Improving the Care Accuracy of Nurses Caring for Allogeneic Arm-Transplant Patients
Abstract
Purpose: The aim of this project is to improve the correct rate of nurse’s knowledge and skill about hand allotransplantation post-operative care.
Resolutions: The intervention includes holding education, revising hand allotransplantation care standards, making drug charts, situational simulation treadmill exercises, and post-operation care videos.
Background & Problems : If the nurse lacks the ability to care the all, the success rate of the hand allotransplantation may be affected, resulting in related complications.
Results: After improvement through the project, the nurse’s knowledge about allotransplantation increased to 91.3%, and the nurse accuracy rate increased to 98%.
Keywords
Allotransplantation, Post-operation, Nursing
Introduction
As the hands play an important role in work and self-care, all severe hand disabilities due to trauma, work accidents, burns and scalds, and disease will severely affect patients’ physical and mental self-image and quality of life. Despite advances in technology and many available prosthetic options, traditional prostheses are still cumbersome and unwieldy. The appearance, fine movements, and sensation provided by a modified prosthesis differ significantly from those of a hand [1]. For this reason, allogeneic arm transplantation is an important option.
An allogeneic arm transplant aims to provide a new arm to replace a disabled arm. In 1998, a team led by Professor Dubernard in Lyon, France completed the world’s first successful allogeneic arm transplantation [2]. Since then, more than 113 such surgeries have been performed worldwide [1]. Hand-transplantation surgeries are taking off in Taiwan. To date, 6 allogeneic arm transplantations have been carried out successfully on 5 patients. Such operations involve many postoperative care precautions and therefore require an interdisciplinary team and highly integrated co-therapy to achieve complete care. The care capabilities of nurses become more important in this context and the department that cares for allogeneic arm-transplant patients is the first-line plastic-surgery ward. The first case in our hospital was carried out in 2016. The allogeneic arm-transplant team organized an education and training course. In 2019, our hospital team completed two allogeneic arm-transplantation cases. Due to a three-year gap and the low number of cases, the ward staff had insufficient care knowledge, competency, and familiarity. As this situation could have affected the survival rate of the transplanted arm, it motivated our group to improve care quality after the allogeneic arm transplantation.
Current Status Analysis
Department overview
Our department is a combined plastic surgery, general surgery, and gastroenterological surgery ward. Between 2016 and 2019, the plastic-surgery unit had 33 beds and the general and gastroenterological surgery department had 5 wards. The staff composition was as follows: 1 head nurse and 21 nurses, with 7.9 mean years of work experience; 14 staff members had more than 5 years of work experience, and 7 staff members had fewer than 5 years of work experience. The staff titles were: N: 3 people, N1: 1 person, N2: 11 people, and N3: 6 people. The manpower allocation was as follows: 6–7 staff members cared for an average of 7–8 patients; 3–4 staff members covered the night shift and 3 staff members worked the graveyard shift, caring for an average of 12–13 patients. Between 2016 and 2019, a total of 3 patients who underwent allogeneic arm-transplantation surgery were cared for by the team; of these, 2 had surgery at our hospital. The allogeneic arm-transplant team only provided 2 continuing-education courses (in 2016 and 2019). The department staffs were first-line staff members, who assisted with immediate postoperative care.
Current status of postoperative nursing care following allogeneic arm transplantation
After their conditions stabilized after surgery, the allogeneic arm-transplant patients were transferred from the intensive-care unit to a single-bed ward. In 2016–2019, the department nurses cared for 2 allogeneic arm-transplant patients (the most recent case was in November 2019). As the interval following the last patient cared for was 3 years, staff members had little actual postoperative clinical-care experience and few relevant care-training classes were provided. Most of the care methods were delivered based on the verbal instructions of experienced nurses. The various postoperative nursing evaluations and measures were referenced from other transplantation-care standards in the hospital, such as liver-transplantation standards. However, these standards did not include methods for evaluating skin rejection; in addition, the postoperative drugs and dosing times were completely different. This shows that current transplantation-care standards do not meet the needs of allogeneic arm-transplantation patients.
