Improving Oral Health in Pediatric Primary Care
Abstract
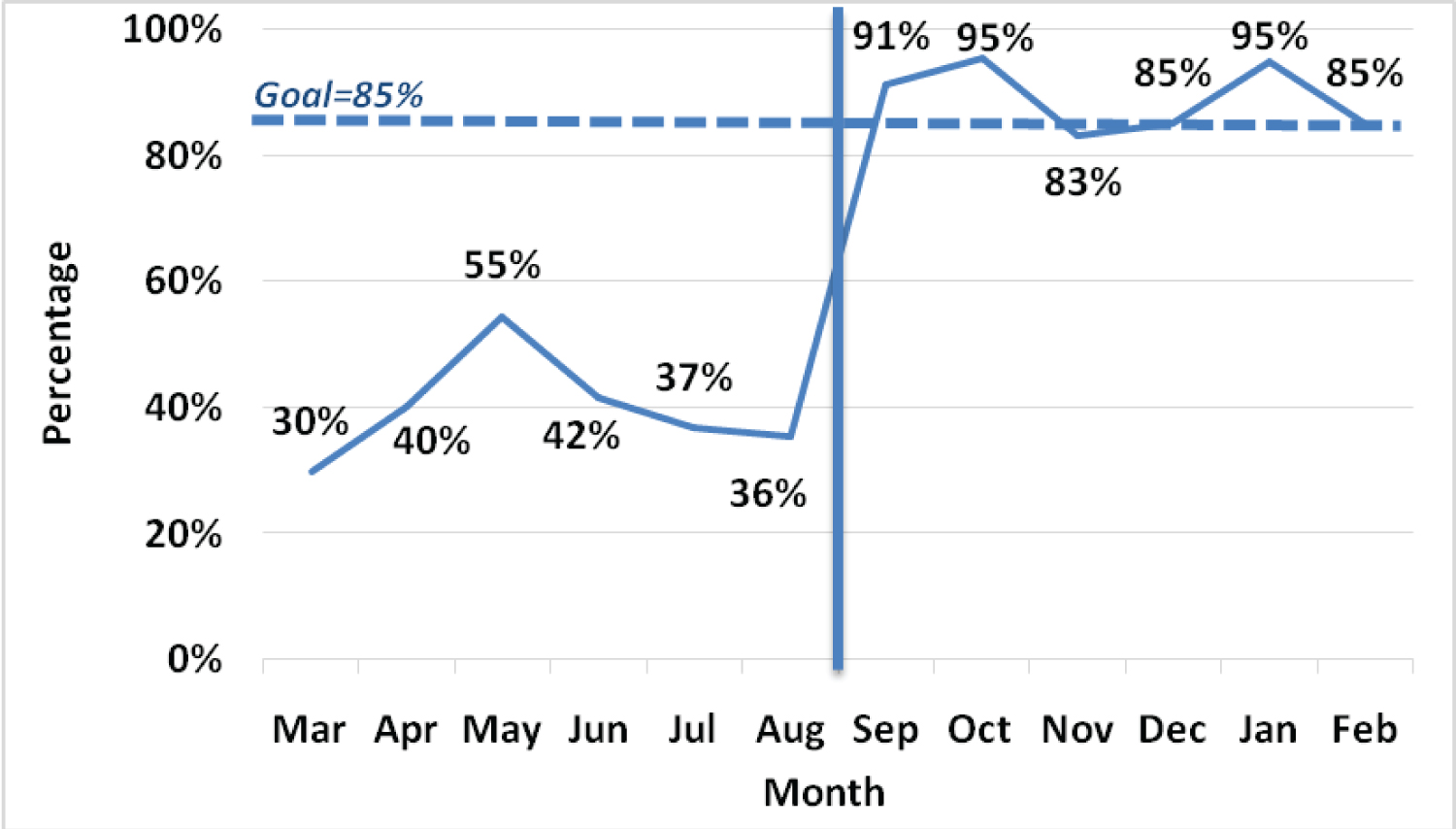
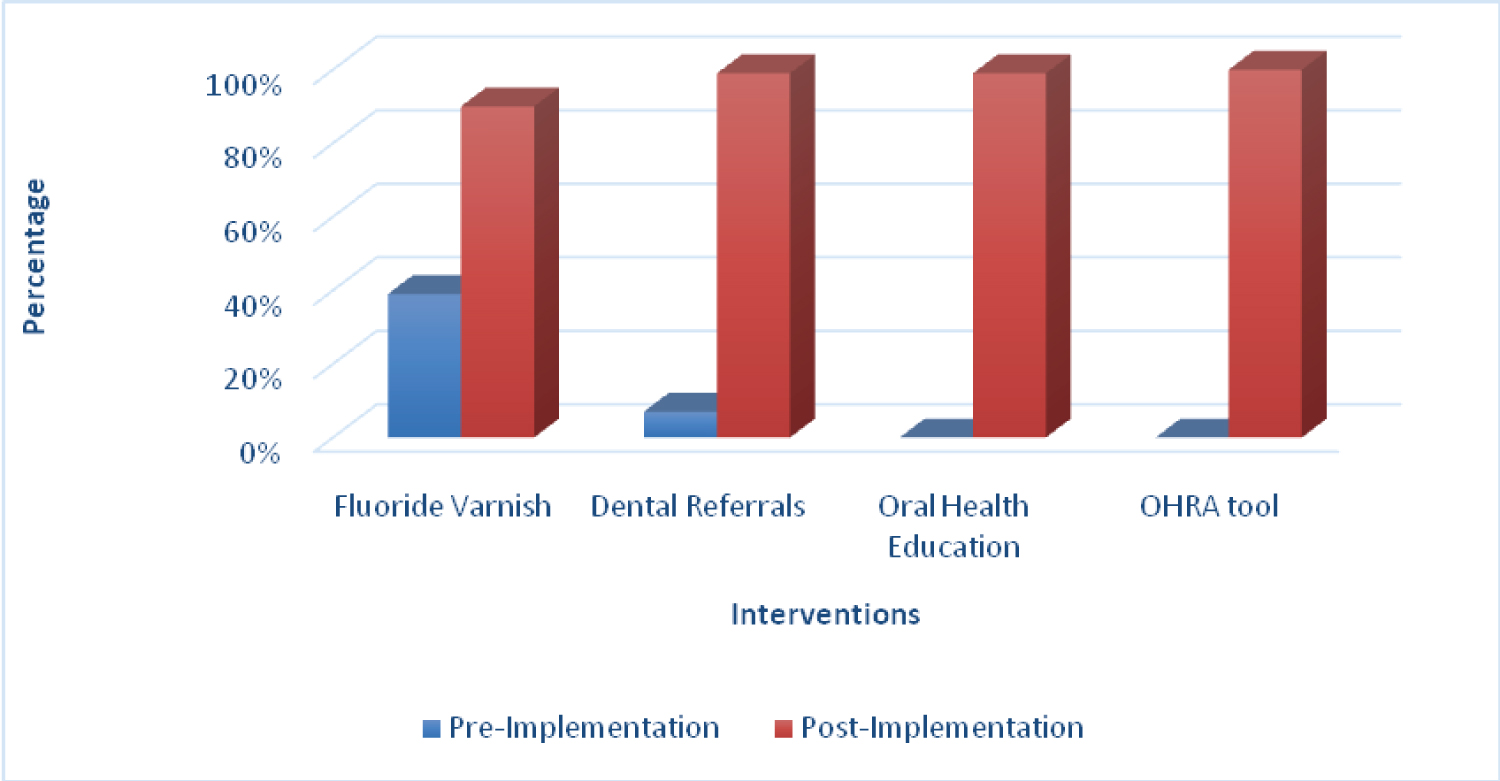
Dental caries is one of the most common, preventable pediatric chronic diseases in the United States. At an urban pediatric office in the Southeast, only 39% of patients between the ages of 12 months to 5 years of age received fluoride varnish. A quality improvement study was implemented utilizing PDSA cycles to improve oral health care and prevention measures in the primary care setting based on the United States Preventive Services Task Force and the American Academy of Pediatrics oral health guidelines. Interventions included an oral health risk assessment tool, staff and caregiver oral health education, and workflow changes to integrate fluoride varnish application. Primary outcome data was collected over six months of pre- and six months of post-implementation. Fluoride varnish rates increased from 39 to 90%. Results suggest a multifaceted approach consisting of evidence-based interventions can increase adherence to oral health preventative measures in the pediatric primary care setting.
