Assessment of the Success of Oral Rehabilitation of Patients with with Teeth Loss and Class III Skeletal Malocclusion
Abstract
Objective: The objective of the study is to assess treatment success of teeth loss patients with class III skeletal malocclusion through a multidisciplinary approach, including orthognathic surgery and implant prosthetic rehabilitation.
Materials and methods: The present retrospective study aimed at investigating the 5-year clinical treatments outcomes 16 patients with class III malocclusion and teeth loss. Clinical, laboratory, radiological methods were used in the examination of patients. Surgical stage included sagittal bilateral osteotomy of the lower jaw and reposition it back.
Le Fort I osteotomy, 7-8 months after the orthognathic surgery 132 implants were inserted. After 2 to 4 months of submerged healing period patients had received implant-fixed prostheses.
Results: No serious intraoperative or immediate postoperative complications were noted. At the control examination after 6 months after surgery, an X-ray examination we did not observe any clinical or radiological signs of inflammation in the area of osteotomy sites and titanium mini plates. Success rate of implants 5 years after was 96.2%.
Conclusion: After orthognathic surgery and dental implant prosthetic rehabilitation, the masticatory function, esthetics of the facial profile and occlusion was improved. Patients expressed satisfaction with the result of treatment and improved quality of life.
Keywords
Orthognathic surgery, Implant prosthetic rehabilitation, Skeletal class III malocclusion
Abbreviations
CT: Computed Tomography; TMJ: Temporo Mandibular Joint; 3D: Three-dimensional; MBL: Mean Marginal Bone Loss
Introduction
Malocclusion is one of the anomalies maxillofacial area. There are several classifications of malocclusion. In 1899 Angle was the first who classified malocclusions into 3 types of Class I, Class II, and Class III [1]. Angle classifications of malocclusion based on the relationship of the first molars and the alignment (or lack of it) of the teeth relative to the line of occlusion.
Class III malocclusion may present with various combinations of dentoalveolar problems [2]. Class III malocclusions classified into 3 types: pseudo, dentoalveolar, and skeletal [3,4]. The etiology of Class III malocclusion is multifactorial, with genetic, ethnic, environmental, and habitual components [5]. Orthognathic surgery is a first approach to treat Class III malocclusion and can be addressed with various surgical approaches [6,7]. The type of surgical treatment depends upon the etiology of the malocclusion and may include sagittal split osteotomies, segmental osteotomies, Le-Forte I osteotomies, or some combination of the aforementioned [8,9]. Orthognathic surgical procedures have been traditionally used in the dentate patient to correct a skeletal malocclusion. However, orthognathic surgery is often recommended for the adult patient presenting with a skeletal malocclusion and teeth loss a desire to restore esthetic and functional relationship [10]. Tooth loss can have a effect on a patient's quality of life due to poor masticatory function, speech and dissatisfaction with appearance. Oral rehabilitation of patients with skeletal malocclusion and teeth loss are challenging procedures and are challenged by the skeletal discrepancies of the maxilla and the mandible [11].
Conventional restorations as removable prostheses can be a limitation for patients with skeletal malocclusions due to poor occlusions. Over the past decade dental implant prosthetic rehabilitation are used for replacing missing teeth in various clinical situations. Patients treated with dental implants to support prostheses have better masticatory function and higher satisfaction, than patients treated with conventional complete dentures [12-14]. For complete denture wearers the chew's ability is less efficient. Without the use of implants to create stability and retention, placing denture teeth can create instability of the prosthesis [15].
Patients with dentofacial deformities orthognathic surgery and implant prosthetic treatment may be possible to complex oral rehabilitation and are providing effects on the speech, chewing, smile and patient respiratory parameters [16].
The most encountered complications orthognathic surgery are post-operative infection, hemorrhage, neurosensory disturbances, and incorrect condylar position [17-19]. Prevention of complications depends largely on the knowledge and skills of the surgeon, multi-disciplinary approach would be prevent and minimize intra and post op complications.
Rehabilitation of patients with Class III malocclusion and teeth loss is one of the urgent problems of orthognathic surgery. In this group of patients to ensure accurate diagnosis, optimal planning and appropriate treatment, a comprehensive interdisciplinary approach is often necessary, in which orthopedists, orthodontists, periodontists, oral and maxillofacial surgeons should participate [20-22]. The interaction established among different specialties provides patients with a comprehensive treatment plan [23,24]. The objective of the study is to assess treatment success of teeth loss patients with class III skeletal malocclusion through a multidisciplinary approach, including orthognathic surgery and implant prosthetic rehabilitation.
Methods
16 patients with class III skeletal malocclusion and teeth loss (5 patients totally and 11 patients partially edentulous) were treated for orthognathic surgery and implant prosthetic rehabilitation between 2014 and 2019. The ages of the patients ranged between 26-years and 43-years (7 males and 9 females). All patients presented functional and esthetic complaints. Clinical, laboratory, radiological methods were used in the examination of patients. Patients were evaluated by preoperative and postoperative outcome using computed tomography scan evaluation. Clinical data included demographic and clinical variables: (1) gender, (2) age, (3) method of orthognathic surgery, (4) type of implant surgery and dental prosthetic rehabilitation.
