Disruption and Rapid Recovery of Emergency Ophthalmic Services Amidst the COVID Pandemic: An English Teaching Hospital Experience
Abstract
Purpose
To share our experience of emergency ophthalmic services at a major Tier 2 emergency department in the UK National Health Service, including; emergency department attendances in eye casualty, urgent intravitreal injection services and emergency ophthalmic surgery during the COVID pandemic. We also share our experience of urgent cataract and adnexal surgery work during and after the easing of COVID pandemic restrictions.
Methods
Using electronic patient records (EPR) we analysed data for emergency eye clinic attendances and surgical work over a 12 week period during the COVID pandemic from March until May 2020. Emergency surgical work and emergency eye clinic attendance numbers, including type of diagnoses seen were analysed and compared to pre-COVID months. Furthermore, we analysed the data after gradual resumption of routine elective cataract and adnexal surgery from June 2020 onwards.
Results
A 73% reduction in patient attendances in the emergency eye clinic and six-fold reduction in surgical work in comparison to the previous year was observed during the height of the pandemic. Our recovery phase elective surgical work demonstrates a 55% and 62% reduction in cataract and adnexal surgical volume respectively, in comparison to pre-COVID numbers.
Conclusion
At the height of the COVID pandemic we witnessed a significant drop in emergency eye attendances and a complete cessation of elective eye surgery. Investment in Telephone Triage allowed > 70% of emergency patients to be managed without attendance to hospital. It was safe to restart urgent surgery almost immediately after lockdown finished.
Introduction
The COVID-19 pandemic has mandated an unprecedented overhaul of healthcare service provision in the United Kingdom and worldwide. In response to guidance issued by the Royal College of Ophthalmologists (RCOphth) [1] as well as the American Academy of Ophthalmology in March 2020, Southampton Hospital Eye Unit began to suspend elective and non-urgent surgery and outpatient appointments from mid-March 2020. Our eye department normally sees 90,000 patient visits a year and this includes all elective and emergency surgery and outpatient visits [2]. Some reports in the literature have provided information on early responses to COVID-19 by emergency eye services [3], and our hospital emergency eye service (HEES), which sees 26,000 patients a year has remained open and we continue to see patients, albeit with challenges and service adjustments tailored to the pandemic. This paper goes further than previous studies and looks additionally at the recovery phase from the COVID-19 pandemic. The strategy of the Unit, a major regional emergency eye department, was also to resume urgent intraocular surgery, which to our knowledge, has not been reported so early in the literature and is relevant in anticipation of further COVID-19 waves and other pandemics. The purpose of our paper is two-fold: First; to highlight the initial impact the of the COVID pandemic on HEES and urgent intraocular and urgent adnexal surgery in a large teaching hospital from March 2020 and second; to demonstrate the earliest reported recovery in the literature of urgent ophthalmic surgical work as early as 1st June 2020. Social lockdown measures in the United Kingdom came into effect on the 23rd March 2020.
Impact of Pandemic on HEES
Reasons for increased pressure on the UK National Health Service (NHS) during this time have included i) An anticipated surge in walk-in and referred emergency patients - due in part to closure of community optometric practices enrolled with the Southampton Minor Eye Conditions Service (MECS), as well as an initial limited general practitioner (GP) service; ii) Re-deployment of key frontline staff away from ophthalmology to other specialties; iii) Pressure from patients whose routine hospital eye appointments have been postponed owing to COVID and who have clinically seriously deteriorated. MECS was the local version of other nationwide schemes but for the South-East NHS Region - it offers patients an alternative to attending the HEES and also includes some general practices (GPs) [4] with 6 optometric practices and 27 GPs enrolled with the scheme [5]. The MECS scheme was replaced by the COVID-19 Urgent Eye Service (CUES) based in the community which started in June 2020, going fully live in July 2020 [6]. The CUES scheme supported our HEES by having a nationally-linked trained group of optometrists see less serious urgent conditions including even anterior uveitis, preseptal cellulitis and microbial keratitis - supported by independently prescribing opticians who were networked on a national level within England.
