Giant Plunging Ranula Presenting As an Emergency: A Case Report
Abstract
Plunging ranulas are pseudocysts which originate from major salivary glands and present as neck swellings with possible life-threatening complications. We present an unusual case of a plunging ranula which presented as an emergency. The patient presented at our clinic with a 4-year history of an asymptomatic recurrent neck swelling which we diagnosed as a ranula. She was clinically stable and we planned for elective surgery in five days. However, three days after clinic review, she presented at the emergency room on account of dyspnoea and dysphagia. She was hospitalized and the surgery was carried out as an emergency, life-saving procedure. This case highlights the importance of anticipating life-threatening complications in seemingly clinically stable cases of plunging ranulas.
Keywords
Plunging ranula, Emergency
Introduction
A salivary mucoele is a fluctuant lesion that forms in the oral cavity in relation to a salivary gland and is more commonly found in the labial or buccal mucosa where it is typically few millimeters in dimension. However, less commonly, it may occur in the floor of the mouth where it may be referred to as a ranula and may attain huge dimensions [1]. A ranula is referred to as "oral" or "superficial" if it is limited to the oral cavity above the mylohyoid, and "deep diving", "plunging" or "cervical" if it lies below the mylohyoid [2-4]. Plunging ranulas are rarer than oral ranulas [4].
A plunging ranula typically presents as a neck swelling which may remain asymptomatic [5,6]. However, it may become symptomatic presenting with signs of local compression like dysphagia and on rare occasions, life-threatening airway compromise. This case report highlights this possibility and the need to prepare for such eventualities when managing seemingly clinically stable cases of plunging ranulas.
Case Report
A 28-year-old woman presented at the oral and maxillofacial surgery clinic of the Nigerian Navy Reference Hospital, Calabar with a 4-year history of a neck swelling. There was a history of trauma to the lower jaw from assault about 3 months prior to the onset of the swelling. The swelling started under the tongue and gradually increased in size till about a year later, when she noticed the swelling extending into the neck. The swelling was mostly painless except when it was traumatized, causing it to burst