Local status: assessment of topographic and anatomical relationships of the upper and lower jaw, evaluation of occlusal relationships, evaluation of dental status, oral hygiene. The treatment plan included detailed analysis of occlusion, space for restoration, bone quantity and density, determination of which teeth were essential for prosthodontic treatment and which teeth had a hopeless periodontal prognosis. Sanitation of the oral cavity as needed. Final treatment plan was drawn up using a team approach with orthodontics, periodontics, oral and maxillofacial surgeons, and prosthodontics. The orthognathic surgery was planned with the aid of 3D computed tomography. Data obtained from CT scan procedure can view the virtual 3D model from different angles using the software to customize the treatment plan. The purpose of treatment: the elimination of abnormal development of the jaws, the elimination of interlocking dentition, dental defects. The choice of surgical treatment is determined by the type of anomaly, the degree of deformation.
The complex oral rehabilitation was performed with orthognathic surgery followed by implant prosthetic treatment. All patients were fully informed of the protocol of the present study and signed a detailed informed consent.
Surgical Technique
The surgical procedure included two stages: orthognathic surgery and implant installation surgery performed 7 to 8 months after reconstruction. All surgical procedures (orthognathic surgery and implant installation) were performed by one surgical team.
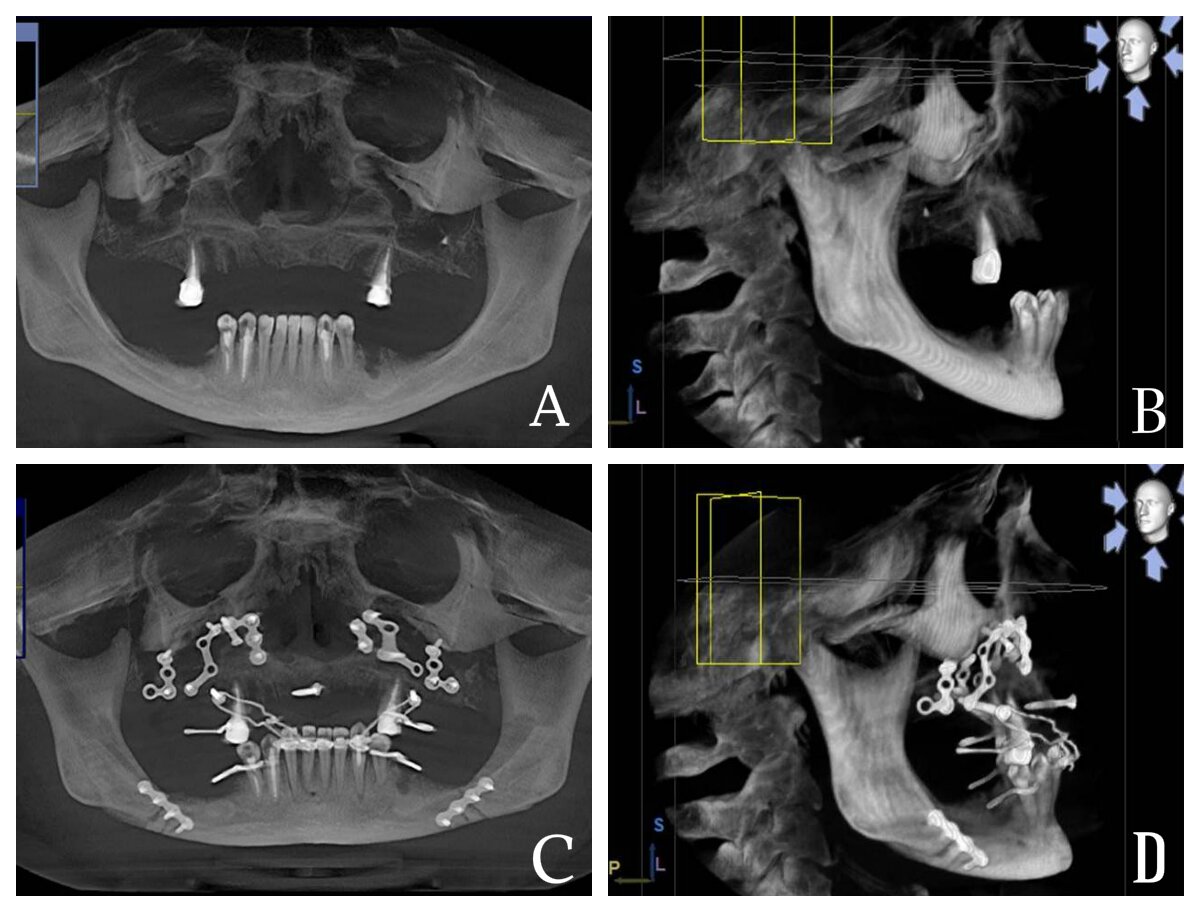
Le Fort I osteotomy and mandibular orthognathic surgery was performed under general anesthesia. After Le Fort I osteotomy maxillary alveolar process was anteriorly positioned as planned by computed tomography analysis and was stabilized using titanium miniplates and screw. After sagittal split osteotomy, the mandible was repositioned posteriorly and was stabilized in the desired position using titanium miniplates and screw or wire fixation (Figure 1A,B,C,D).
