Gorlin-Goltz Syndrome: A Case Report
Abstract
Nevoid basal cell carcinoma syndrome usually presents as an autosomal dominantly inherited syndrome with variable phenotypic expression. The aim of this study was to report a case of this syndrome based on clinical, radiographic, and histopathological findings. Male patient, 13-years-old, attended the Oral Diagnostic Clinic from State University of Paraiba, complaining of mandible swelling. On physical examination, left facial asymmetry was found, with mandible swelling and inflammatory submandibular lymphadenopathy. The patient also presented polydactyly. Panoramic radiography showed a multilocular well-defined mandibular radiolucency in anterior region. An incisional biopsy was performed, confirming the diagnosis of odontogenic keratocyst. Skull postero-anterior and thorax radiographic images were also performed, with no alterations. The patient was clinically diagnosed as having nevoid basal cell carcinoma syndrome with the presence of odontogenic keratocyst as a major criterion and the following minor criteria: Polydactyly, hypertelorism, Sprengel anomaly, deformed chest and prominent frontal bossing. The patient was referred to the physician for evaluation. Nevoid basal cell carcinoma syndrome has several distinct clinical characteristics and careful investigation is important, especially using imaging tests as complementary exams.
Keywords
Nevoid basal cell carcinoma syndrome, Gorlin syndrome, Odontogenic keratocyst
Introduction
Nevoid basal cell carcinoma syndrome (NBCCS), also known as Gorlin-Goltz syndrome or Gorlin Syndrome, usually presents with dominant autosomal heritage, with variable phenotypic expression. It is usually caused by mutations in the Patched Tumor Suppressor (PTCH1) gene, located in chromosome 9q [1,2]. The mutation usually affects the germ cells resulting in vertical transmission but in as many as 40% of cases, the mutation affects somatic cells, and the syndrome occurs sporadically without other family members affected. NBCCS was described in 1960 by Gorlin and Goltz [3], who established the classic triad: Multiple nevoid basal cell carcinomas (NBCC), multiple odontogenic keratocyst [4,5] and bifid ribs [6,7].
The syndrome can be diagnosed only when the first signs and symptoms appear [8]. The presence of multiple odontogenic keratocysts in the jaws is very common [9], and may be the first and unique manifestation [10,11], being highly suggestive of the syndrome, even in the absence of other manifestations [12,13].
In addition, this syndrome is a condition that has a predisposition to cancer, being of fundamental importance to diagnose it as early as possible. Careful clinical examinations and imaging tests are of great value as a diagnostic aid [11].
The first health care professional to come into contact with the patient may be the dental surgeon, due the presence of swelling on the face resulting from the keratocysts in the jaws [10,11]. So, this study aimed to report a case with unusual clinical manifestations in a young patient with NBCCS.