In terms of HEES staffing, the COVID pandemic provisions were shaped at this university teaching hospital by the presence of a relatively large number of junior doctors in ophthalmology training posts - in anticipation of the pandemic these doctors were prepared for re-deployment to hospital wards, the main emergency department and intensive care, leaving only consultant ophthalmologists to deliver eye services. There was a significant reduction in staff due to shielding or sickness and due to a significant portion of nursing staff having been redeployed to other departments within the hospital. This has affected triage and led to loss of nurse practitioners from HEES.
In addition patient flow pathways were adjusted into COVID positive and negative areas as in many hospitals, but with the Eye Casualty suite temporarily vacated to allow physical distancing of elderly patients undergoing intravitreal injections in the adjacent intravitreal suite as the waiting rooms were shared. A number of emergency kits were distributed into key areas with slit lamps in the hospital e.g. for intravitreal injections (for endophthalmitis) and lateral canthotomy (for oculoplastic/orbital emergencies), and emergency eye care pathways clarified for consultants. However, the eventual pandemic was not as severe as had been prepared for, so at the 11th hour the department retained its junior medical staff. We have had to cope with the restrictions in terms of physical space, HEES being moved temporarily into paediatric eye clinics.
Measures Taken to Help Reduce Spread of the Virus
In order to reduce the spread of the pandemic we have had to make adjustments to our HEES at the door triage. All patients are asked to clean their hands with alcohol gel on arrival and asked to wear a surgical mask to cover the mouth and nose. Patients are asked screening questions and have their body temperature recorded. Any patients suspected of having COVID are redirected to an isolated area in the hospital for further assessment. Those subsequently found to be infected with COVID are examined and managed in a separate 'hot' area of the hospital. Patients with no suspicion of COVID infection were either seen on arrival or allocated an appointment in the HEES clinic at a later date depending on urgency. This was in order to minimise the number of patients in the department and adhere to social distancing rules. All staff with patient face to face interaction were required to undergo 'fit testing' for personal protective equipment (PPE) face masks. Doctors and other staff who were seeing patients were provided with face masks, disposable gloves and aprons, and protective eye goggles. Slit lamps were fitted with protective plastic shields to prevent droplet transmission. These protective measures are similar to what other units have reported [7-10].
Additionally, we invested heavily in a telephone consultation service for patients with urgent eye conditions to avoid unnecessary attendance to hospital. A pre-existing telephone triage service was bolstered with two full time staff (specialist nurses) to handle incoming calls. There were an average of 44 telephone calls a day and an average of 23 clinical 'call backs' a day. Investment in Telephone Triage allowed > 70% of emergency patients to be managed without attendance to hospital. This was supported by re-deploying staff to this key area. This necessitated adjustments to the Patient Electronic Patient Record (EPR) (Symphony) and support by doctors, aided by in a small number of cases video-conferencing in common with other units. Video consultation was found to be useful for external diseases in computer-literate patients. Anecdotally, we found telephone consultation was faster and easier to use, especially in elderly patients and most cases regardless of age group could be managed with it. Photos sent by patients to a secure Trust email address often equally sufficed for video consults.
We acknowledge there are validated triage tools for ophthalmic emergencies in the literature such as the Alphabetical Triage Score for Ophthalmology (ATSO) [11] or the Rome Eye Scoring System for Urgency and Emergency (RESCUE) [12], which have been found to be accurate and useful for risk stratification of ophthalmic emergencies. In our case staff performing triage adhered to locally drafted hospital protocols.
Initially all elective surgery was cancelled except for patients in urgent cancer pathways.
Emergency Eye Clinic Attendances during the COVID Pandemic
Using our electronic medical records, we analysed 12 weeks of data from our HEES attendances beginning from the 16th of March 2020 (Table 1). This corresponds to the week we began to cease all elective and non-urgent clinical and surgical work (lockdown). We observed that weekly HEES attendances gradually declined for the first four weeks of the lockdown and began to steadily rise from mid-April onwards. Comparison is made with the corresponding weeks from the previous year, which at one point in early April showed a 73% reduction in attendances compared with the same time the previous year.
In the 12 weeks we analysed during the pandemic, the HEES observed 3427 attendances and telephone consultations in total. In the corresponding period from the preceding year, the HEES received 6826 patient visits and telephone consultations in total.