Preoperative antibacterial therapy was given day prior to surgery and were continued for another 5 days postoperatively to prevent inflammatory complications. Intraoperative and postoperative complications, such as bleeding, swelling, pain and nasal bleeding, neyrosensory disorders, infection were recorded. We celebrated the residual effects of neurosensory disorders in 3 patient which disappeared within 3-6 weeks.
After orthognathic surgery, the esthetics of the facial profile and occlusion was improved significantly.7-8 months after the orthognathic surgery 132 implants were inserted. After implant insertion, the cover screw was connected. The mucoperiosteal flap was carefully sutured to submerge the implants. Implant length and diameter were chosen based on the bone volume in the implant sites and base on the prosthetic indication. The diameter of the implants used was 3.75 - 4.5mm, lengths was 10 -15mm. Postoperative clinical and radiographic controls were made regularly, the criteria for implant success were assessed. The dental prosthetic phases started 3 to 5 months after implant submerged healing period. The cover screws were removed and changed into healing abutments and prosthetic fabrication was carried out. Patients had received implant-bridge and hybrid denture that provided ideal facial balance and occlusion. The prosthetic indication was made according to each patient clinical condition in order to achieve the highest function and esthetic.
Assessment of masticatory function was made both subjectively and objectively. Masticatory performance was objectively evaluated by chewing of a piece of color-changeable chewing gum (Xylitol, Lotte, Tokyo, Japan) for 60 strokes. This method is easy, simple, and quick, with no need for bulky equipment, and it has advantages in stimulating a natural and stable act of chewing while still allowing complete recovery of the test item. Color-changeable chewing gum has been applied in various fields. This gum base contains red, yellow, and blue dyes, citric acid and xylitol. With the progression of chewing, the color of the chewing gum turns from yellowish green to red [25]. Positive value indicating redness, and negative value indicating greenness.
An implant was considered to have failed (clinical or absolute failure) if it had any of the following conditions: pain on function, mobility, radiographic bone loss > 1/2 the length of the implant, uncontrolled exudate, or was no longer in the mouth [26]. Clinical examination was performed to evaluate peri-implant and periodontal tissue, implant stability. Success of oral implant rehabilitation were prosthesis success; implant success; complications; probing pocket depths; marginal bleeding; and bone marginal bone loss (MBL).
Radiograph was used to detect any bony abnormality and evaluate alveolar bone around each implant and made as average value. Postsurgical change in marginal bone level was assess by digital X-ray were taken immediately (base line for comparison) and 3 months after implant installation, after prosthesis loading, 1- year, 3-years, and 5- years after implant installation.
Statistical Analysis
Statistics were used to calculate and analyze the mean marginal bone loss of implants. The differences between follow-up periods were tested by paired Student's t test. All analyses were carried out using SPSS (SPSS Software Company, Chicago, IL, USA). p values < 0.05 were considered statistically significant.
Case Report
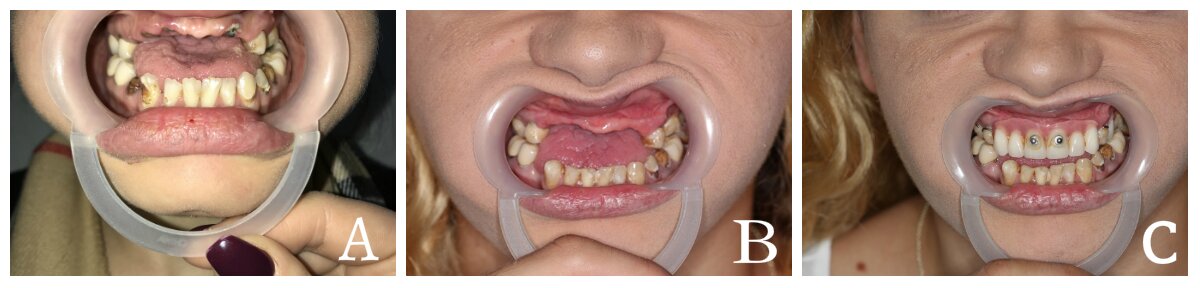
This case report describes the multidisciplinary approach, including endodontic treatment, cystectomy, orthognathic surgery, and implant prosthetic rehabilitation. The interaction of multidisciplinary specialties and complex treatment planning were required. A 27-year-old female patient with multiple missing teeth and a malocclusion was unsatisfied with the esthetic aspects of her face and masticatory function. She also wanted to improve dental esthetics. Medical examination revealed that the patient presented good general health. Extra oral evaluation revealed pronounced chin, short lower face and prognathic mandibula (Figure 2A,B,C). Upon intraoral examination, partially teeth loss, multiple caries remaining teeth, and discrepancy between the dental arches were observed (Figure 3A).