Case Presentation
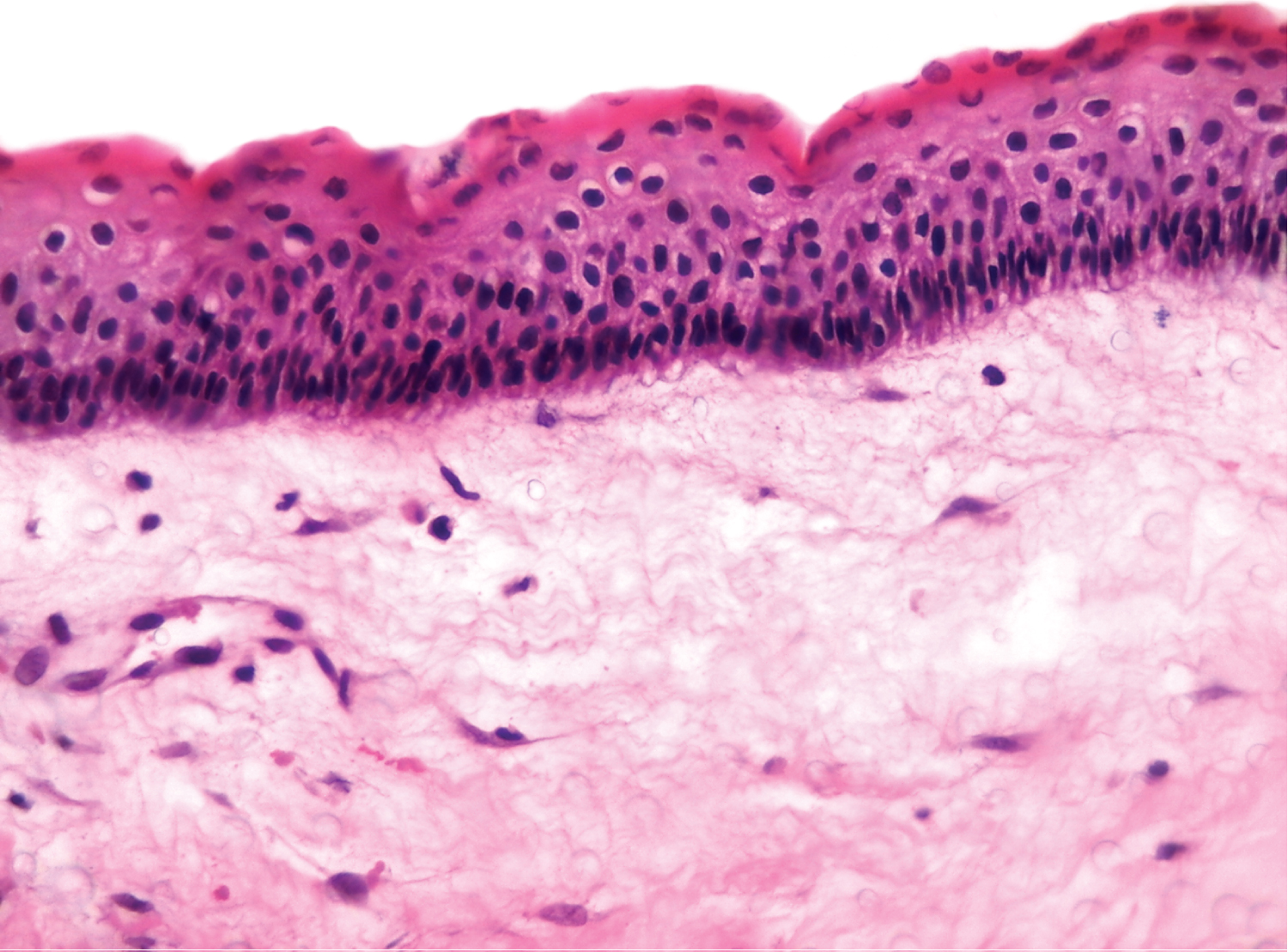
A 13-years male patient attended the Oral Diagnostic Clinic from Campus VIII of the State University of Paraiba (UEPB), complaining of swelling in the mandible (Figure 1). The extra-oral physical examination found left facial asymmetry with localized mandible swelling on the left side and inflammatory submandibular lymphadenopathy. The patient also had polydactyly of the hands and feet (Figure 2). Sprengel anomaly was also found (Figure 3) and chest deformation. Basal cell carcinomas were not seen on the skin. The intraoral physical examination showed swelling in anterior region of the mandible, painless on palpation and with dental malposition (Figure 4). Panoramic radiography revealed a well-defined multilocular radiolucent lesion in anterior region of the mandible (Figure 5). An incisional biopsy confirmed the diagnosis of odontogenic keratocyst (Figure 6). Postero-anterior radiographies of the skull and the thorax were performed, and these did not show any notable changes such as calcification of falx cerebri and bifid ribs, or other bony anomalies typical of the syndrome. The patient was clinically diagnosed with NBCCS based on a keratocyst as a major criterion and the presence of five minor criteria: Sprengel anomaly (congenital scapular elevation), polydactyly, deformed chest, hypertelorism and prominent frontal bossing. The patient underwent surgical decompression and subsequent enucleation of the lesion and is being followed up by the Clinic team. The person responsible for the patient signed the Informed Consent Form when filling out the patient's medical record.
Discussion
NBCCS is a rare syndrome with large phenotypic heterogeneity which makes it difficult to diagnosis. More than 100 different clinical manifestations have been reported which include skeletal, craniofacial, neurological, oropharyngeal, dermal, sexual, ophthalmic, and cardiac abnormalities [14-16].
The diagnosis is clinical and based on specific characteristics, requiring the presence of two major criteria (odontogenic keratocyst, nevoid basal cell carcinoma, palmoplantar pits), or a major criterion with two minor [1,17], or a major criterion associated with a minor one. Minor criteria include macrocephaly, congenital malformations, ocular and skeletal abnormalities, radiographic changes, among others. The syndrome should also be considered if there is a major criterion and a molecular confirmation. Gene mutation analysis confirms the diagnosis [18]. Although the patient in the present case had only one large odontogenic keratocyst in mandible (major criterion), he had other minor criteria such as Sprengel anomaly (congenital elevation of the scapula with rotation toward the spine with scoliosis), polydactyly in the hands and feet, prominent frontal bossing, hypertelorism and chest deformity (Pectus Excavatum).