To understand staff methods of acquiring knowledge about allogeneic arm transplantation, our project team designed a Google questionnaire in July 2021. Two members of the team designed the questionnaire content, selecting open-ended questions and multiple response options. Nineteen nurses were investigated to determine why they were unfamiliar with allogeneic arm transplantation. The multiple-choice questionnaire had 6 questions; the results showed that 10 subjects (52.6%) had not undertaken any relevant courses or periodic audits of their allogeneic arm-transplant-related knowledge and competency; 8 (42.1%) did not care for allogeneic arm-transplant patients; 6 (31.6%) did not have training in allogeneic arm-transplant care standards and had no health-education forms; 6 (31.6%) had no models or videos to use as a reference; and 6 (31.6%) had treated fewer than 6 cases. As the department had never developed postoperative-care standards or health-education forms, no models or videos were available for colleagues to learn from; as a consequence, 8 colleagues lacked any relevant postoperative clinical experience. For this reason, postoperative care knowledge and competency were narrated and taught by experienced nurses.
Awareness of postoperative care for allogeneic arm transplantation in nurses
To understand the staff members’ level of awareness of allogeneic arm-transplant postoperative care, the project team consulted attending physicians, resident physicians, nurse practitioners, and head nurses from the plastic-surgery department in February 1–10, 2021 to ascertain their opinions. A 20-item “allogeneic arm-transplant postoperative-care awareness questionnaire” was formulated to measure the awareness of nurses. The questionnaire included 10 true/false questions and 10 multiple-choice questions. A correct answer was assigned 5 points and 100 points were full marks. From February 22 nd to 28 th , the project team used the “allogeneic arm-transplant-awareness questionnaire” to investigate the awareness of 19 nurses in the department (excluding 2 members of the project team). The results showed 68.2% awareness accuracy, with 12 questions having less than 80% accuracy. The three questions with the lowest accuracy levels were Question 9 (Do you draw blood 30 minutes before administration to measure the peak Prograf and Certican concentrations?) for which the accuracy level was only 10.5%; Question 7 (88% of patients will develop rejection during the first 30 days and we should administer antibiotics and increase the immunosuppressant dose when skin inflammation or necrosis and fever occurs) for which the accuracy level was 21.1%; and Question 1 (According to medical orders, a water-soluble povidone-iodine solution and physiological saline are used to disinfect the transplanted arm every day before an aseptic dressing change is performed) for which the accuracy level was 31.6%. The above results show that the nurses had insufficient understanding of postoperative care for allogeneic arm-transplantation patients. The details are presented in Table 1.
Nurses’ current allogeneic arm-transplantation postoperative-care competency
In order to understand the nurses’ current allogeneic arm-transplantation postoperative-care competency, the project team consulted experts and invited a transplantation team, including the attending physicians, pharmacists, nurse practitioners, and head nurses from the plastic-surgery department to attend in March 1–15, 2021 to formulate the “allogeneic arm-transplant postoperative-care accuracy” evaluation form. The form contained 5 major categories, namely rejection evaluation, circulation evaluation, drugs, infection-control measures, and other, divided into 29 questions. A score of 1 point was assigned for every correct answer; 0 was assigned for a form not implemented or an implementation error. Between June 15 th and 30 th , 2021, 19 staff members (excluding 2 people in the project group) were audited on their allogeneic arm-transplantation postoperative care. In each evaluation, the same member conducted a one-to-one simulated scenario assessment. The scenarios were as follows: 1. Creating normal skin-color photographs and abnormalities after allogeneic arm-transplantation surgery, such as rejection phenomena or rashes, for peer evaluation; 2. Creating cards of common anti-rejection drugs (including the dose, effects, and side effects) for patients after allogeneic arm-transplantation surgery; the cards were for use by colleagues to deepen their understanding of drugs; 3. For infection control, the team members prepared single-bed wards. The preparation items included beds, a weighing machine, scales, a physiological monitor, a nursing trolley, a dressing-change trolley, and disinfectants. Alcohol, a used-a clothes bucket, a sterile surgical gown, gloves, a cap, and a dustproof mat were prepared outside the ward so that colleagues could gown up for the actual operation before entering the ward; 4. An allogeneic arm-transplantation-care evaluation form was prepared. The evaluation content included skin color, temperature, capillary-filling time, Doppler, and SPO2. 5. Three scenario questions were designed to help colleagues determine how to evaluate and notify others when abnormalities occurred during allogeneic arm transplantation. The results showed a mean care accuracy of (67.7%). Questions with low accuracy included dressing-change preparations for allogeneic arm-transplant patients (10.5%); the evaluation of rejection phenomena (15.8%); the side effects of Cellcept (15.8%), and the evaluation of urine volume and color change in patients (21.1%). From the above results, it can be seen that the nurses had low accuracy in postoperative care for allogeneic arm-transplantation patients.