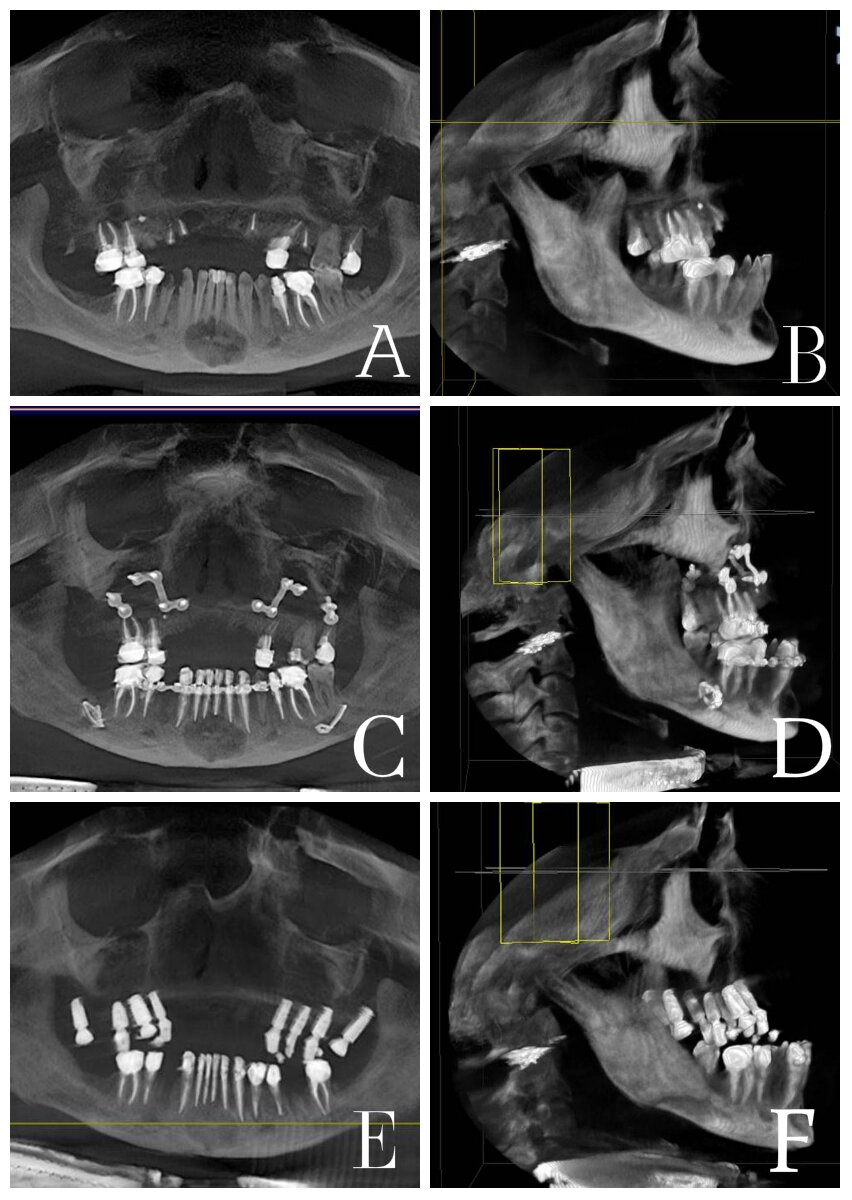
Occlusion was analyzed with the diagnostic casts mounted on articulator and computed tomography. Computed tomography evaluation confirmed the discrepancy between the dental arches, also revealed odontogenic cyst in frontal part of lower jaw, and alveolar bone loss in frontal part of maxilla (Figure 4A,B).
Dental diagnosis of conditions was multiple caries, chronic periodontitis, partially edentulous, Angle Class III malocclusion, alveolar bone loss in frontal part of maxilla. After discussing a treatment plan with periodontists, prosthodontists, orthodontists, oral and maxillofacial surgeons, selected a final treatment plan. The treatment plan included extraction hopeless teeth, endodontic treatment, cystectomy, periodontics phase, prosthodontics phase, followed by a orthognathic surgery phase, and a final implant prosthetic rehabilitation. The patient were detailed informed of the treatment plan and signed the informed consent. The orthognathic surgical stage was planned according to facial analysis, predictive computed tomography, and preparation of the surgical guide. The surgical procedures included a Le Fort I osteotomy and bilateral sagittal split osteotomy followed by dental implant treatment.
Аt the first stage of treatment were performed extraction teeth hopeless periodontal prognosis, endodontic treatment, splinting of the lower teeth, cystectomy and manufacturing temporary partial denture upper jaw (Figure -3 B,C).Temporary prosthetics at the preparatory stage of an orthognathic surgery is important, since during orthognathic surgery it is necessary to position the tooth-containing segments of the upper jaw in the state of central occlusion. One months after oral sanation orthognathic surgery (mandibular setback, Le Fort I osteotomy) was performed under general anesthesia in one stage. After sagittal split osteotomy, the mandible was repositioned posteriorly and was stabilized in the desired position using wire fixation. After Le Fort I osteotomy maxillary alveolar process was anteriorly positioned and was stabilized in the desired position using titanium miniplates and screws (Figure 4C,D).