Among the major criteria, the presence of multiple keratocysts (affecting 74% [1] to 90% [16] of the patients) and calcification of falx cerebri is also quite prevalent [7,9,11,16,19], in addition to palmoplantar pits [17]. The patient in the present case presented with one large keratocyst in the mandible with a multilocular pattern. Keratocysts in syndromic patients can present, on average, five per patient, in addition to a higher recurrence rate after enucleation compared to non-syndromic patients. Because of this, it is recommended follow- up for a long period (annually for five years and biannually, for the entire life of the patient) [7,11,20]. Khaliq, et al. [11] when evaluating seven syndromic patients, found that all had multiple keratocysts as the first manifestation of the syndrome, most of which were located in the mandible (77%), in an unilocular pattern (71%), associated with teeth (88%). As treatment, the patient of the present case initially received a conservative approach (cystic decompression), due to the large extent of the lesion, followed by enucleation, the most common treatment for keratocysts [21].
However, despite being prevalent major criterion, the patient of this case did not present palmoplantar pits, but he was alerted to their appearance and the possibility of malignant transformation into nevoid carcinomas [1]. In addition, he was referred to the dermatologist for evaluation. Often the basal cell carcinomas of the skin in these patients are the most challenging to manage and produce the most morbidity. The Posterior-Anterior (PA) radiography of the patient's skull did not demonstrate calcification of falx cerebri, although this is the most frequent radiographic alteration found in syndromic patients [2,15]. All syndromic patients evaluated by Santos, et al. [16] and by Khaliq, et al. [11] presented calcification of falx cerebri.
Among the most prevalent minor criteria of the syndrome are the presence of skeletal anomalies, especially in the ribs [13,17]. However, the evaluation of chest radiography did not show any noticeable changes in the ribs of the patient.
Because NBCCS is a hereditary condition, genetic counseling is mandatory in order that family members, especially children, can be genetically tested or followed. For this, radiographic exams, which have a low cost, must be used [14]. As the syndrome is of autosomal dominant inheritance, offspring have 50% risk of being affected [1,14,22]. However, some syndromic patients can present a new spontaneous mutation [23,24], with no history of an affected family member [15]. In the present case, it was not possible to assess the rest of the patient's family.
As the treatment is multidisciplinary, the early referral of the patient to other professionals is essential for the diagnosis of other changes and possible interventions. The patient must be followed up by different specialists, especially dermatologists, due to his high predisposition to basal cell carcinomas and neoplasms [25]. Carcinomas associated with the syndrome are diagnosed often in young patients (mean 25-years-old), in unexposed areas of the body [1,7].
However, due the relative rarity and phenotypic variability, this syndrome is usually diagnosed late [26]. Our 13-year-old patient had earlier indications of the syndrome, such as polydactyly, Sprengel anomaly, prominent frontal bossing and hypertelorism, but it was only due to the swelling in the face that the family sought the health professional and the final diagnosis of NBCCS was confirmed.
This case presents an alert to dentists that, the NBCCS should at least be considered in any patient with a biopsy proven odontogenic keratocyst, and the patient should be examined for other features of the syndrome as well as family history of jaw cysts. If other major or minor criteria are present, referral to other specialists would be in order to document as soon as possible other features of the syndrome that could lead to a more definitive diagnosis.
Final Considerations
NBCCS presents well-defined clinical criteria for its diagnosis and the performance of molecular tests is indicated only in a few particular cases, due to its high cost. A helpful complementary diagnostic tool of great importance is the imaging tests that are relatively inexpensive but are critical to discover the keratocyst.
References
- VE Kimonis, Goldstein AM, Pastakia B, et al. (1997) Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndrome. Am J Med Genet 69: 299-308.
- Lo Muzio L (2008) Nevoid basal cell carcinoma syndrome (Gorlin syndrome). Orphanet Journal of Rare Diseases Dis 3: 32.
- Gorlin RJ, Goltz RW (1960) Multiple nevoid basal-cell epithelioma, jaw cysts and bifid rib. A syndrome. N Engl J Med 5: 908-912.
- Speight P, El-Naggar AK, Chan JK , et al. (2017) Odontogenic keratocyst. In: El-Naggar AK, Chan JK, Grandis JR, Takata T, Slootweg PJ. World Health Organization classification of head and neck tumours. (4th edn), IARC, Lyon 235-236.
- Stoelinga PJW (2019) Keratocystic odontogenic tumour (KCOT) has again been renamed odontogenic keratocyst (OKC). Int J Oral Maxillofac Surg 48: 415-416.