The most commonly recorded diagnoses for HEES attendances are recorded in Table 2, as well as the corresponding diagnoses for the previous year. In comparison to the previous year, during the pandemic the percentage of patients seen with less serious conditions in eye casualty such as conjunctivitis and blepharitis fell by 5.9% and 2.4% respectively.
The increase in vitreoretinal emergencies (such as retinal detachments) that was anticipated but not realised, by some tertiary hospitals due to satellite unit closures [3], was not seen in our unit. This is most likely due to our neighbouring units continuing emergency surgical work. Forty-two cases of retinal detachment attended the HEES in the 12 weeks of lockdown, in comparison to 54 cases in the preceding year, a 22% reduction.
Surgical Work during the COVID Pandemic
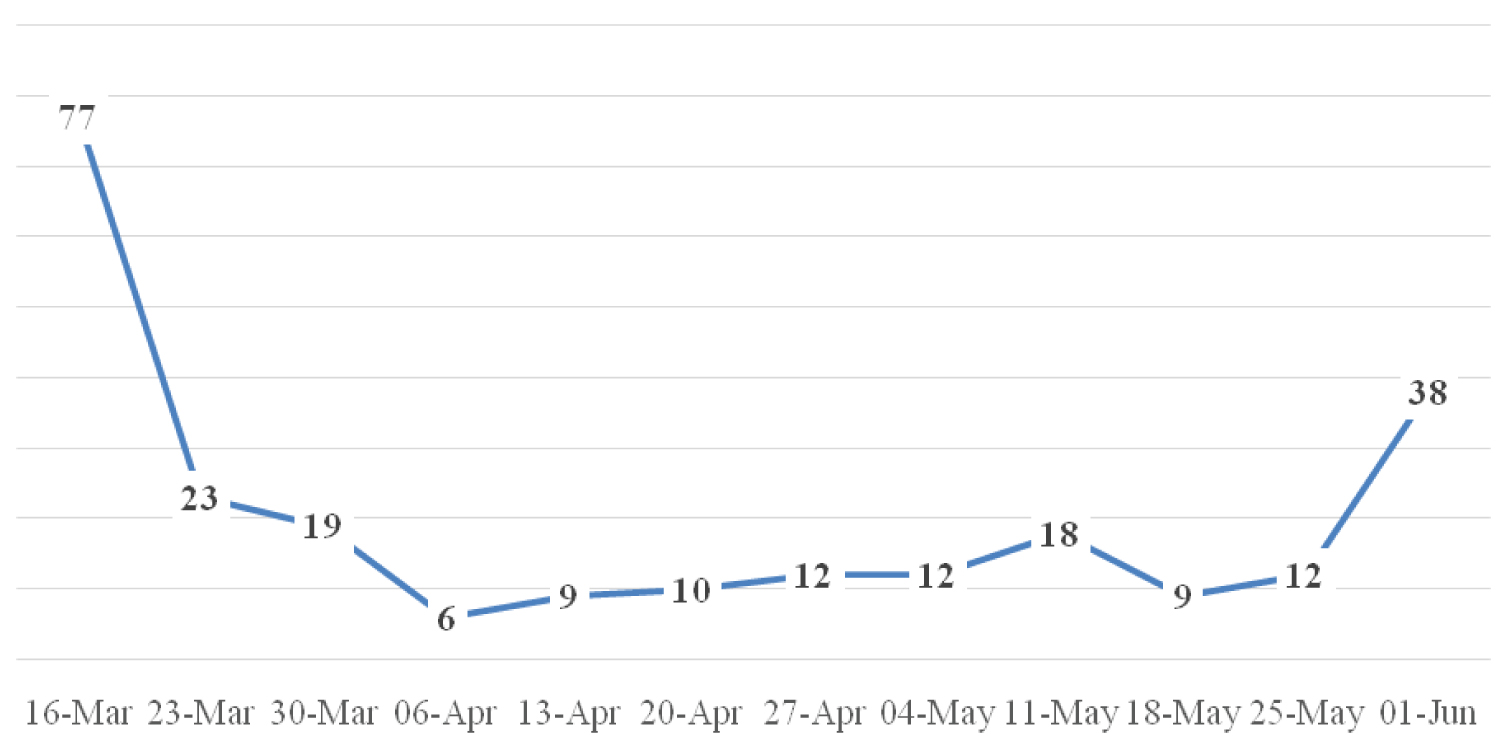