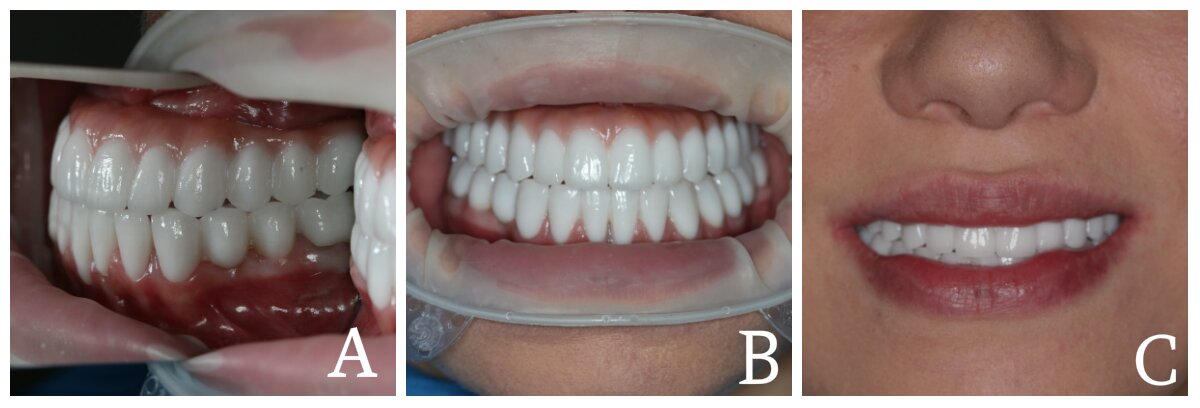
The post-operative period was uneventful, with only slight paraesthesia which disappeared within 3 weeks. Eight months after the orthognathic surgery, dental implants placement was performed. A total of 8 implants were inserted in upper jaw (2 implants placed in the tuber regions), and dental prosthetic rehabilitation was performed after five months of submerged healing (Figure 4E,F). Implant-fixed full arch prosthesis in upper jaw and tooth supported fixed prostheses in lower jaw was fabricated (Figure 5A,B,C). Clinical and radiographic controls were made regularly, the implant success was assessed. All the implants were stable and in good function with no postoperative complications. The facial posttreatment photographs show improvement in the facial profile (Figure 6A,B,C).
In these cases, alveolar crest bone loss in frontal part of maxilla is гrequires bone graft procedures for insertion of endoosseos implants. The benefits of using 2 implants in the tuber area and prosthodontic rehabilitation with implant-fixed full arch prosthesis include avoidance of bone grafting and donor side morbidity. After orthognathic surgery followed by implants prosthetic treatment anteroposterior discrepancy between the dental arches were satisfactorily. The patient had been successfully rehabilitated, with adequate masticatory function, good esthetics and was satisfied with his profile and smile line. This case report describes the multidisciplinary approach, including endodontic treatment, cystectomy, orthognathic surgery, and implant prosthetic rehabilitation. The interaction of multidisciplinary specialties and complex treatment planning were required.
A 27-year-old female patient with multiple missing teeth and a malocclusion was unsatisfied with the esthetic aspects of her face and masticatory function. She also wanted to improve dental esthetics. Medical examination revealed that the patient presented good general health. Extra oral evaluation revealed pronounced chin, short lower face and prognathic mandibula Upon intraoral examination, partially teeth loss, multiple caries remaining teeth, and discrepancy between the dental arches were observed. Occlusion was analyzed with the diagnostic casts mounted on articulator and computed tomography. Computed tomography evaluation confirmed the discrepancy between the dental arches, also revealed odontogenic cyst in frontal part of lower jaw, and alveolar bone loss in frontal part of maxilla (Figure 2A,B).
Dental diagnosis of conditions was multiple caries, chronic periodontitis, partially edentulous, Angle Class III malocclusion, alveolar bone loss in frontal part of maxilla. After discussing a treatment plan with periodontists, prosthodontists, orthodontists, oral and maxillofacial surgeons, selected a final treatment plan. The treatment plan included extraction hopeless teeth, endodontic treatment, cystectomy, periodontics phase, prosthodontics phase, followed by a orthognathic surgery phase, and a final implant prosthetic rehabilitation. The patient was detailed informed of the treatment plan and signed the informed consent. The orthognathic surgical stage was planned according to facial analysis, predictive computed tomography, and preparation of the surgical guide. The surgical procedures included a Le Fort I osteotomy and bilateral sagittal split osteotomy followed by dental implant treatment.
Аt the first stage of treatment were performed extraction teeth hopeless periodontal prognosis, endodontic treatment, splinting of the lower teeth, cystectomy and manufacturing temporary partial denture upper jaw. Temporary prosthetics at the preparatory stage of an orthognathic surgery is important, since during orthognathic surgery it is necessary to position the tooth-containing segments of the upper jaw in the state of central occlusion. One months after oral sanation orthognathic surgery (mandibular setback, Le Fort I osteotomy) was performed under general anesthesia in one stage. After sagittal split osteotomy, the mandible was repositioned posteriorly and was stabilized in the desired position using wire fixation. After Le Fort I osteotomy maxillary alveolar process was anteriorly positioned and was stabilized in the desired position using titanium miniplates and screws (Figure 2C,D).