Keywords
Dental caries, Pediatrics, Fluoride varnish, Oral health, Quality improvement
Introduction
In the United States, oral health is one of the most common unmet health needs among the pediatric population (Okunseri, et al., 2015). In particular, dental caries remain a significant chronic disease in childhood [1]. About 50% of children have dental caries in one or more primary teeth by the end of their toddler years [2]. Dental caries, also known as tooth decay or cavities, are defined as a plaque-induced acid demineralization of the tooth [3]. Early childhood caries (ECC) is the presence of one or more decayed, missing, or filled primary teeth in a child five years old or younger [3]. Complications of ECC can lead to pain, infection, difficulty eating, weight loss, poor speech, sleep loss, low self-esteem due to dissatisfaction of dental aesthetic, and impact eruption of permanent teeth [2]. These complications may lead to alterations in overall nutrition, growth, and development. Therefore, maintaining the health of primary teeth is essential to a child’s development and health of the permanent teeth [2].
The United States Preventive Services Task Force (USPSTF) and American Academy of Pediatrics (AAP) recommend that primary care providers apply fluoride varnish to the primary teeth of all infants and children starting at the age of 6 months or first tooth eruption until 5-years-old [4,5]. In addition, the AAP recommends that primary care providers begin oral health assessments starting at 6 months of age [4]. This includes asking about the parent’s and patient’s oral health practices and examining the patient’s mouth to assess the risk of caries.
To gain more insight on adherence to guidelines at an urban pediatric primary care office located in Southern United States, the author conducted a random chart review of patients ages 12 months to 5 years for adherence to fluoride varnish application, oral health risk assessment, and caregiver education. At this clinic, oral health assessment did not begin until 12 months of age. Only 39% of eligible well-child visits included the recommended application of fluoride varnish. In addition, 53% of patients reported not having a dental home, while only 7% of those received a dental referral. No patients had documentation of oral health risk assessment, oral health education or anticipatory guidance discussed. The findings led to the development and implementation of a multifaceted approach to help nurses and providers adhere to oral health guidelines at well-child visits.
Literature Review
A literature search was conducted using CINAHL Complete and Scopus search engines. The search terms included oral health, oral hygiene, dental health, dental care, dental hygiene, oral care, fluoride varnish, pediatrics, children, primary care, and primary health care . Abstracts were reviewed to determine relevance to fluoride varnish application in the pediatric primary care setting. Five articles were selected based on implementation of preventative oral health services in children, and assessment, and the impact on fluoride varnish rates.
Literature supported multifaceted interventions focused on an oral health risk assessment tool, workflow changes, and education to staff and caregivers using the Plan-Do-Study-Act (PDSA) model. PDSA cycles consist of four steps that are carried out within rapid cycles [6]. With the use of a PDSA cycle approach in the primary care setting, interventions can be rapidly tested with either continuous adoption or modification to build success [7-9]. The results of the literature review demonstrate the effectiveness of implementing a multifaceted approach utilizing PDSA cycles to improve oral health care and prevention measures in the primary care setting [7-9].
Incorporating the AAP Oral Health Risk Assessment (OHRA) tool into the dental history in two quality improvement studies was associated with an increase in oral health screening rates and fluoride varnish application [8,10]. The risk assessment tool was provided to parents during their child’s well-child visit to identify caries risk and status of a dental home [8,10]. The AAP OHRA tool includes a checklist that serves as a guide and reminder for providers to order fluoride varnish, provide anticipatory guidance, and/ or give a dental referral if needed. The incorporation of checklists or tools showed to help facilitate oral health assessments [8,10].