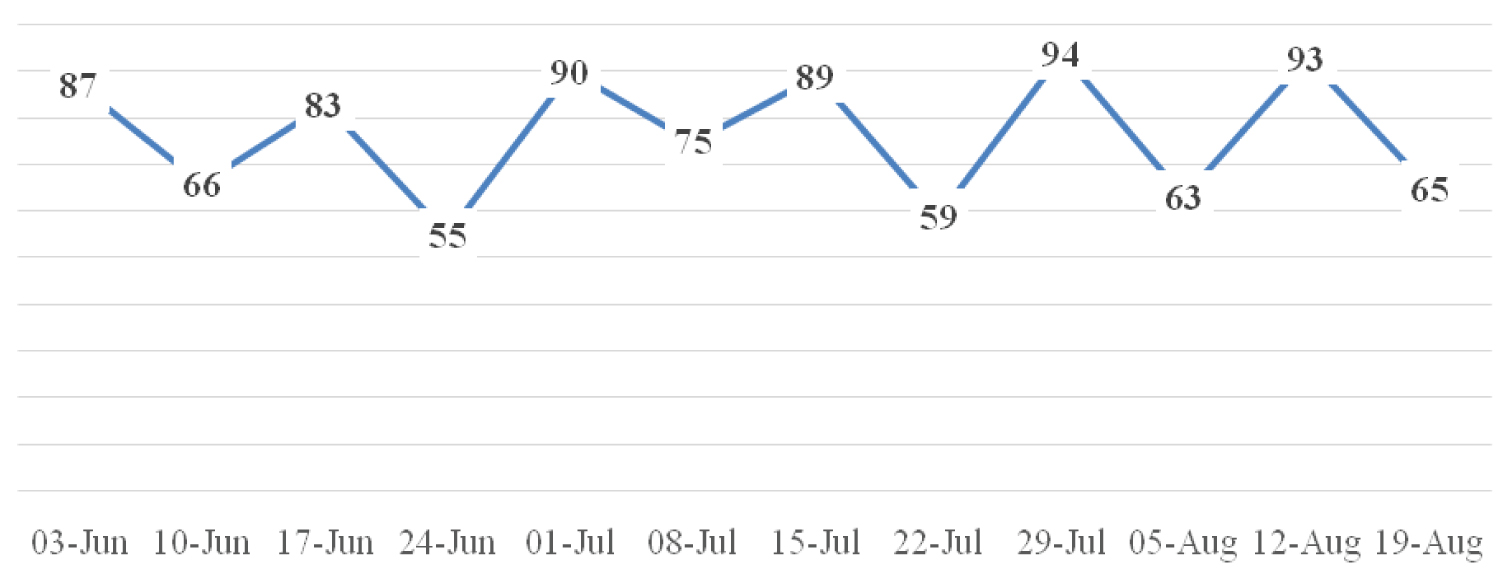
In total 168 emergency/urgent operations took place in the 12 weeks of reduced surgical work we analysed. A week by week breakdown of numbers is shown in Figure 1. Of these, 53% were vitreoretinal procedures mainly for retinal detachment surgery, a sight-threatening emergency. The remaining operations included urgent trabeculectomy or minimally invasive glaucoma surgery combined with or without phacoemulsification intraocular lens insertion [13], urgent eyelid lesion or tumour biopsy with or without reconstruction [5], corneal gluing for perforated eyeballs [4], globe rupture or eyelid/lacrimal system trauma repair [4], paediatric cataract where amblyopia (permanent sight loss) is a major risk [1]. In comparison, 1035 operations were performed in the same 12 weeks in 2019, which represents a six-fold reduction in surgical output.