The post-operative period was uneventful, with only slight paraesthesia which disappeared within 3 weeks. Eight months after the orthognathic surgery, dental implants placement was performed. A total of 8 implants were inserted in upper jaw (2 implants placed in the tuber regions), and dental prosthetic rehabilitation was performed after five months of submerged healing. Implant-fixed full arch prosthesis in upper jaw and tooth supported fixed prostheses in lower jaw was fabricated. Clinical and radiographic controls were made regularly, the implant success was assessed. All the implants were stable and in good function with no postoperative complications. The facial posttreatment photographs show improvement in the facial profile.
In these cases, alveolar crest bone loss in frontal part of maxilla is гrequires bone graft procedures for insertion of endoosseos implants. The benefits of using 2 implants in the tuber area and prosthodontic rehabilitation with implant-fixed full arch prosthesis include avoidance of bone grafting and donor side morbidity. After orthognathic surgery followed by implants prosthetic treatment anteroposterior discrepancy between the dental arches were satisfactorily. The patient had been successfully rehabilitated, with adequate masticatory function, good esthetics and was satisfied with his profile and smile line.
Results
During the clinical examination, the state of the temporomandibular joint, and the state of the prostheses on the implants were evaluated. The treatment objective was to achieve adequate esthetics profile, and to construct biomechanically favorable prosthesis to provide efficient masticatory function. During a clinical examination, we evaluated the general condition of the patient, revealed the presence of complaints of pain in the region of the upper and lower jaws, TMJ, and the presence of inflammatory phenomena in the area of dental implants and titanium mini plates.
No serious intraoperative or immediate postoperative complications were noted. 2 patients had a minor neyrosensor complication which disappeared within 3-4 weeks. This complication did not impede rehabilitation with dental implants. A total of 132 implants were installed in 16 patients. At the control examination 3 months after implant installation, after prosthesis loading, 1-year, 3-years, and 5 -years after implant installation, an X-ray examination was performed to determine the status of the osteotomy area, the status of dental implants, the mean marginal bone loss of implants (Table 1).
We did not observe any clinical or radiological signs of inflammation in the area of osteotomy sites and titanium mini plates. The implants were Osseo integrated, radiographies revealed no radiolucency around the implants and no sign of excessive peri implant bone loss. Patients presented with healthy soft tissue. A stable orthognathic occlusion was achieved in all patients, no recurrence of the disease was observed, which confirms the appropriateness of using dental implants for prosthetics in the complex treatment of patients with skeletal malocclusion and teeth loss.132 implants placed in these 16 patients, 2 failed to Osseo integrate and 3 after 3 years of loading (peri-implantitis). Success rate of implants 5 -years after was 96.2%.
The success rates of implants in maxilla were 96.4%, and the success rates of implants in mandible were 95.8%, There were no statistically significant differences in the success rate among implantation site, although the success rates in maxilla were higher than mandible (Table 2). The success rates of patients with ages less than 30-years old were 97.1%, and the success rates of patients with ages greater than 30-years old were about 95.9%. There were no statistically significant differences in the success rate among ages of patients, although the success rates of patients with ages less than 30-years old were higher than those with ages greater than 30- years old (Table 3).
Mean marginal bone loss (MBL) at 3 months after implant installation, after prosthetic loading, 1-year, 3-years, and 5-years after installation was significantly higher than MBL at the time of implant installation (p < 0.05). Mean marginal bone loss (MBL) at prosthetic loading was significantly higher than at 3 months post-installation, and mean MBL at 1 year after installation was significantly greater than at prosthetic loading. MBL change after 3- years, and 5 -years post-installation did not differ significantly (p < 0.05) (Table 4).
The mean MBL after the first year was 0.81 ± 0.42 mm, the mean cumulative MBL after 5- years was 1.42 ± 0.53mm, and the MBL change each year was not greater than 0.2 mm. These MBL results are within the threshold indicating success [27]. There were 2 groups regarding prosthetic indication, including bridge and hybrid denture. The difference between MBL value at 5 years post-installation and MBL at prosthetic loading of the bridge group was 0.94 ± 0.31 mm of the hybrid denture group was 0,76 ± 0,28 mm (p < 0.05). (Table -5).Mean marginal bone loss (MBL) bridge prosthesis group was significantly higher than hybrid denture prosthesis group (p < 0.05).
The results showed that implant treatment is effective to improve patient's masticatory efficiency. The gum initially had a greenish color and became more-and-more reddish with the duration and intensity of chewing, and there is a strong correlation between color change and masticatory performance and ability. Masticatory efficiency correlated with occlusal contacts, occlusal area of natural teeth, and the number of posterior teeth. Treatment with implant‐based fixed prosthesis in patients with Angle Class III malocclusion and teeth loss results in an improved satisfaction regarding dental appearance, ability to chew and speech. After orthognathic surgery and dental implant prosthetic rehabilitation, the esthetics of the facial profile and occlusion was improved. Patients expressed satisfaction with the result of treatment.
Discussion
Malocclusions are one of the most common pathologies in the maxillofacial area and the treatment of patients with these pathologies remains an urgent problem. Treatment of skeletal Class III malocclusion in an adult requires surgical procedures, with the aim to achieve normal occlusion and improve facial esthetics. Oral rehabilitation of patients with Angle Class III malocclusion and teeth loss due to difficulty sometimes requires surgical, orthodontic, and prosthetic treatments combination. The main objectives of this interdisciplinary approach are to restore the facial and dental harmony, functional occlusion [28]. The best result of the operation is achieved only with a team approach.