Maximizing team roles and minimizing the pressure on the providers’ workflow is associated with increased adherence to oral health prevention measures [7,8,10,11]. Changes include expanding the role of the nursing staff in documenting risk assessments, documenting patient’s dental home, applying fluoride varnishes, and providing oral health care education [7,8,10,11]. Time-efficient interventions included placing list of local dentists and fluoride varnish kit in the examination room to make easily accessible and serve as a visual reminder [7,11]. Other workflow changes, including reminders and communication during daily huddles, also played a role in an increase in oral health assessments and fluoride varnish applications [7,9]. Daily huddles were an effective method to allow time for questions, concerns, and feedback for improvement among staff [7,10].
Evidence supports educational interventions to increase the staff’s knowledge and awareness of oral health, dental caries prevention, and fluoride varnish application in young children [7-9,11]. Interventions included online training by Smiles for Life , knowledge and skills training in office, a PowerPoint presentation, and a resource notebook containing guidelines on fluoride varnish application [7-9,11]. Education on current guidelines increased the staff’s knowledge and awareness, which ultimately increased adherence to oral health preventative measures [7-9,11]. Furthermore, evidence also supports educating the caregiver at the well child visit. In a quality improvement project by [8], nursing staff provided standardized oral health education and providers reinforced anticipatory guidance to the parent with an associated increase in successfully increase in fluoride varnish rates and decreased refusals [10].
Literature supported multifaceted interventions focused on an oral health risk assessment tool, workflow changes, and education to staff and caregivers using the Plan-Do-Study-Act (PDSA) model. PDSA cycles consist of four steps that are carried out within rapid cycles [6]. With the use of a PDSA cycle approach in the primary care setting, interventions can be rapidly tested with either continuous adoption or modification to build success [7-9]. The results of the literature review demonstrate the effectiveness of implementing a multifaceted approach utilizing PDSA cycles to improve oral health care and prevention measures in the primary care setting [7-9].
Purpose
The purpose of this quality improvement project was to increase the rates of fluoride varnish application in well-child visits from 6 months of age or first tooth eruption to 5-years-old through the implementation of evidence-based interventions using PDSA cycles. The interventions included staff oral health education, workflow changes, the AAP OHRA Tool, fluoride varnish application from first tooth eruption to 5 years of age, and parent/guardian oral health education. Secondary outcomes included: (1) Adherence to oral health risk assessments, (2) Completion of parent/guardian oral health education, and (3) Dental referrals for patients without a dental home or at high risk for caries.
Methods
Setting
This QI project was implemented at an urban pediatric primary care office located in Southern United States. The office is a private practice serving over 9,000 patients annually. This office accepts Medicaid plans, most private insurance carriers, and self-pay. Staff members include two full-time physicians, four full-time nurse practitioners, one part-time nurse practitioner, two full-time licensed practice nurses, five full-time certified medical assistants, one part-time registered nurse, and four full-time front office staff. The author was the project coordinator leading the planning, development of interventions, providing staff and provider education, data collection, and analysis. The target population was chosen based on AAP and USPSTF guidelines. This project included patients from 6 months of age or first tooth eruption to 5-years-old. Patients eligible for criteria for application of a fluoride varnish included patients ages of 6 months and 5 years of age with tooth eruption presenting for a well-child visit.
Prior to this project, nurses inconsistently asked about a patient’s dental history and their dental home but lacking a standardized oral health risk assessment tool. Fluoride varnishes were ordered by a provider for patients from ages 12 months to 5 years of age at the end of a visit, but there were low rates of application. All nurses were trained during orientation on how to apply fluoride varnish to patients by completing the Smiles for Life Oral Health online training module. If a patient did not have a dental home, a dental sheet was provided. The dental sheet was a list of local pediatric dentists utilized as a dental referral. However, dental referrals, education, assessment, fluoride varnish application, and documentation were inconsistently completed.