and release its fluid contents into the mouth. On two occasions, she presented at lower-level facilities where it was drained, leading to transient resolutions but recurrence few weeks to months later. At presentation in our clinic, she was otherwise healthy, except for mild dysphagia and psychosocial complications.
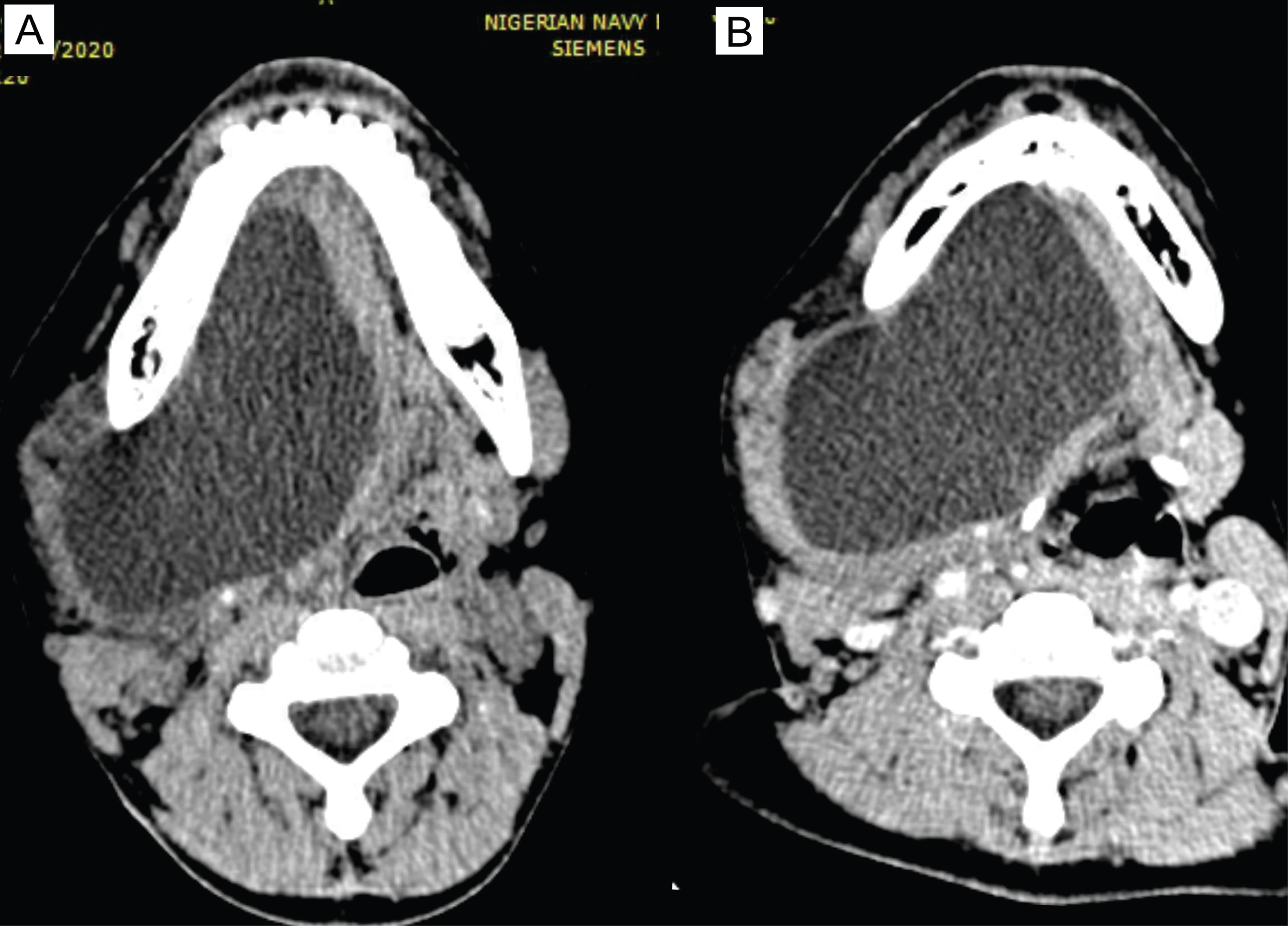
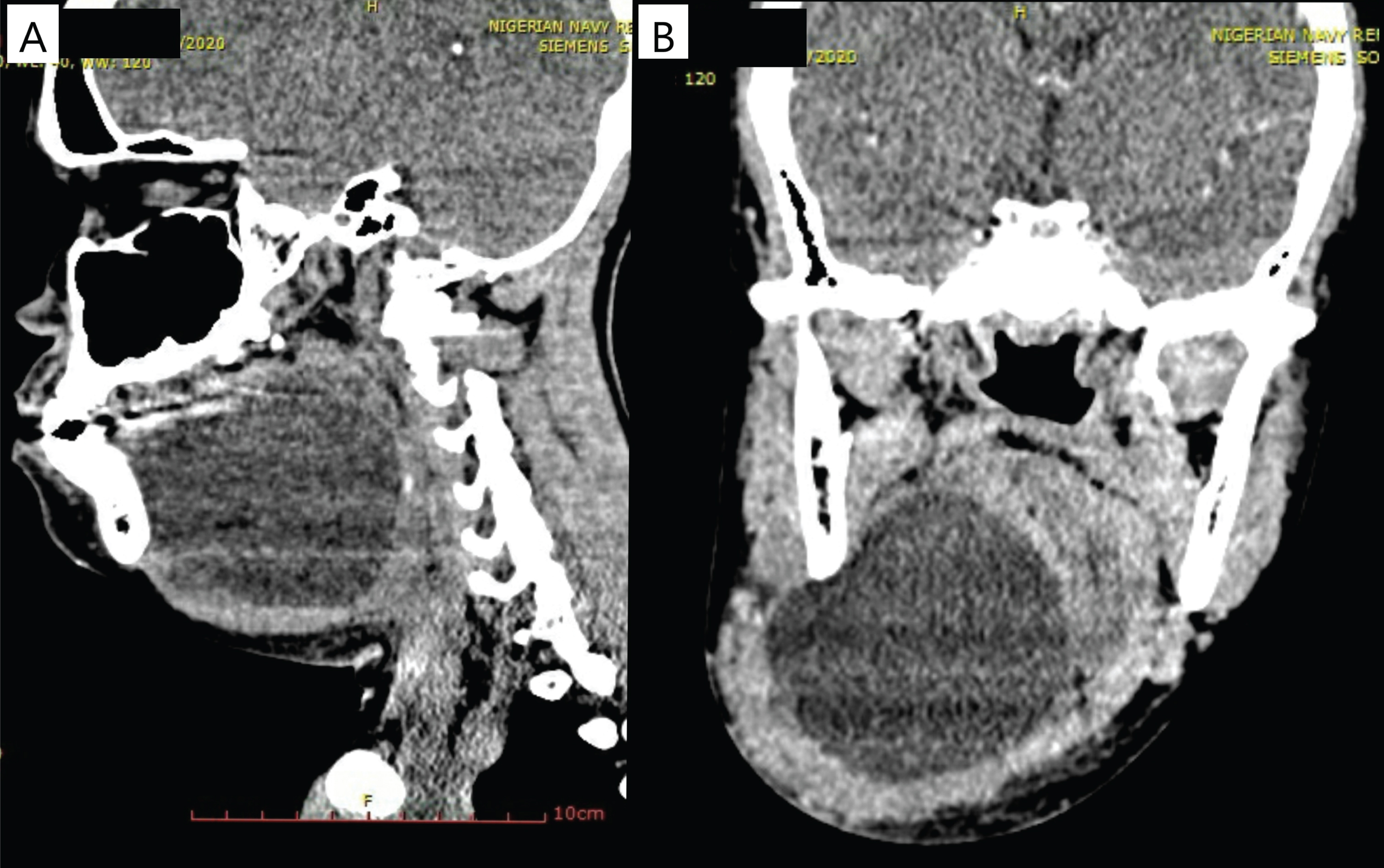
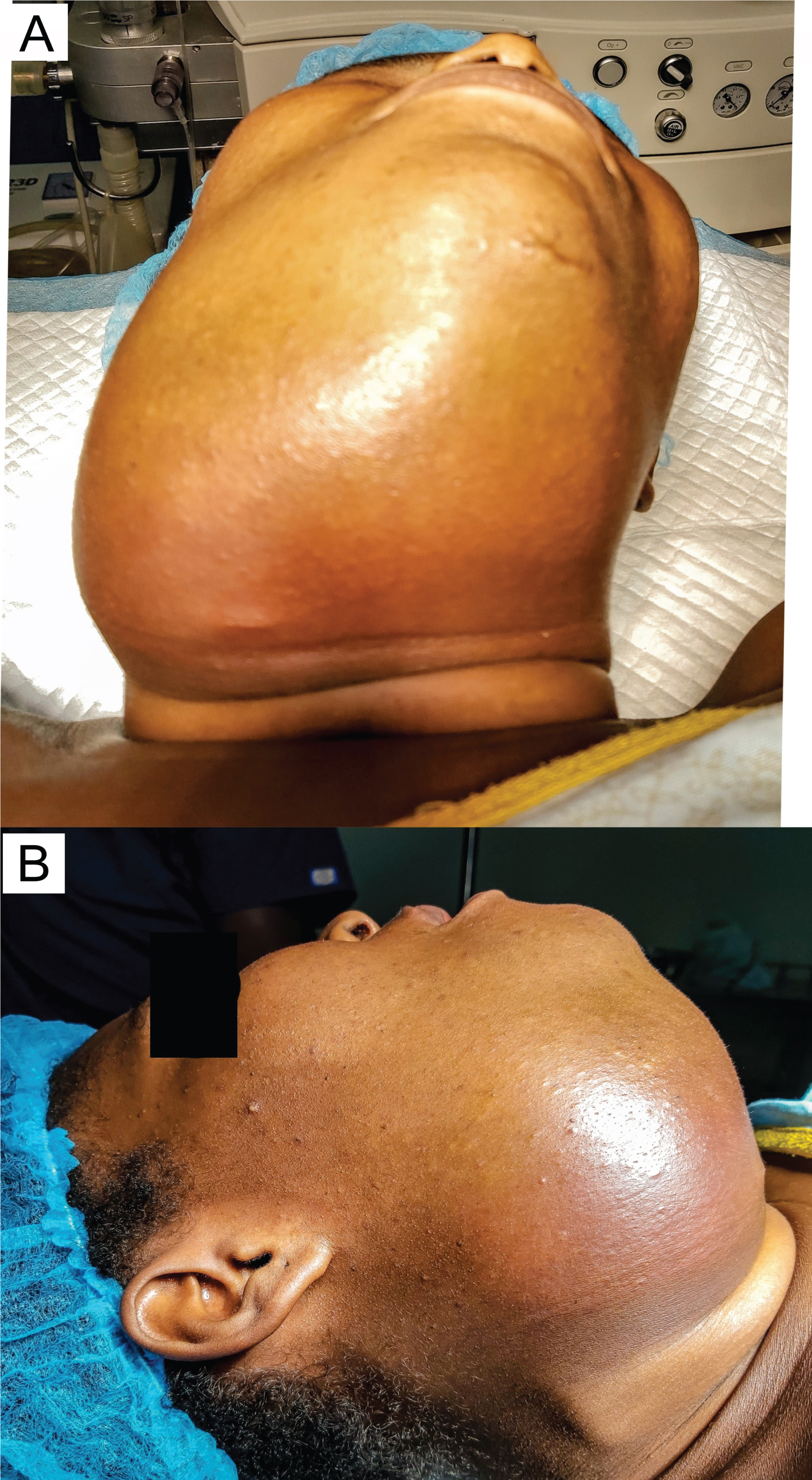
On examination, she was clinically stable and not in any distress. There was a painless, fluctuant swelling involving the submental, right submandibular and pretracheal regions. The swelling measured about 7.3 cm in its widest dimension and also diffused to the face over the right body of the mandible. Intraorally, there was a mild elevation of the tongue on the right. The anatomy of the sublingual and submandibular salivary glands could not be appreciated on palpation (Figure 1 and Figure 2). We aspirated a viscous, whitish fluid and made a provisional diagnosis of a plunging ranula with a differential diagnosis of a benign salivary gland neoplasm. A CT scan showed a cystic mass measuring 6.96 × 8.71 × 6.66 cm with an enhancing wall, displacing several neck structures and compressing the pharynx (Figure 3 and Figure 4).
The plan was to admit her and work her up for surgery scheduled for five days later, but due to financial constraints, she declined admission. However, three days after clinic review, at about 11.40 pm, the patient reported at the emergency room (ER) with progressively worsening dysphagia and dyspnoea. For six hours prior to presentation, she had not been able to swallow clear fluids and had needed to lean forward to breathe comfortably. On review at the ER, she was adjudged to be in moderate respiratory distress.
The swelling now measured about 9.6 cm in its widest dimension and was tender. Unlike the presentation in the clinic, the skin over the swelling was now shiny, dusky red and warm to touch, necessitating the impression of a superimposed infection. Via needle aspiration, about 150 ml of cystic fluid was drained and a sample was sent for microbiological examination. She was placed on oxygen therapy with close monitoring of SpO2 and other vital signs. After about 30 minutes, her respiratory condition began to improve. Empirical antimicrobial therapy (IV cefuroxime and metronidazole) was commenced as she was being worked up for surgery.