Anti-VEGF (Vascular Endothelial Growth Factor) Treatment
Intravitreal treatment with anti-VEGF injections has continued in our unit but initially only for urgent cases with serious risk of acute sight loss from severe macular disease, and in comparison to last year the number of injections seemed to drop off significantly especially at the peak of the pandemic lockdown. The week by week number of patients treated with anti-VEGF injections, both during the pandemic and the corresponding period from last year, are demonstrated in Table 3. It demonstrates a 48% reduction in injection treatment at the height of the pandemic, albeit the reduction seemed to tail off towards the end of the 12 week period, due to an increase in service provision as the lockdown measures started to ease. Where reasonably possible patients were placed on a longer-acting anti-VEGF agent aflibercept (Eylea) to reduce injection frequency.
Recovery Phase
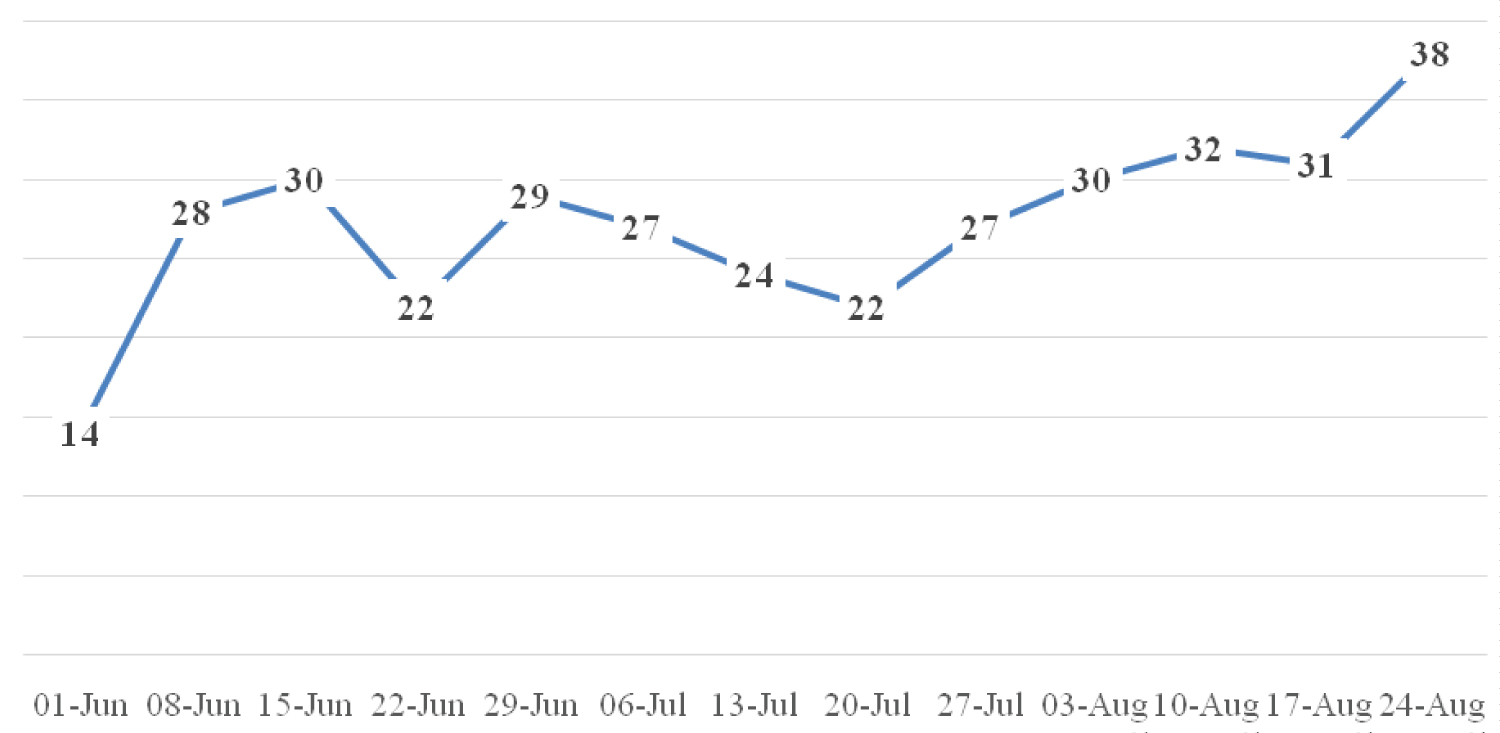
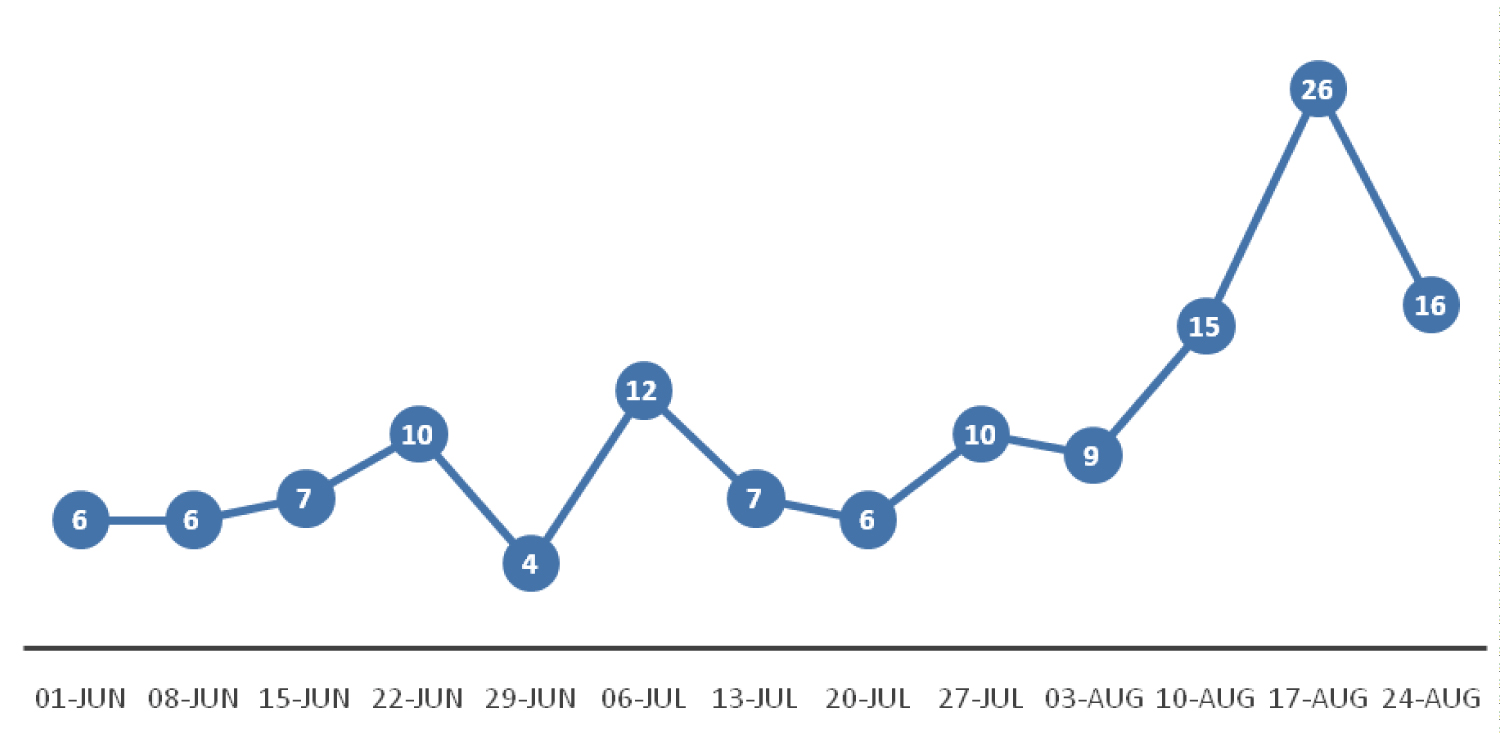
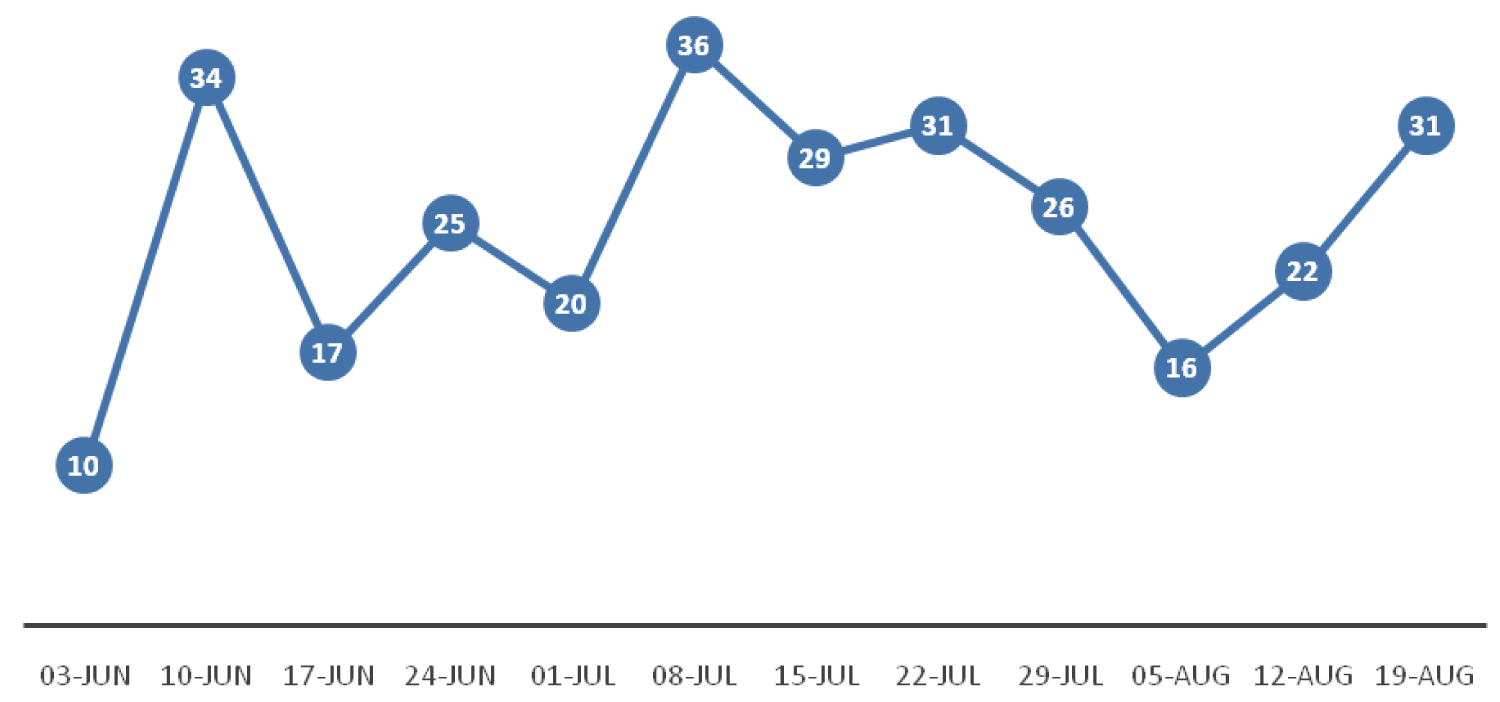
From June 1st 2020, the ophthalmology department at University Hospital Southampton recommenced urgent cataract and urgent adnexal surgery in a gradual fashion. Patients were triaged, often electronically, choosing the most severe cases or where there was risk of permanent sight loss or loss to life for adnexal cases including cancers such as those with intracranial involvement. Figure 2 and Figure 3 illustrate the weekly number of cataract and adnexal operations performed respectively. All patients undergoing surgery must demonstrate a negative COVID PCR test prior to surgery and were instructed to isolate at home for two weeks prior to their surgery.
The weekly number of patients seen in the HEES from June 2020 onwards is demonstrated in Table 4. It demonstrates a significant increase in attendances compared to the 12 weeks of HEES attendances during the pandemic demonstrated in Table 1. It also shows a gradual increase in patient attendances week by week. This increase in numbers corresponds with the easing of nationwide lockdown measures. It remains to be seen if subsequent social lockdowns will correspond with reductions in patient attendances.