Interventions
The interventions of this quality improvement project include several evidence-based components to increase fluoride varnish application rates in children. PDSA was utilized to guide the implementation, evaluation, and project management. This approach allowed for rapid implementation and evaluation of interventions with opportunities for refinement to enhance outcomes. Specific interventions implemented in this project included (1) Staff and caregiver oral health education (2) The AAP OHRA Tool, and (3) Workflow changes that included placing dental sheets and fluoride varnish kits in the examination rooms and daily huddles.
6.2.1. Plan: Pre-intervention data was collected over 6 months through chart reviews to assess the primary care clinic’s rates of fluoride varnishes and dental referrals at well-child visits in children between the ages of 6 months or first tooth eruption to 5-years-old. A root cause analysis was conducted by the author, clinic staff, and providers on the low fluoride varnish rates and dental referrals. Root causes included staff resistance to fluoride varnish application due to COVID-19, time constraints, non-adherence to oral health guidelines, lack of dental referrals and a standardized oral health assessment. At this clinic, assessment of oral health and application of fluoride varnish did not begin until 12 months of age which is inconsistent with the AAP guidelines. In addition, fluoride varnish is not covered by all private insurance companies. Patients without medical insurance are also responsible for the cost of the varnish and while the cost was $18.00. The caregivers were refusing with no oral health education or anticipatory guidance provided.
A plan to address these barriers was developed based on choosing evidenced based interventions that were feasible at this primary care practice. Interventions included oral health education for staff, workflow changes, AAP OHRA tool from 6 months of age to 5 years of age, fluoride varnish application from first tooth eruption to 5 years of age, and parent/guardian oral health education, which was consistent with AAP guidelines. The OHRA tool supported the provider in acquiring information about the caregiver’s oral health, the patient’s oral health practices, examination of the oral cavity, and develop an appropriate plan. It includes the following components: (a) Risk factors (b) Protective factors (c) Clinical findings (d) Levels of caries risk (e) Checklist of services and (f) Self-management goals [12]. If any of the risk factors or positive clinical findings were documented yes, then the patient was at a high risk for caries and the tool serves as a guide for the provider to order application of a fluoride varnish and a referral to a pediatric dentist. If any of the risk factors or clinical findings, marked with an explanation point, were documented no, then the provider used clinical judgement to determine if the patient was at high risk of caries based on positive responses to other risk factors or clinical findings [12]. There is also a checklist on the tool that served as a reminder to give anticipatory guidance, apply fluoride varnish, and/or give a dental referral if needed. Implementation was over a 6-month period and all interventions were simultaneously implemented.
6.2.2. DO: The first intervention included staff education on oral health care, the AAP OHRA tool, and current recommendations on fluoride varnish. A presentation was given to all staff and included information on dental caries, how to use the AAP OHRA tool, recommendations on when and how to apply fluoride varnish, and clinic goals for oral health assessment and dental referrals. Education also included how to document the oral health assessment, fluoride varnish application, oral health education, anticipatory guidance, and parent/guardian fluoride varnish refusals in the electronic medical record (EMR). Concerns regarding COVID-19 exposure with oral health assessment and fluoride varnish application were addressed. Following the presentation, a group discussion addressed questions, concerns, and further exploration of the evidence and interventions. A resource notebook was placed at the nursing station that included current guidelines on fluoride varnish application for staff to refer to if needed. Lastly, the online education course, Smiles for Life , remained a continued requirement for all new hires.
The second intervention focused on changes in clinic workflow to maximize team roles from check-in to check-out. Workflow changes included daily staff huddles for reminders, updating referral lists of dental offices, and visual reminders including fluoride varnish kits and dental sheets in each exam room. Front-desk staff assessed the patient for COVID-19 symptoms. If no symptoms, the front desk staff roomed the patient on the well side of the clinic. If the patient disclosed COVID-19 symptoms or known exposure, the front desk staff roomed the patient on the sick side for further evaluation and COVID-19 testing prior to completion of the well-visit. If a positive COVID-19 test, the well-child visit was rescheduled; however, if the COVID-19 test was negative, then the well-child check continued with AAP OHRA tool and fluoride varnish application.