- Tarnoki AD, Tarnoki DL, Kiss KK, et al. (2014) Unusual cortical bone features in a patient with Gorlin-Goltz syndrome: A case report. Iran J Radiol 11: e5316.
- Thomas N, Vinod SV, George A, et al. (2016) Gorlin-Goltz syndrome: An often missed diagnosis. Ann Maxillofac Surg 6: 120-124.
- Guo Y-Y, Zhang J-Y, Li X-F, et al. (2013) PTCH1 gene mutations in keratocystic odontogenic tumors: A study of 43 Chinese patients and a systematic review. PLoS One 8: e77305.
- Pol CA, Ghige SK, Kalaskar RR, et al. (2013) Gorlin-Goltz syndrome: A rare case report. Contemp Clin Dent 4: 547-550.
- Pereira T, Tamgadge A, Sapdhare S, et al. (2015) Multiple keratocystic odontogenic tumors in nevoid basal cell carcinoma syndrome. Ann Maxillofac Surg 5: 277-280.
- Ul Khaliq MS, Shah AA, Ahmad I, et al. (2016) Keratocystic odontogenic tumors related to gorlin-goltz syndrome: A clinicopathological study. J Oral Biol Craniofac Res 6: 93-100.
- Hashmi AA, Edhi MM, Faridi N, et al. (2016) Multiple keratocystic odontogenic tumors (KCOT) in a patient with gorlin syndrome: A case report with late presentation and absence of skin manifestations. BMC Res Notes 9: 357.
- Pachowicz M, Staskiewicz G, Opielak G, et al. (2017) Complex rib anomalies in patient undergoing PET/CT study: A case report. Nuclear Medicine Review 20: 64-65.
- Acharya S, Panda S, Dhull KS, et al. (2013) Gorlin syndrome with bilateral polydactyly: A rare case report. Int J Clin Pediatr Dent 6: 208-212.
- Chen JJ, Sartori J, Aakalu VK, et al. (2015) Review of ocular manifestations of nevoid basal cell carcinoma syndrome: What an Ophthalmologist needs to know. Middle East Afr J Ophthalmol 22: 421-427.
- Santos TS, Vajgel A, Martins-Filho PRS, et al. (2016) Nevoid basal cell carcinoma syndrome: A long-term study in a family. Craniomaxillofac Trauma Reconstr 9: 94-104.
- Evans DG, Ladusans EJ, Rimmer S, et al. (1993) Complications of the nevoid basal cell carcinoma syndrome: Results of a population based study. J Med Genet 30: 460-464.
- Bree AF, Shah MR, BCNS Colloquium Group (2011) Consensus statement from the first international colloquium on basal cell nevus syndrome (BCNS). Am J Med Genet A 155A: 2091-2097.
- Manjima S, Naik Z, Keluskar V, et al. (2015) Multiple jaw cysts-unveiling the gorlin-goltz syndrome. Contemp Clin Dent 6: S102-S105.
- Kamil AH, Tarakji B (2016) Odontogenic keratocyst in children: A review. Open Dent J 10: 117-123.
- Diaz-Belenguer A, Sanchez-Torres A, Gay-Escoda C (2016) Role of Carnoy's solution in the treatment of keratocystic odontogenic tumor: A systematic review. Med Oral Patol Oral Cir Bucal 21: e689-e695.
- Bala Subramanyam S, Naga Sujata D, Sridhar K, et al. Nevoid basal cell carcinoma syndrome: A case report and review. J Maxillofac Oral Surg 14: 11-15.
- Durmaz CD, Evans G, Smith MJ, et al. (2018) A novel PTCH1 frameshift mutation leading to nevoid basal cell carcinoma syndrome. Cytogenet Genome Res 154: 57-61.
- Zhou J, Zhang G, Shi M, et al. (2019) A novel splicing mutation of PTCH1 in a chinese family with nevoid basal cell carcinoma syndrome. Med Mol Morphol 52: 235-237.
- NK Kiran, Tilak Raj, Mukunda, et al. (2012) Nevoid basal cell carcinoma syndrome (gorlin-goltz syndrome). Contemp Clin Dent 3: 514-518.
- Fini G, et al. (2013) Nevoid basal cell carcinoma syndrome (Gorlin-Goltz syndrome): Case report. G Chir 34: 176-179.
Corresponding Author
Sandra Aparecida Marinho, State University of Paraiba (Universidade Estadual da Paraiba-UEPB), Rua Cel Pedro Targino sn. Centro, Araruna, PB 58233-000, Brazil, Tel: 55-83-3373-1040
Copyright
© 2021 Carvalho SHG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.