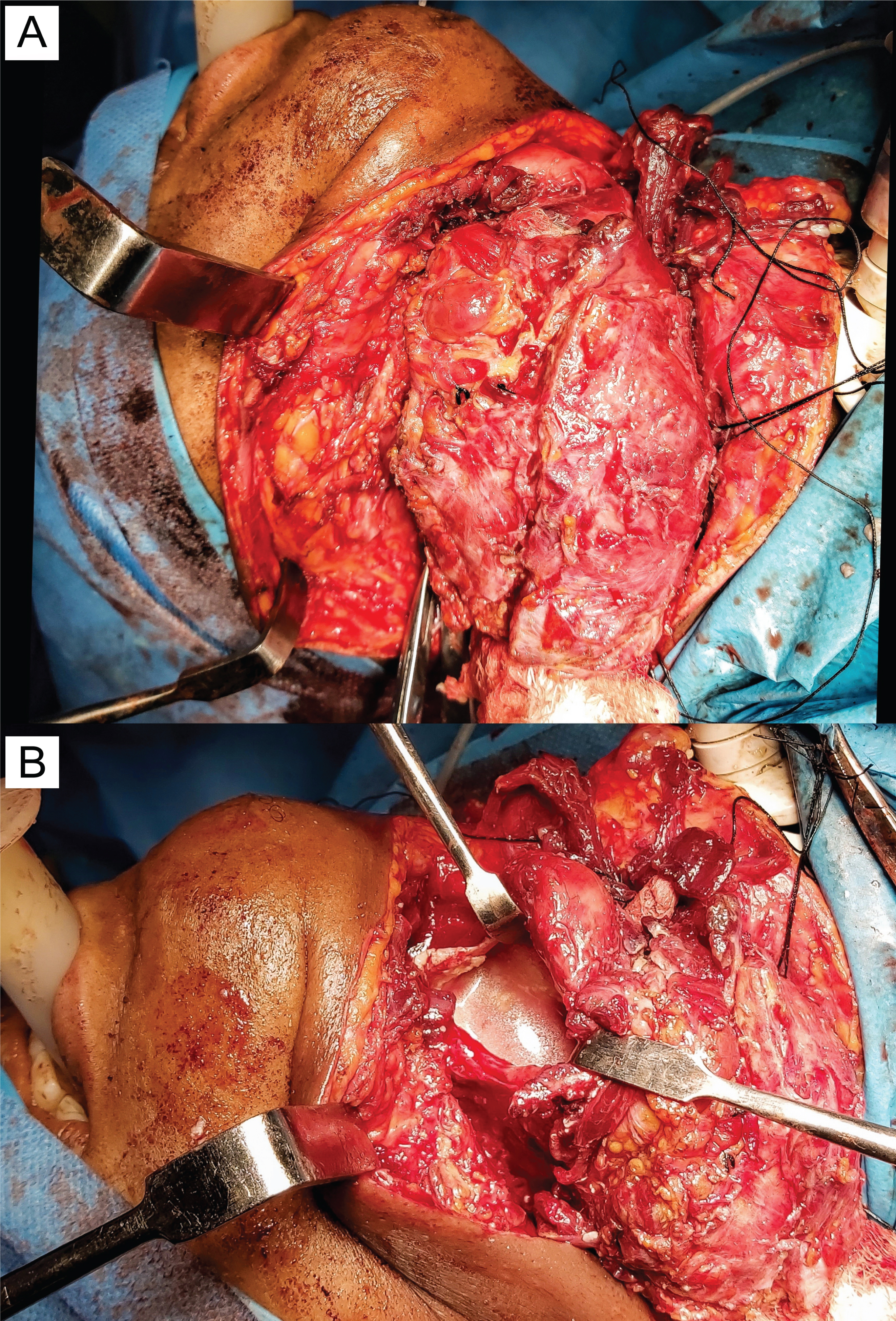
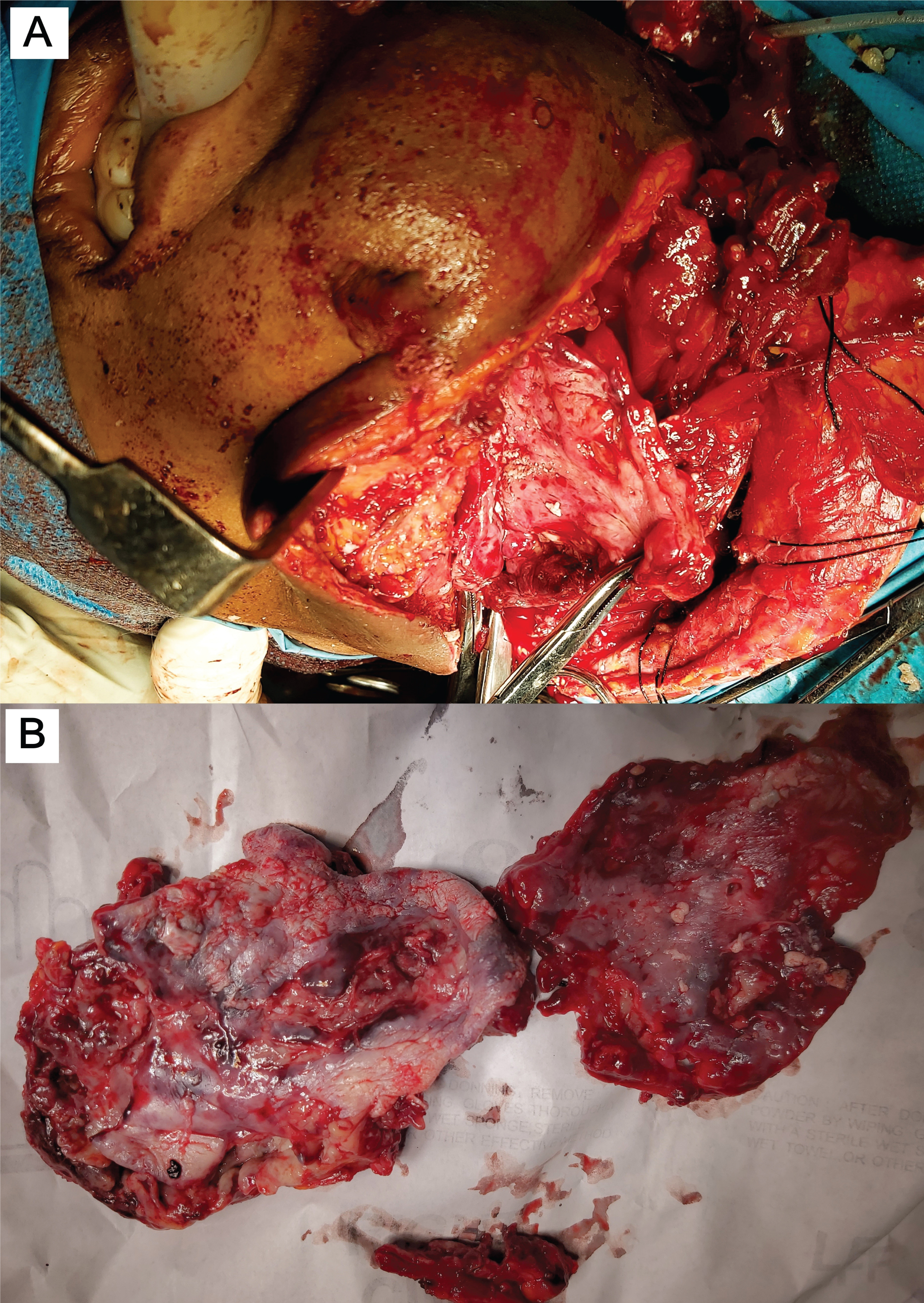
About 8 h 25 min after the ER presentation, she was taken into the operating room for surgery (Figure 5). General anaesthesia was instituted via a tracheostomy. Through a submandibular incision, the cystic capsule was exposed in all aspects except at the floor of the mouth where it was adherent to the mucosa. This aspect was left to be dissected last. The platysma and the subcutaneous tissue overlying the cyst were found to have been attenuated by the cystic compression.
To ease delivery, the cyst was drained and deflated (Figure 6). The thick, fibrous capsule was divided into two parts with the inferior part delivered first and the superior part dissected out from the floor of the mouth and pharynx (Figure 7). The altered anatomy made it impossible to identify the submandibular and sublingual salivary glands. However, it was certain that both glands must have been excised with the harvested tissue. At the end of the dissection, the surgical bed was examined and we were certain that no remnant salivary gland tissue was left behind. All surgical samples were sent for histology.
