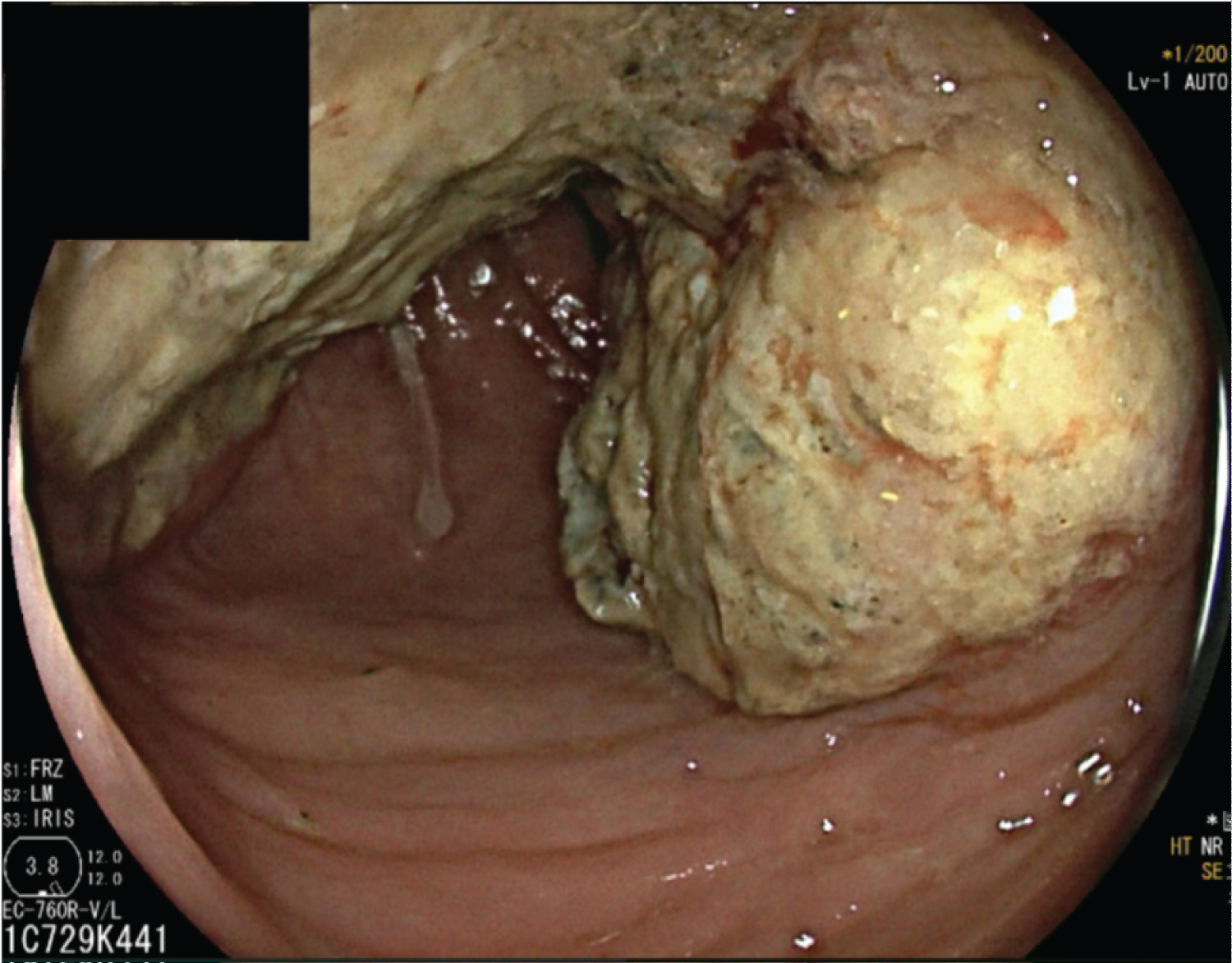
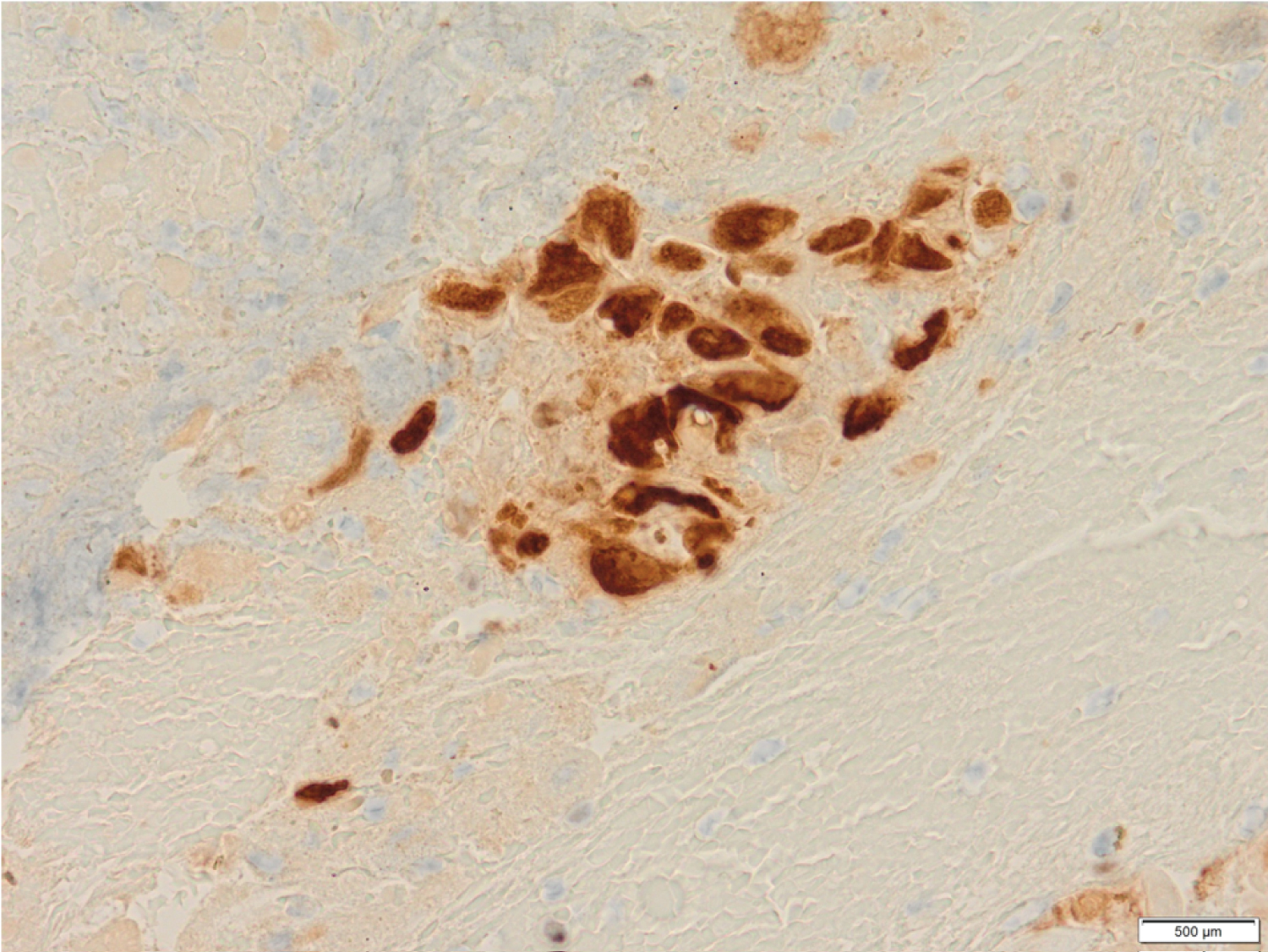
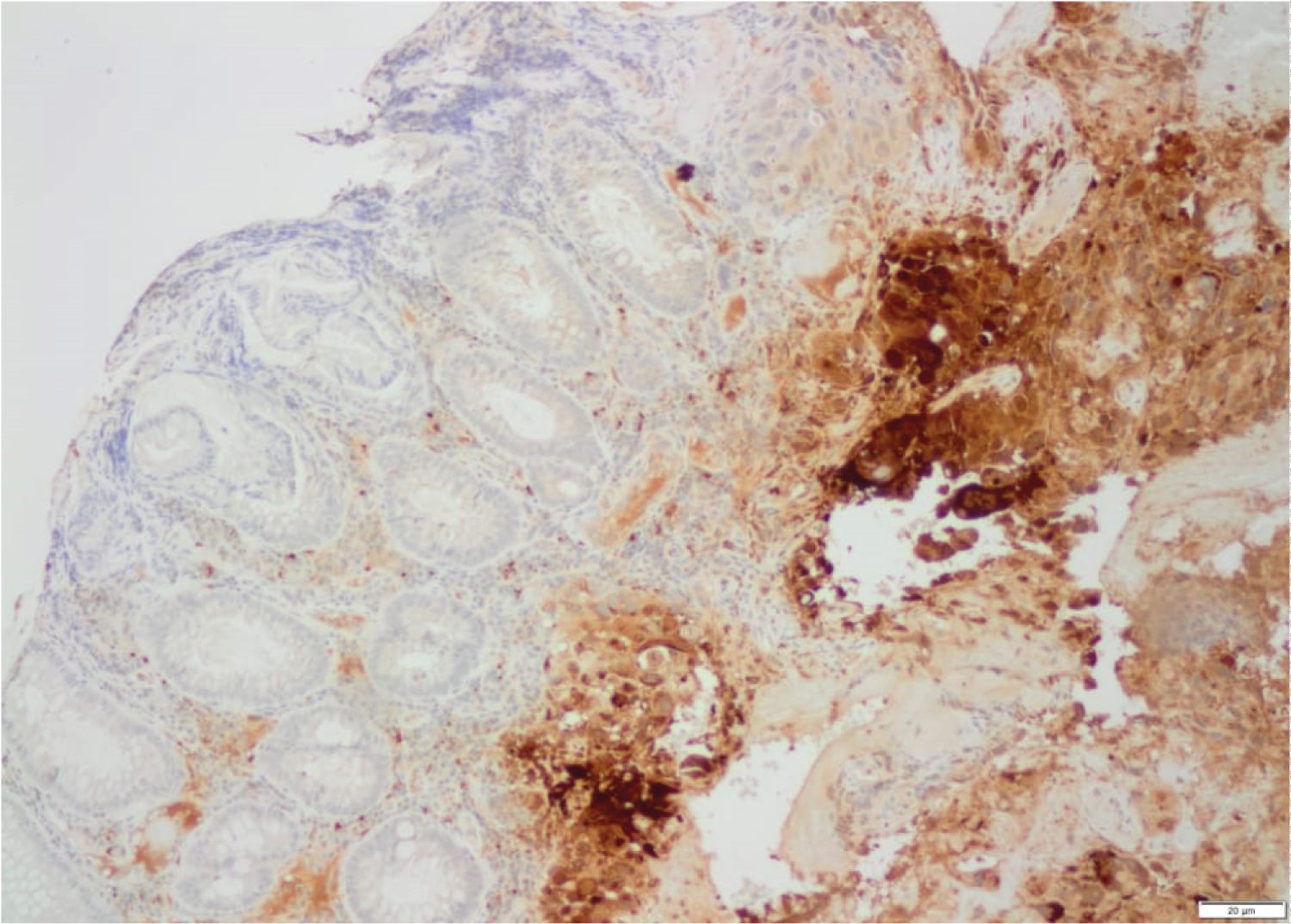
A 42-year-old healthy female, G2P2, underwent an abdominopelvic ultrasound for evaluation of a 3-month history of menorrhagia. Multiple large liver lesions were found, so an abdominal MRI was performed which revealed many large centrally necrotic lesions, largest measuring 10.5 × 11.5 cm, highly suspicious for metastases (Figure 1). The patient also had enlarged retroperitoneal lymph nodes. There was also a 6 cm mid-sigmoid mass extending into the peri-colonic fat with surrounding lymphadenopathy. The tumor was closely related to the cervix and left ovary. The patient denied change in bowel habits and continued to have formed bowel movements once every 2 days without