Orthognathic surgery is distinguished by a high degree of predictability of the postoperative result and fully restored occlusion of the dentition. Harmony of the face and smile when performing a comprehensive orthognathic surgery of patients with skeletal deformities of the maxillofacial area should be achieved by detailed planning of the orthodontic, surgical, and orthopedic stages [29]. Orthognathic surgery can play an important role in complex restorative dental problems that cannot be successfully managed in the presence of a jaw size discrepancy [30]. In cases with teeth loss, implant therapy is a necessary step to restore the masticatory function and should be included in the treatment plan in the early stages. Restoration of the dentition plays an important role in the treatment of this category of patients. Implant therapy allows to increase the functional and esthetic efficiency combination treatment for patients with class III malocclusion and edentulous jaws.
Alternatively, removable denture represents a second treatment option for this patient [31]. However, in patients with class III malocclusion and teeth loose difficult to achieve a satisfactory esthetic result with conventional prosthetic restoration, its functionally and esthetically effectiveness is lower compared implant-fixed prostheses. Implant-retained restorations present considerable advantages over removable partial dentures for missing teeth including a more stable occlusion, preservation of bone.
Correlation between masticatory performance and quality of life of patients using posterior dental implant
It is of interest to evaluate the results of treatment of patients with skeletal forms of Class III malocclusion, complicated by the loss of teeth in order to increase its effectiveness and to obtain a predictable result of treatment, because there is inadequate published information about the prevalence of teeth loss in such patients. This study is based on an analysis of the results of treatment of 16 patients with skeletal form class III malocclusion and teeth loss who underwent combination of orthognathic surgery (maxillary Le Fort I osteotomy and mandibular setback) procedure and implant prosthetic rehabilitation. Planning and evaluation of the quality of treatment was carried out on the basis of a detailed assessment of the aesthetic parameters of the face using clinical photography, X-ray examination of the jaws in the front and side projections. The functional and esthetic rehabilitation was performed with orthognathic surgery, dental implants, and prosthodontic therapy to restore missing tooths and occlusion.
We considered successful treatment criteria: the normal position of the temporomandibular joint with both sides; achievement of central occlusion; the state of the chewing apparatus, allowing completely perform a chewing function; patient satisfaction with their appearance. The use of dental implants in the treatment of patients with skeletal form class III malocclusion and teeth loss allows to achieve a stable state of occlusion in the postoperative period. As a result, complex treatment, the patients were successfully rehabilitated and correction of the anteroposterior discrepancy between the dental arches with no recurrent malocclusion.
The long-term results of the use of dental implants in the complex treatment of such patients have been evaluated. Dental implantation is the best choice for complex oral rehabilitation of patients with class III malocclusion and teeth loss for cases similar to that demonstrated in the present report. Treatment not only restored function and esthetics, but also showed a positive psychological impact. The multidisciplinary approach proved to be effective in overcoming the challenges. The teamwork of the team of doctors is the key to successful treatment of these patients, and accordingly leads to patient satisfaction with the quality of the treatment carried out.
Conclusion
Dental implant prosthetic rehabilitation is the method of choice in the complex treatment of patients with skeletal form class III malocclusion and total or partial teeth loss. Dental implantation in such cases provides a complete occlusion efficient masticatory function and significantly reduces the risk of recurrence.
Declarations
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' Contributions
Khachatryan Levon, Hakobyan Gagik: Conceived of the study and participated in its design and coordination.
Tunyan Gegham, Hakobyan Gagik:Made substantial contributions to data acquisition and conception of manuscript.
Tunyan Gegham, Khachatryan Levon, Khachatryan Grigor, Hakobyan Gagik: Drafted and designed the manuscript.
Ethics Approval and Consent to Participate
This protocol was approved by the Clinical Research Ethics Committee Yerevan State Medical University after M. Heratsi (protocol N3 17.11.16) and in accordance with those of the World Medical Association and the Helsinki Declaration.
Acknowledgements
Not applicable.
Competing Interests
Tunyan Gegham, Khachatryan Levon, Khachatryan Grigor, Hakobyan Gagik declare that they have no competing interests.
References
- Angle E H (1899) Classification of malocclusion. Dent Cosmos 41: 248-264.
- Mackay F, Jones J A, Thompson R, et al. (1992) Craniofacial form in class III cases. Br J Orthod 19: 15-20.
- Tweed CH (1966) Clinical orthodontics. St Louis: Mosby 715-726.
- Moyers R E (1988) Handbook of orthodontics 4th ed Chicago: Yearbook Medical Publishing 183-195.
- Haryani J, Nagar A, Mehrotra D, et al (2016) Management of severe skeletal Class III malocclusion with bimaxillary orthognathic surgery. Contemp Clin Dent 7: 574-578.
- Fox G L, Tilson H B (1976) Mandibular retrognathia: A review of the literature and selected cases. J Oral Surg 34: 53-61.