After 3 hours in the high-dependency unit, she was transferred to the open ward. The microbiological examination returned a scanty growth of S. aureus which was sensitive to cefuroxime while the histology report confirmed the diagnosis of a submandibular gland mucus extravasation cyst. She was discharged on the 8th postoperative day and has since recovered successfully. She was recalled at the 13th postoperative week (Figure 8) and there was no sign of recurrence.
Discussion
A ranula is a typically bluish, cyst-like mucosal swelling that forms in the floor of the mouth. This appearance resembles a frog's translucent belly giving it the name "ranula" which derives from the Latin word "rana" for "frog". The term is used for two pathogenetically distinct entities which are mucus extravasation cysts (MECs) and mucous retention phenomena (MRP) [2]. A MEC results when mucus leaks out of a traumatized salivary gland into the surrounding connective tissue. The leaked mucus elicits a chronic inflammatory reaction forming a granulation capsule around the lesion. A MRP on the other hand results from obstruction in the gland or duct leading to the retention of mucus and enlargement [1,4]. The obstruction may be from sialolithiasis, a tumour, or a stenosis.
A plunging ranula is almost exclusively due to extravasation. Other pathogenetic mechanisms include aberrant ducts from the sublingual gland to the submandibular duct, anatomical defects and openings in the mylohyoid muscle, and ectopic sublingual glands below the mylohyoid muscle [4].
A ranula is an uncommon disease. A Chinese survey reported a prevalence of 20 per 100,000 with a peak incidence in the second decade of life [3] while a New Zealand survey reported an incidence of 24 per 1,000,000 person-years [7]. Ranulas are commoner in males which may be explained by the aetiological association with trauma [3,7,8].
Trauma is a major aetiological factor in the development of ranulas [1,9] and we were able to elicit a history of trauma in our case. However, the role of trauma in this case cannot be ascertained. The long duration of the cyst before presentation in our case might be due to the series of drainages both by self-trauma and practitioners. This is similar to the case report by Gupta and Karjodkar in which there was a surgical intervention by a family physician, six months before presentation [10].
At presentation, we considered a differential diagnosis of a neoplasm because, as reported by Sousa Melo, et al. a neoplasm like mucoepidermoid carcinoma can mimic a ranula [11]. Other differential diagnoses of a plunging ranula include cystic hygroma, brachial cyst, and an abscess [4] but in our case, the history and examination findings successfully ruled out these differential diagnoses.
We anticipated life-threatening complications and therefore preemptively planned for immediate hospitalization for close monitoring of clinical condition and preoperative workup, but the patient declined immediate admission. We then counseled her on the possibility of life-threatening complications before admission and the need to report at the ER as soon as she noticed any unfavourable symptom.
Most cases of ranulas are stable with no life-threatening complications [3]. This explains the rarity of reports of life-threatening cases or acute presentations in literature. While writing this case report, we did an English Pubmed search and were able to find only five reports of acute presentations. Of the five reported cases, only three cases presented with respiratory distress [12-14] while the other two cases presented acutely for general discomfort, dysphagia, and speech difficulty [15,16]. Our patient presented with respiratory distress and dysphagia.
When our patient reported acutely in the ER, the cyst appeared to have been infected. This could have explained the rapid increase in size over the previous 48 hours and necessitated our commencement of empirical antibiotic therapy. Urgent surgery was required like it was required in the other reported cases of acute presentation. Due to the complicated anatomy of the mass, intubation was unsuccessful and tracheostomy was done. This is in contrast to the other cases in which intubation was successful.
Ranulas are notorious for recurrence and this has created a controversy about the best surgical management. Although most authors recommend the excision of the sublingual gland as the mainstay of the surgical management, some other authors favour other modalities like cystectomy alone [17] or in combination with sublingual sialadenectomy [4,5,18].
In three of their four cases, Olojede, et al. used the transcervical approach for adequate access to remove the sublingual gland and evacuate the extravasated fluid [18]. This is similar to our case in which the size necessitated the transcervical approach for adequate access and we decided for sialadenectomy. However, due to the huge dimensions of the mass, we could not radiologically ascertain if the cyst was from the submandibular or sublingual gland. Moreover, the anatomy of the glands could not be appreciated intraoperatively as they appeared to have been distorted by the long-standing compression effect of the cyst and incorporated into the thick capsule. We therefore decided to clear the surgical bed of any salivary gland tissue.