At the beginning of the well-child visit, starting at 6 months, the nursing staff gave the paper AAP OHRA tool on a clipboard to the parent and/or guardian to complete and provided oral health education to the caregiver during the rooming process. Standard oral health education included brushing teeth twice a day, regular dental visits starting at 12 months of age, limiting sugary drinks, and the importance of a fluoride varnish. The nurse placed a fluoride varnish kit in the in the examination room to serve as a visual reminder to ensure completion of the OHRA and application of the fluoride varnish for the nurse. The parent and/or guardian completed the AAP OHRA tool after the nurse completed patient check-in and while waiting on the provider to enter the room. Upon entering the room, the provider reviewed the completed AAP OHRA tool, performed an oral health visual examination, and reinforced age-appropriate anticipatory guidance. The provider placed a fluoride varnish order in the EMR. At the end of the visit, the nursing staff applied the fluoride varnish. If the patient was at high risk for caries and/or did not have a dental home, a dental sheet with an updated list of local dentists was given to the parent/guardian by the provider. Dental sheets were placed in each examination room so that it is easily accessible. At the end of the visit, the results of the paper OHRA were transcribed into the dental history section of the EMR by the nursing staff. After it was transcribed, it was placed in the scan folder to be scanned into the EMR by the front desk staff. If a dental sheet was given or if fluoride varnish was applied, it was documented in the plan section of the EMR by the provider. The provider entered the current procedural terminology (CPT) code 99188 in the EMR. If a fluoride varnish was not applied, the nursing staff documented a reason why it was not applied in the EMR.
6.2.3. Study: Data was collected biweekly on the adherence to fluoride varnish application, AAP OHRA tool in patient’s chart, education, anticipatory guidance, dental referrals, and CPT codes. The providers and staff were engaged in a biweekly discussion during the daily huddle to provide data trends, determine challenges and successes of the interventions, make any needed changes, and receive feedback.
6.2.4. Act: Challenges, feedback, and necessary changes were addressed within the biweekly huddle. Additional PDSA cycles were implemented following intervention changes. Over the 6-month implementation period, the changes included scheduling the patient for a nurse visit to come back for fluoride varnish application if the patient was sick and having one nurse assigned to do nurse visits only. By having one nurse assigned to do nurse visits only, it allowed the nurse to have more time during the visit to give oral health education and fluoride varnish application. The last change that was implemented was deciding that a patient can receive a fluoride varnish if a fluoride varnish was applied greater than one month prior to the visit.
Measures and data collection
The primary outcome measure was patients from ages 6 months or first tooth eruption to 5 years of age with documented fluoride varnish application. Process measures included (a) The number staff that attended the educational session, (b) Completed AAP OHRA tool, (c) Documentation of dental referral sheet provided to high-risk patients, (d) Documentation of oral health care education by nursing staff, (e) Documentation of anticipatory guidance by the provider, and (f) CPT code in chart by the provider.
Pre-intervention data collection was obtained by the author from March 2022 to August 2022 by a chart review of patients between the ages of 12 months to 5-years-old to determine the rate of fluoride varnish application. Additional data collection included age, provider seen at the visit, dental home, if patient received a dental referral, if patient had teeth present, and if a fluoride varnish CPT code was placed in chart.
Implementation and post-data collection occurred from September 2022 to March 2023 by a chart review of all patients from ages 6 months to five years of age presenting for well-child visit. The same information was obtained as the pre-intervention data, however, post-intervention data also included if oral health education and anticipatory guidance was given, if the oral health assessment tool was in the chart, and if the patients were determined to be high risk for caries. Pre- and post-intervention data were analyzed using descriptive statistics including means and percentages. Microsoft Excel © was used for graphical display to trend data.
Ethical considerations
The university’s Quality Improvement/Program Evaluation Self-Certification Tool was completed, and the project was deemed a quality improvement project. Therefore, IRB review of this project was not required. Privacy and confidentiality of the patients were ensured. De-identified data included in the data analysis was collected, and stored on a secure, encrypted password protected server.