Factors affecting nurses’ accuracy in postoperative care for allogeneic arm-transplantation patients
To understand the reasons for these low levels of accuracy in allogeneic arm-transplantation postoperative care, the project team designed a Google questionnaire on potential factors influencing allogeneic arm-transplantation postoperative care accuracy from July 13 to 17, 2021. The questionnaire contained 6 open-ended multiple-choice questions. Overall, 19 questionnaires were collected. The results revealed the following reasons for the nurses’ low levels of allogeneic arm-transplantation postoperative care accuracy: Did not take relevant courses (n = 10, 52.6%); did not periodically audit allogeneic arm-transplantation care-related knowledge and accuracy (n = 10, 52.6%); never cared for allogeneic arm-transplant patients before (n = 8, 42.1%); A lack of allogeneic arm-transplantation care standards and health-education leaflets in the department (n = 6, 31.6%); and the low number of allogeneic arm-transplant patients (n = 6, 31.6%). This shows that many nurses had not taken continuing-education courses and lacked actual experience. In addition, they did not have access to a periodic audit of hand transplantation care-related knowledge and care accuracy.
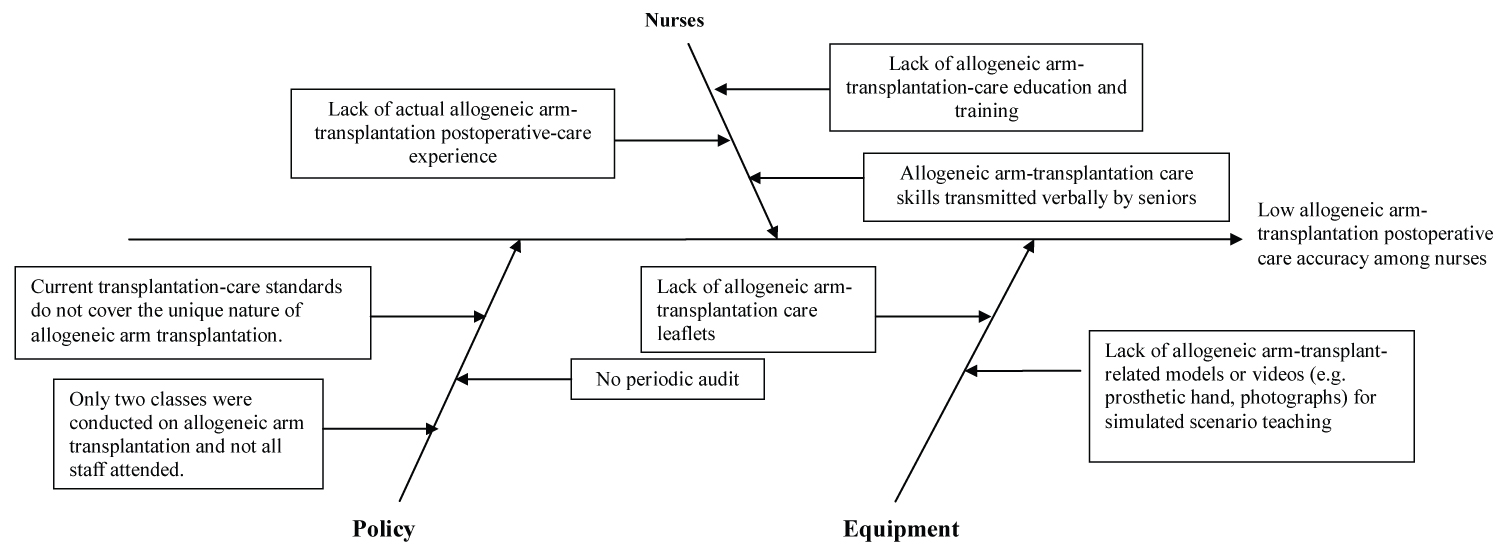
Determining Problems and Causes
In summary, the main causes of low-level allogeneic arm-transplantation postoperative-care accuracy were personnel related: allogeneic arm-transplantation postoperative-care skills were transmitted verbally by senior nurses; there was a lack of allogeneic arm-transplantation postoperative-care education and training; nurses also lacked actual allogeneic arm-transplantation postoperative-care experience. In relation to policy, only two classes were held to teach allogeneic arm-transplantation; current transplantation-care standards did not cover the unique nature of allogeneic arm transplantation. There were no periodical audits of allogeneic arm-transplantation postoperative-care accuracy. In terms of equipment, there were no allogeneic arm-transplantation models or videos for simulated scenario learning or allogeneic arm-transplantation postoperative-care leaflets. A plot of characteristic causes was created based on the above data (Figure 1).
Purpose of this project
To increase the accuracy of allogeneic arm-transplantation care awareness from 68.2% to 90%.