Conclusion
Typically, ranulas are asymptomatic. However, they can occasionally present as life-threatening emergencies requiring urgent intervention especially when they attain huge sizes in the neck. When huge and long-standing, they can also distort local anatomy making intraoperative dissection challenging. Therefore, surgeons need to be prepared for this possibility when managing similar cases.
Ethical Approval
Informed consent was obtained from the patient.
Conflict of Interest
The authors declare they have no conflicts of interest in the studies performed.
References
- Hayashida AM, Zerbinatti DC, Balducci I, et al. (2010) Mucus extravasation and retention phenomena: A 24-year study. BMC Oral Health 10: 10-15.
- Kolomvos N, Kalfarentzos E, Papadogeorgakis N (2019) Surgical treatment of plunging ranula: Report of three cases and review of literature. Oral Maxillofacial Surgery Cases 5: 100098.
- Zhao YF, Jia Y, Chen X, et al. (2004) Clinical review of 580 ranulas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 98: 281-287.
- De Visscher JG, van der Wal KG, De Vogel PL (1989) The plunging ranula: Pathogenesis, diagnosis and management. J Craniomaxillofac Surg 17: 182-185.
- Nilesh K, Malik NA, Patil P, et al. (2015) Large plunging ranula presenting as isolated neck swelling: Steps in diagnosis and surgical steps in management. J Clin Diagn Res 9: MD01-MD3.
- Macdonald AJ, Salzman KL, Harnsberger HR (2003) Giant ranula of the neck: Differentiation from cystic hygroma. AJNR Am J Neuroradiol 24: 757-761.
- Chin SJ, Zeng IS, Morton RP (2016) The epidemiology of plunging ranula in South Auckland. Laryngoscope 126: 2739-2743.
- Lyly A, Castren E, Aronniemi J, et al. (2017) Plunging ranula - patient characteristics, treatment, and comparison between different populations. Acta Otolaryngol 137: 1271-1274.
- Bezerra TMM, de Brito Monteiro BV, Henriques ACG, et al. (2016) Epidemiological survey of mucus extravasation phenomenon at an oral pathology referral center during a 43 year period. Braz J Otorhinolaryngol 82: 536-542.
- Gupta A, Karjodkar F (2011) Plunging ranula: A case report. ISRN Dent 2011: 806928.
- Sousa Melo SL, Lanzel E, Pagedar NA, et al. (2018) Mucoepidermoid carcinoma mimicking a mucocele (ranula) in the floor of the mouth. Dentomaxillofac Radiol 47: 20170331.
- Ovet G, Alatas N, Guzelkara F, et al. (2015) A rare cause of acute respiratory distress: Cervical ranula. Turk Arch Otorhinolaryngol 53: 133-135.
- Effat KG (2012) Acute presentation of a plunging ranula causing respiratory distress: Case report. J Laryngol Otol 126: 861-863.
- Sathanantham DK, Shah GB, Ulualp S (2015) Rapid development of a simple ranula in a child. Ann Otol Rhinol Laryngol 124: 322-325.
- Thimann D, Huang C, Patel K (2012) Images in emergency medicine. 10-year-old female with a subglottic mass. Ranula. Ann Emerg Med 60: 668-677.
- Dayton K, Ryan MF (2014) Symptomatic floor-of-mouth swelling with neck extension in a 14-year-old girl. Case Rep Pediatr 2014: 831923.
- Baurmash HD (2007) A case against sublingual gland removal as primary treatment of ranulas. J Oral Maxillofac Surg 65: 117-121.
- Olojede ACO, Ogundana OM, Emeka CI, et al. (2018) Plunging ranula: Surgical management of case series and the literature review. Clin Case Rep 6: 109-114.
Corresponding Author
Peter Olalekan Adeosun, Oral and Maxillofacial Surgery Division, Nigerian Navy Reference Hospital, Calabar, Cross River State, Nigeria, Tel: +2348037766147
Copyright
© 2021 Adeosun PO, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.