Results
The charts of 488 patients were reviewed in the pre-intervention period (March 1, 2022-August 31, 2022) and 526 patients for the post-intervention period (September 19, 2022- February 28, 2023). In the pre-intervention period, oral health risk assessments were not being completed and parents/guardians were not receiving oral health education based on documentation in the EMR. All well child visits from 6 months of age to 5 years of age were eligible for an oral health assessment and oral health education. With the implementation of oral health assessments, 100% of patients were screened utilizing the AAP OHRA tool post-intervention (Figure 1). Out of the 526 patients screened, 11% (56) were determined to be at high risk for caries. During the pre-intervention period, 63% (259/412) of patients did not have a dental home versus 54% (263/485) in the post-intervention period. Rates of dental referrals for children who were identified as high risk and/or without a dental home increased from 2% (17/259) in the pre-intervention period to 99% (269/273) in the post-intervention period (Figure 2). During the post-intervention period, 99% (522/526) of parents/guardians received oral health education by the nursing staff and 99% (524/526) received anticipatory guidance given by the provider (Figure 2).
All well child visits from first tooth eruption to 5 years of age were eligible for fluoride varnish application. In the pre-intervention period, 412 patients were eligible for fluoride varnish application versus 485 patients in the post-intervention period. Fluoride varnish rates improved significantly from 39% in the pre-intervention period to an average of 90% in the post-intervention period. The fluoride varnish application rate exceeded the clinic benchmark of 85%, peaking at 95% in the poster-intervention period (Figure 2). Rates of CPT codes for fluoride varnish application remained at 100% pre- and post-intervention. Despite oral health education and anticipatory guidance given to the parent/guardian, the refusal rate for fluoride varnish application in the post-intervention period was 7% (36/485). Of the 36 patients that did not receive fluoride varnish application due to refusal by the caregiver, 75% (27/36) had a reason documented for omission, which included sick symptoms or recent dental visit.
Discussion
This quality improvement project aimed to implement evidence-based interventions to increase rates of oral health assessment, oral health education, dental referrals, and fluoride varnish application from age of first tooth eruption to 5-years-old in primary care. Fluoride varnish application rates improved significantly from pre- to post- implementation. All staff was supportive of incorporating these evidenced based interventions into the daily workflow. An educational session on the importance of oral health care and training on workflow changes helped gain support among staff and increase engagement in this project. A project leader present at the clinic also increased staff engagement via intervention and outcome to provide continuous monitoring, support, and feedback to staff during biweekly huddles.
This quality improvement study’s findings were consistent with the literature and the impact of Okah, et al. [7], Sengupta, et al. [10], and Sudhanthar, et al. [8] incorporating oral health assessments, fluoride varnish application, and dental referrals into well child visits. Interventions include staff education, workflow improvements, and adding the AAP oral health assessment tool into the EMR’s dental history section. The incorporation of the AAP OHRA tool increased the identification of children who were at high risk for caries, children without dental homes, and provide age-appropriate oral health education with no perceived increase in workload by the staff. While a simple process change, moving fluoride varnish kits and dental referral sheets into the examination room for easy accessibility contributed to improvement of fluoride varnish application rates and dental referral for children who were identified as high risk and/or without a dental home.
The lowest rate of fluoride varnish application was in November 2021 which was likely due to the start of sick season and being short staffed. A chart review revealed that the date of a patient’s last dental visit and refusal reasons were not being documented correctly. The huddle was spent reviewing where and how to document this correctly. Common refusal reasons included sick symptoms with fever and a recent dental visit. At the biweekly huddle, there was also a lack of understanding with how often a fluoride varnish can be applied. To improve refusal and fluoride varnish application rates, further intervention was done. It was discussed that if a patient received a dental varnish greater than one month ago, then they were eligible to receive another fluoride varnish application. As a result of these changes, the fluoride varnish application rate increased to 95% and decreased the refusal rate to 4% in January.
Limitations
A significant limitation of this study included the 6-month timeframe of implementation. This is due to the inability to demonstrate long term sustainability and the impact of reducing caries. Implementation occurred during the winter months when respiratory illnesses are more common leading to increased sick visits, decreased well child visits, and an increase in well child visits with a concurrent sick issue. This led to an increased number of refusals due to sick symptoms. However, this was addressed by the parents scheduling a nurse visit to come back for a fluoride varnish application only.