any rectal bleeding. On physical examination, the patient's abdomen was soft, nondistended, mildly tender in the left lower quadrant, with no palpable masses. Blood work showed a hemoglobin of 9.4 g/dL, MCV 74 fl, and platelet count of 581,000/cu.mm. CEA, CA-125, and CA 19-9 levels were all normal. A colonoscopy showed a semi-circumferential pale appearing necrotic mass extending from 18 cm to 24 cm from the anal verge (Figure 2 and Figure 3). The shiny and smooth endoscopic appearance of this mass was not typical of a primary colonic adenocarcinoma. The mass was very hard on biopsies and revealed invasive poorly differentiated carcinoma. P16 and CK5/6 immunostains were negative excluding a primary colonic malignancy. The tumor cells were diffusely and strongly positive for GATA-3 staining as shown in Figure 4 [4].
Although our patient's initial radiographic images suggested a primary colon malignancy, given the atypical histologic staining of this young female patient, a choriocarcinoma had to be excluded. Serum beta-human chorionic gonadotropin (b-HCG) was checked and was elevated at 51,522 mIU/mL. Also, HCG staining on the tumor was positive confirming the diagnosis of a choriocarcinoma (Figure 5). Whole body PET/CT was consistent with above findings, and MRI brain was negative for metastases. On dedicated pelvic exam and imaging, our patient was found to have an enlarged uterus with an apparent necrotic mass that was causing abnormal uterine bleeding, indicating that the choriocarcinoma was originating from the uterus and directly invading the sigmoid colon.