Target setting = accuracy of allogeneic arm-transplantation-care awareness before improvement + (accuracy of allogeneic arm-transplantation-care inaccuracy before improvement x competency of team members) = 68.2% + (31.8% x 70%) = 90.5%
To increase the accuracy of allogeneic arm-transplantation-care execution from 67.7% to 90%.
Target setting = accuracy of allogeneic arm-transplantation-care execution before improvement + (accuracy of allogeneic arm-transplantation-care execution before improvement x competency of team members) = 67.7% + (32.3% x 70%) = 90.3
Literature Review
Key aspects of allogeneic arm-transplantation patient care and nursing
Allogeneic arm-transplantation surgery is relatively precise, complex, and time-consuming [3]. For this reason, the care capabilities of nurses are more important after a successful surgery. The literature points out that 80% of transplant patients develop at least one rejection reaction after surgery [4]. Nurses must therefore be able to identify acute rejection at an early stage by knowing how to observe skin changes, including erythema and papules, alopecia, desquamation, and other clinical characteristics of acute rejection reaction. Postoperative inhibition of rejection reaction requires lifetime immunosuppressant treatment. As there are many types of immunosuppressants and precautions, dosing times and contraindications should be strictly adhered to. After hand-transplantation surgery, the transplanted arm must be disinfected with 75% alcohol before undergoing an aseptic dressing change every day; the skin color, tension, capillary-filling response, skin temperature, blood oxygen, and Doppler monitoring of circulation in the transplanted arm must be closely monitored [5]. Nurses must understand the need to ensure infection-prevention measures, provide guidance on avoiding raw foods, use soft brushes, carry out aseptic techniques accurately, and adopt stringent protective-isolation measures [6]. Microvascular surgery will damage the vascular endothelium, causing platelet aggregation and thrombosis. The first 3–5 days after microvascular surgery is when thrombosis tends to occur. After thrombosis occurs, circulation must be reestablished within 2 hours to be able to save the graft [6]. Therefore, nurses must have the ability to identify venous/arterial thrombosis and warn the physician to arrange for surgery within the golden hour.