A second limitation was a nursing staffing shortage during two months of project implementation, leading to increased responsibility of workflow on a few nurses. Fluoride varnish application rates did decrease during this time, but remained above the pre-intervention rate. A new nurse was hired and trained on fluoride varnish application by Smiles for Life and the project leader, with an increase in fluoride varnish rates and oral health education the following month. Last, the nurses and providers relied on caregiver self-reporting for dental home, last dental visit, and last fluoride varnish possibly contributing to under identification of patients at high risk for caries and needing a dental referral and fluoride varnish application If their last fluoride varnish application was done at the clinic, caregiver self-reporting was minimized by nurses checking the EMR for the date. If it was done greater than one month ago, a dental varnish was applied. In addition, if a patient with a dental home was at high risk for caries based on the AAP OHRA tool or an oral health visual examination, a dental referral was still given.
Conclusion
Nursing staff and primary care providers play an important role in providing education to children and families on preventative oral health care and fluoride varnish. The implementation of an AAP OHRA tool was effective to identify patients in need of a dental referral and to encourage provider/parent discussion about oral health. Maximizing team roles by engaging nursing staff helped support workflow changes and adherence to fluoride varnish application. This study demonstrated the feasibility of incorporating oral health guidelines into practice. A multifaceted intervention is most likely to be successful in an environment with a project leader and supportive team. Future recommendations include incorporating the AAP OHRA tool into the EMR system and sending dental referrals electronically from the primary provider to the dental home in place of dental sheets.
References
- Dooley D, Moultrie NM, Heckman B, et al. (2016) Oral health prevention and toddler well-child care: Routine integration in a safety net system. Pediatrics 137:
- Kazeminia M, Abdi A, Shohaimi S, et al. (2020) Dental caries in primary and permanent teeth in children's worldwide, 1995 to 2019: A systematic review and meta-analysis. Head & Face Medicine, 16:
- American Academy of Pediatric Dentistry (2008) Definition of early childhood caries (ECC).
- Hagan JF, Shaw JS, Duncan PM (2017) Promoting Oral Health. In: Guidelines for Health Supervision of Infants, Children, and Adolescents. (4 th edn), American Academy of Pediatrics, 205-214.
- US Preventive Services Task Force (2021) Prevention of dental caries in children younger than 5 years: Screening and interventions. uspstf/ recommendation/prevention-of-dental-caries-in-children-younger-than-age-5-years-screening-and-interventions.
- White KM (2016) The science of translation and major frameworks. In: KM White, S Dudley-Brown, MF Terhaar, Translation of evidence into nursing and health care. (2 nd edn), Springer Publishing Company, 25-55.
- Okah A, Williams K, Talib N, et al. (2018) Promoting Oral Health in Childhood: A Quality Improvement Project. Pediatrics 141:
- Sudhanthar S, Lapinski J, Turner J, et al. (2019) Improving oral health through dental fluoride varnish application in a primary care paediatric practice. BMJ Open Quality 8:
- Johnson SC, French GM (2020) A quality improvement project to optimize fluoride varnish use in a pediatric outpatient clinic with multiple resident providers. Hawai'i Journal of Health & Social Welfare 79: 7-12.
- Sengupta N, Nanavati S, Cericola M, et al. (2017) Oral health integration into a pediatric practice and coordination of referrals to a colocated dental home at a federally qualified health center. American Journal of Public Health 107: 1627-1629.
- Dahlberg D, Hiott DB, Wilson CC (2019) Implementing pediatric fluoride varnish application in a rural primary care medical office: A feasibility study. Journal of Pediatric Health Care: Official Publication of National Association of Pediatric Nurse Associates & Practitioners 33: 702-710.
- American Academy of Pediatrics (2011) Oral Health Risk Assessment Tool.
Corresponding Author
Jennifer Reilly, BSN, RN, Medical University of South Carolina, Charleston, South Carolina, USA.
Copyright
© 2023 Reilly J, et al. This This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.