The recovery phase however still shows a significant reduction in surgical activity in comparison to the previous year. The week by week numbers of cataract and adnexal surgery from the preceding year are shown in Figure 4 and Figure 5 respectively. During the initial 12 weeks of recovery there was still a 55% and 62% reduction in adnexal and cataract surgery respectively, in comparison to the previous year.
Conclusion
The impact of the COVID pandemic on ophthalmic healthcare is multifaceted. The primary concern is that patients will come to harm due to delayed presentation to the HEES. To date we have not seen evidence of significant delayed presentation of eye pathology. Many patients with emergency ophthalmology conditions are in groups vulnerable for COVID-19, including the elderly many of whom have been reluctant to attend the emergency eye department. Provision of a large telephone triage service, providing over the phone advice was crucial in providing support for all groups especially the elderly, with limited additional benefit from video consultation outside of acute external diseases where photographs also sufficed. Investment in Telephone Triage allowed > 70% of emergency patients to be managed without attendance to hospital. It was safe to restart urgent surgery almost immediately after lockdown finished.
COVID-19 infection rates are once again accelerating in the UK [13] and the UK government has warned of local and possible repeat national lockdowns. The data in this paper shows a successful strategy to cope with further lockdowns (including for other similar pandemics) and how urgent surgery can be restarted very early after lockdown. No patients suffered harm by restarting surgery so quickly immediately after lockdown - no patients or eye department staff caught COVID-19. Restarting urgent surgery early reduces the large waiting times COVID-19 has created for serious disease in which patients can go may become irreversibly sight impaired or lose life in case of aggressive malignant disease unless treated urgently.
References
- Royal College of Ophthalmologists (2020) Management of ophthalmology services during the covid pandemic.
- University Hospital Southampton NHS Foundation Trust.
- Wickham L, Hay G, Hamilton R, et al. (2020) The impact of COVID policies on acute ophthalmology services- experiences from Moorfields Eye Hospital NHS Foundation Trust. Eye (Lond) 34: 1189-1192.
- Konstantakopoulou E, Edgar D, Harper R, et al. (2016) Evaluation of a minor eye conditions scheme delivered by community optometrists. BMJ Open 6: e011832.
- Hampshire Local Optical Committee.
- Harper RA, Dhawahir-Scala F, Wilson H, et al. (2020) Development and implementation of a greater Manchester COVID19 urgent eyecare service. Eye.
- Shih CK, Chan J, Lai J (2020) Maintenance of ophthalmic specialist out-patient service during the COVID-19 outbreak: The University of Hong Kong experience. Eye (Lond) 34: 1241-1242.
- Williams A, Kalra G, Commiskey P, et al. (2020) Ophthalmology practice during the coronavirus disease 2019 pandemic: The university of pittsburgh experience in promoting clinic safety and embracing video visits. Ophthalmol Ther 9: 1-9.
- Safadi K, Kruger J, Chowers I, et al. (2020) Ophthalmology practice during the COVID-19 pandemic. BMJ Open Ophthalmol 5: e000487.
- Romano MR, Montericcio A, Montalbano C, et al. (2020) Facing COVID-19 in Ophthalmology department. Curr Eye Res 45: 653-658.
- D'Oria F, Bordinone MA, Rizzo T, et al. (2020) Validation of a new system for triage of ophthalmic emergencies: The alphabetical triage score for ophthalmology (ATSO). Int Ophthalmol 40: 2291-2296.
- Rossi T, Boccassini B, Iossa M, et al. (2007) Triaging and coding ophthalmic emergency: The Rome Eye Scoring System for Urgency and Emergency (RESCUE): A pilot study of 1,000 eye-dedicated emergency room patients. Eur J Ophthalmol 17: 413-417.
- (2020) Coronavirus (COVID-19) in the UK.
Corresponding Author
Muhammed Jawad, Department of Ophthalmology, Southampton General Hospital, Coxford Rd, Southampton, SO16 5YA, UK.
Copyright
© 2020 Jawad M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.