Strategies for improving care accuracy among nurses caring for allogeneic arm-transplant patients
As the 48 hours after allogeneic arm-transplantation surgery constitute a critical period, improved knowledge due to nursing education and training must match clinical application. Hybrid courses must therefore be used, with knowledge, skills, and practice as their goals. Lectures, practical workshops, and simulations can provide integrated training to integrate knowledge and skills with clinical applications [5]. Hybrid courses include: (1) Traditional teaching, which mostly includes lectures. Usually, the teacher will use slides and handouts to teach professional knowledge and skills in an organized and systematic manner [7]. (2) Theory and application in workshops. In this type of practical teaching, an experienced lecturer guides a small group of 10–20 people to examine a theme [8]. (3) Simulation training, in which scenario simulations are used to mimic actual clinical scenarios. Students can repeatedly practice in a realistic, safe, and interactive learning environment, while ensuring patient safety and improving medical quality. This method can be used to train personnel of various grades from different domains, including resident physicians, nurses, and medical teams. Scenario simulation is employed for training, as it strengthens knowledge, improves skills, and cultivates teamwork [9].
The content of standard operating procedures was developed to be used as a reference by staff members during operations. In comprehensive quality management, there is a particular emphasis on standardizing care procedures; standardized procedures allow staff members to communicate easily, provide a basis for execution; they can also improve operation quality [10].
Solutions
Solutions were classified based on their feasibility, importance, and effectiveness. The decision matrix was used and 6 people (team members, the head nurse, and 3 nurse practitioners) evaluated solutions using a 5-point standard, with 5 points indicating the highest feasibility and effectiveness, 3 points indicating moderate results, and 1 point indicating low feasibility and poor results. The maximum score was 90 points and strategies achieving 70% (63 points) were selected. Table 3 presents the decision-matrix analysis.
Execution Process
Scheduled period (July 19, 2021 to August 20, 2021)
After the decision analysis, the solutions included formulating allogeneic arm-transplantation care standards and a monitoring plan, planning continuing-education courses, making cards to identify drugs, and arranging workshop simulations.
The project team formulated allogeneic arm-transplantation care standards and a monitoring plan after the literature review and references to liver-transplantation care standards in the hospital. The contents included allogeneic arm-transplantation postoperative protective-isolation measures, dietary precautions, allogeneic arm-transplant rejection and circulation-evaluation methods, immunosuppressant and postoperative medication precautions and health education. Images and textual annotations were used to help colleagues design monitoring plans based on allogeneic arm-transplantation care standards; in addition, the execution accuracy of all nurses was to be monitored every 6 months.
Allogeneic arm- transplantation continuing-education courses were scheduled between July 26 and August 20, 2021. Attending physicians, head nurses, nurse practitioners, and pharmacists from the plastic-surgery department were consulted. The contents included protective-isolation measures, postoperative dietary precautions, transplanted-arm rejection and circulation-evaluation methods, immunosuppressants, and other postoperative medications. Each class lasted 30–40 minutes and was supplemented by case discussions and question-and-answer sessions. In addition, simulated scenarios were designed as actual operations for colleagues. Allogeneic arm-transplantation care videos were recorded. The videos lasted 10 minutes and their contents included room preparation, transplanted-arm rejection, and circulation evaluation. These videos were used for revision. Drug-identification cards were also produced to help staff members recognize immunosuppressants.
Execution period (August 23, 2021 to September 30, 2021)
The head nurse helped to present the allogeneic arm-transplantation postoperative-care standards to colleagues. At 8:00–8:30 a.m. on August 25 th and on the mornings of September 6 th and 15 th , the project-team members explained the importance of allogeneic arm-transplantation care and the current status-analysis information so that colleagues could understand the results.