Shortly after diagnosis, the patient traveled to seek a second opinion and underwent a repeat colonoscopy with biopsies, after which she developed severe left lower quadrant abdominal pain and fever. She then returned to our institution (a month after initial presentation) and evaluation showed a contained perforation of the colon at the level of the sigmoid mass with adjacent loculated collections containing fluid and gas. The patient underwent laparoscopic drainage of the pelvic abscess with a laparoscopic left end colostomy. Given the high tumor load with WHO score of 19, she was started on low-dose induction chemotherapy with cisplatin and etoposide (EP) with a plan to switch to EMACO (Etoposide, Methotrexate, Actinomycin-D, Cyclophosphamide and Vincristin). Given the excellent response to treatment, she was continued on the same regimen until normalization of b-HCG. She then received 3 more maintenance cycles beyond normal b-HCG, with a total of 16 cycles over 5 months. One month after completion of chemotherapy, b-HCG was 1.4, however PET/CT and MRI showed a new suspicious liver lesion with resolution of all previous metastases. Biopsy of the new lesion was consistent with the initial pathology. Options of surgery verses chemotherapy were discussed, and after multidisciplinary consultation, the decision was to repeat serial imaging a one month later to assess the evolution of disease. Repeat PET revealed progression of disease with hilar, hepatic, retroperitoneal and peritoneal metastases, and a rise in b-HCG to 16. After consultation with international experts, the patient was started on a new regimen of chemotherapy (Paclitaxel, Ifosfamide and Cisplatin).
Discussion
Abnormal uterine bleeding or amenorrhea, are among the usual symptoms of gestational and non-gestational trophoblastic neoplasia which was the case in our patient. However, the absence of uterine abnormalities on pelvic US and the incidental appearance of liver lesions and a mid-sigmoid mass on the initial imaging shifted the working diagnosis to the more common primary colonic adenocarcinoma with liver metastases.
The unusual endoscopic appearance of a pale appearing shiny necrotic mass with negative stains for a gastrointestinal malignancy as well as the high tissue and serum HCG confirmed the diagnosis of primary uterine choriocarcinoma with invasion of the sigmoid colon. To date, there have not been any reported cases of such an atypical presentation of a uterine choriocarcinoma invading the colon and mimicking a primary colon adenocarcinoma. Primary choriocarcinoma of the sigmoid colon as well as metastatic choriocarcionoma to the small bowel have been reported [2,5]. Staging of choriocarcinoma depends on local invasion as well as distant metastasis. Low risk trophoblastic neoplasias are treated with single agent chemotherapy while high risk neoplasias are treated with multi-agent chemotherapy EMACO. However, choriocarcinomas of ovarian origin tend to be more chemo-resistant as compared to their gestational counterparts. Hysterectomy is indicated in the case of uncontrolled uterine bleeding [6]. Our patient had a WHO score of 19 based on the following: Age, 42: 1; Antecedent pregnancy, term: 2; Interval, > 12 months: 4; Pretreatment serum b-HCG, 51,522: 2; Largest tumor, > 5 cm: 2; Metastases, to liver: 4; Number of metastases, > 8: 4; Prior chemotherapy, none: 0. Due to the high tumor load and WHO score of 19, she was given low-dose induction chemotherapy to decrease the risk of massive tumor lysis and mortality. Unfortunately, she was at high risk for recurrence and recurred shortly after completion of first-line chemotherapy.
Sources of Funding
None.
Conflict of Interest
No conflict of interest exists.
Author's Contributions
S Jabak: Acquisition of data; analysis and interpretation of data; drafting of the manuscript.
R Abdallah: Acquisition of data and interpretation of data.
FF Francis: Critical review of the manuscript.
HM Kfoury: Acquisition of data.
JG Hashash: Study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; and critical review of the manuscript.
References
- Hillard AE, RW Allen, G Beale (1993) Metastatic choriocarcinoma: Correlation of MRI, CT, and angiography. South Med J 86: 1299-1302.
- Arencibia PB, RE Gómez, GJ Marchena (2020) Metastatic choriocarcinoma in the proximal jejunum, an exceptional cause of massive upper gastrointestinal bleeding. Rev Esp Enferm Dig 112: 327-328.
- Andrea Ronchi, Immacolata Cozzolino, Marco Montella, et al. (2019) Extragonadal germ cell tumors: Not just a matter of location. A review about clinical, molecular and pathological features. Cancer Med 8: 6832-6840.
- Mirkovic J, Elias K, Drapkin R, et al. (2015) GATA3 expression in gestational trophoblastic tissues and tumours. Histopathology 67: 636-644.
- Hiromitsu Maehira, Tomoharu Shimizu, Hiromichi Sonoda, et al. (2013) A rare case of primary choriocarcinoma in the sigmoid colon. World J Gastroenterol 19: 6683-6688.
- Hextan YS Ngan, Michael J Seckl, Ross S Berkowitz, et al. (2015) Update on the diagnosis and management of gestational trophoblastic disease. Int J Gynaecol Obstet 131: S123-S126.
Corresponding Author
Jana G Hashash, MD, MSc, Assistant Professor of Medicine, Division of Gastroenterology, American University of Beirut, Lebanon, Tel: +961-1-374374; Fax: +961-1-365612.
Copyright
© 2020 Jabak S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.