- de Lir A D, de Moura W L, Oliveira Ruellas A C, et al. (2013) Long-term skeletal and profile stability after surgical-orthodontic treatment of Class II and Class III malocclusion. J Craniomaxillofac Surg 41: 296-302.
- Sato F R, Asprino L, Consani S, et al. (2012) A comparative evaluation of the hybrid technique for fixation of the sagittal split ramus osteotomy in mandibular advancement by mechanical, photo elastic, and finite element analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 114: S60-8.
- Park J U, Baik S H (2001) Classification of angle class III malocclusion and its treatment modalities. Int J Adult Orthodon Orthognath Surg 16: 19-29.
- Benech A, Mazzanti C, Arcuri F, et al. (2011) Simultaneous Le Fort I osteotomy and computer-guided implant placement. J Craniofac Surg 22: 1042-1046.
- Sakar O, Beyli M, Marsan G (2004) Combined prosthodontic and orthodontic treatment of a patient with a Class III skeletal malocclusion: Aclinical report. J Prosthet Dent 92: 224-228.
- Moraschini V, Poubel L A, Ferreira V F, et al. (2015) Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int J Oral Maxillofac Surg 44: 377-388.
- Koji Honda, Makoto Hirota , Toshinori Iwai, et al. (2018) Orthognathic surgery and implant-supported bridge in a class iii patient injured in a motor vehicle accident. J Craniofac Surg 29: e296-e298.
- Bakke M, Holm B, Jensen B L, et al. (1990) Unilateral, isometric bite force in 8-68-year-old woman and men related to occlusal factors. Scand J Dent Res 98: 149-158.
- Rendell J, Grasso J E, Gay T (1995) Retention and stability of the maxillary denture function. J Prosthet Dent 73: 344-347.
- Foltán R, Hoffmannová J, Pavlíková G, et al. (2011) The influence of orthognathic surgery on ventilation during sleep. Int J Oral Maxillofac Surgery 40: 146-149.
- Panula K, Finne K, Oikarinen K (2001) Incidence of complications and problems related to orthognathic surgery: A review of 655 patients. J Oral Maxillofac Surg 59: 1128-1136.
- Westermark A, Bystedt H, von Konow L (1998) Inferior alveolar nerve function after sagittal split osteotomy of the mandible: Correlation with degree of intraoperative nerve encounter and other variables in 496 operations. Br J Oral Maxillofac Surg 36: 429-433.
- Acebal-Bianco F, Vuylsteke P L, Mommaerts M Y, et al. (2000) Perioperative complications in corrective facial orthopedic surgery: a 5-year retrospective study. J Oral Maxillofac Surg 58: 754-760.
- Sakar O, Beyli M, Marsan G (2004) Combined prosthodontic and orthodontic treatment of a patient with a Class III skeletal malocclusion: A clinical report. J Prosthet Dent 92: 224-228.
- Buttke T M, Profitt W R (1999) Referring adult patients for orthodontic treatment. J am Dent Assoc 130: 73-79.
- Williams A C, Shah H, Sandy J R, et al. (2005) Patients’ motivations for treatment and their experiences of orthodontic preparation for orthognathic surgery. J Orthod 32: 191-202.
- Pinho T, Neves M, Alves C (2012) Multidisciplinary management including periodontics, orthodontics, implants, and prosthetics for an adult. Am J Orthod Dentofacial Orthop 142: 235-245.
- Uribe F, Janakiraman N, Nanda R (2013) Interdisciplinary approach for increasing the vertical dimension of occlusion in an adult patient with several missing teeth. Am J Orthod Dentofacial Orthop 143: 867-876.
- Komagamine Y, Kanazawa M, Minakuchi S, et al. (2011) Association between masticatory performance using a colour-changeable chewing gum and jaw movement. J Oral Rehabil 38: 555-563.
- Misch C E, Perel M L, Wang H L, et al. (2008) Implant success, survival, and failure: The International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent 17: 5-15.
- Galindo-Moreno P, León-Cano A, Ortega-Oller I, et al. (2015) Marginal bone loss as success criterion in implant dentistry: beyond 2 mm. Clin Oral Implants Res 26: e28-e34.
- Ellis E, Macnamara J A (1984) Components of adult Class III malocclusion. J Oral Maxillofac Surg 42: 295-305.
- Weissheimer A, Menezes L M, Koerich L, et al. (2015) Fast three-dimensional superimposition of cone beam computed tomography for orthopedics and orthognathic surgery evaluation. Int J Oral Maxillofac Surg 44: 1188-1196.
- Zachary S Peacock, Cameron C Y Lee, Katherine P Klein, et al. (2014) Orthognathic Surgery in Patients Over 40 Years of Age: Indications and Special Considerations 72: 1995-2004.
- Luka Dias Wellar, Leandro Reinhardt, Marcos Antonio Torriani et al. (2013) Combined orthognathic surgery and prosthetic treatment for class III skeletal malocclusion. Stomatos 19: 10-19.
Corresponding Author
Hakobyan Gagik, Professor, Head of Dept. of Oral and Maxillofacial Surgery Yerevan State Medical University after M. Heratsi, Armenia
Copyright
© 2021 Gagik H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.