Throughout September 22–28, 2021, two allogeneic arm-transplantation-care training classes were conducted in the mornings. In one class, the pharmacist described medications used after allogeneic arm-transplantation surgery. Another class, designed by the project team, covered allogeneic arm-transplantation postoperative-room preparation, self-protection and related infection-control measures, and postoperative dietary-health education. It described allogeneic arm-transplantation rejection and circulation and transplanted arm-wound dressing changes. Afterwards, 10 minutes’ worth of videos on allogeneic arm-transplantation rejection and evaluation techniques were played for colleagues to practice, deepening their understanding. The course lasted around 40 minutes. Overall, 19 colleagues participated and the attendance rate was 100%. During the course, colleagues asked whether allogeneic arm-transplant patients had to drink distilled water or whether boiled tap water could be used, as in the case of liver-transplantation patients. To answer these questions, the project team searched the literature and found that tap water tends to contain cryptosporidium, Giardia lamblia, bacteria, and E. coli and cannot be drunk without treatment by transplant recipients. However, boiling can remove cryptosporidium and other aqueous-medium pathogens. Alternatively, filtered or boiled drinking water can be used as substitutes; however, the filters must be effective and the bottled water must be high-quality. After a discussion with the physician, drinking water was changed to sterile distilled water or boiled tap water, a guideline accepted by our colleagues.
On September 6 th , cards detailing allogeneic arm-transplantation postoperative-care standards and immunosuppressant-recognition information were placed in the nursing station for reference. However, there was no actual case that could be used as a reference by participants. The project team therefore invited colleagues to a simulation on September 28–30 to practice postoperative care, based on allogeneic arm-transplantation postoperative-care standards; the experience was evaluated and doubts were clarified. Each session lasted 10–15 minutes; participants felt that this simulation helped them better understand allogeneic arm-transplantation postoperative room-preparation methods and items and the steps for evaluating allogeneic arm-transplantation rejection and circulation; the response was good.
Evaluation period (October 1–29, 2021)
Between October 1 st and 29 th , 2 members of the project team evaluated the allogeneic arm-transplantation care awareness and accuracy of nurses, based on the allogeneic arm-transplantation care awareness and accuracy evaluation form. 19 nurses were audited on the questions and simulation scenarios.
Results
Between October 1 st and 29 th , 2021, the allogeneic arm-transplantation postoperative-care-awareness questionnaire was used to investigate the awareness accuracy of staff members. The results showed that care accuracy had risen to 91.3%, an improvement of 23.1%, compared with 68.2% before improvement. This shows that the allogeneic arm-transplantation-care courses significantly increased nurses’ allogeneic arm-transplantation postoperative-care awareness. The Following a project-team discussion, an allogeneic arm-transplantation care-evaluation form was designed, based on a skin-flap evaluation form from the plastic-surgery department. In addition, videos on key aspects of allogeneic arm-transplantation care were recorded and actual simulations were employed. This significantly improved the participants’ allogeneic arm-transplantation care knowledge.
From October 13 th to 29 th , the project team used the allogeneic arm-transplantation care-accuracy form and one-to-one simulation scenarios to determine the competency of the 19 nurses. In the results, their accuracy improved from 67.7% to 98%, an improvement of 30.3%. The details are shown in Table 2.
Conclusion and Discussion
In this project, a current status analysis found that nurses had low allogeneic arm-transplantation-care accuracy. Continuing-education courses were conducted and allogeneic arm-transplantation care standards were revised. These measures significantly improved the allogeneic arm-transplantation care awareness and care accuracy of nurses. The timely completion of this project relied on the cooperation of colleagues and expert opinions. The persistence of team members provided the greatest assistance; they searched the literature when questions were asked during implementation. Papers were found to change the original transplantation-care standards and sterile distilled water was no longer provided for patients to drink. This made caring easier without affecting the patient. To maintain the nurses’ allogeneic arm-transplantation postoperative care accuracy, this item was listed a core quality-audit item for the department; monitoring will now be carried out once every 6 months. In addition, the inspection and review results will be presented in every departmental meeting. Newly employed staff members will undergo training courses. Every year, the awareness of staff members in the department will be assessed to ensure that they understand the importance of allogeneic arm-transplantation care.
To maximize the benefits of this project, allogeneic arm-transplantation care simulations were arranged during the execution process. They covered allogeneic arm-transplantation postoperative-room preparation, self-protection and other related infection-control measures, postoperative dietary-health education, allogeneic arm-transplantation rejection and circulation evaluations, transplanted-arm wounds, dressing changes, and videos on allogeneic arm-transplantation rejection and circulation evaluation techniques. The group believes that this project is innovative and can be promoted for other transplantation surgery departments.
The project execution had the following limitations. Simulations were used to assess allogeneic arm-transplantation care accuracy. As there were few cases and many variables and patient gender had to be considered in clinical practice, simulation scenarios were used for practice and assessment; an actual situation audit could not be performed. The greatest contributions of this project are as follows: it provides video CDs on allogeneic arm-transplantation care skills for newly employed staff members; allogeneic arm-transplantation care is covered in annual mandatory courses; there are periodic audits of staff competency; and basic-care evaluation standards have been established. Many factors affect the postoperative success rate and complications of allogeneic arm-transplantation patients. Allogeneic arm-transplantation care-evaluation accuracy is just one of the factors affecting postoperative effectiveness—and not a direct influence. Allogeneic arm transplantation requires joint postoperative care by a multidisciplinary team; nurses must help to provide maximum care for arm rehabilitation after surgery. In future, we recommend incorporating the professional knowledge and skills of various specialists, including rehabilitation and occupational therapists, physiotherapists, nutritionists, psychologists, social workers, and case managers, to achieve greater effectiveness.
Conclusion
The project was effective improved the quality of allotransplantation care. The nurse knowledge and ability have been significantly improved, and the operation has achieved better results.
References
- Salminger S, Roche A D, Sturma A, et al. (2016) Hand transplantation versus hand prosthetics: Pros and cons. Curr Surg Rep 4: 8.
- Dubernard J, M Owen, E Herzberg, et al. (1999) Human hand allograft: Report on first 6 months . Lancet 353: 1315-1320 .
- Kuo YR (2017) Allotransplantation creates new field of medicine. Kaohsiung Medical University Institutional Repository, 36: 4.
- Alolabi N, Augustine H, Thoma A (2017) Hand transplantation: Current challenges and future prospects. Transplant Research and Risk Management 9: 23- 29.
- Avery RK, Michaels MG, AST Infectious Diseases Community of Practice (2019) Strategies for safe living following solid organ transplantation-Guidelines from the American society of transplantation infectious diseases community of practice. Clin Transplant 33: e13519.
- Shores JT, Malek V, Lee WPA, et al. (2017) Outcomes after hand and upper extremity transplantation. J Mater Sci Mater Med 28: 72.
- Chu YC, Chang KC, Hsu LC, et al. (2015). Hybrid Technical Training Curriculum. Taiwan Society for Simulation in Healthcare 2 : 32-38.
- Yang CW (2015) Application of medical simulation in clinical skills training. Formos J Med 19: 365-362.
- Chen SF, Wei HF, Hsieh HF, et al. (2018) A project to improve the integrity of cold cap therapy in nursing staff of neonatal intensive care unit. Tzu Chi Nurs J 17: 89-100.
- Salminger S, Sturma A, Roche AD, et al. (2016) Functional and psychosocial outcomes of hand transplantation compared with prosthetic fitting in below-elbow amputees: A multicenter cohort study PLOS ONE 11: e0162507.
Corresponding Author
Tsai-Rung, LIN, Kaohsiung Medical University, 100, Shin-Chuan 1st Road, Kaohsiung 80708, Taiwan, Tel: 886-7-3121101; ext.7481.
Copyright
© 2023 Tsai-Rung LIN, et al. This This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.