Extent to which Visual Inspection with Acetic Acid Screening Guidelines are Adhered to in Selected Health Facilities in Embu County, Kenya before and after Intervention
Abstract
Cervical cancer is one of the few diseases that reflect global inequities. In low and middle income countries, its incidence is nearly twice as high and its death rates three times as high compared to high income countries. Programs must focus on changing these trends. Visualizing with acetic acid encompasses the following: First, the health Care provider (HCP) does vaginal examination using a speculum, then dilute (3-5%) acetic acid (vinegar) is applied to the cervix. The presence of abnormal tissue often temporarily appears white when exposed to vinegar and then cervical color changes are observed with a naked eye. The outcome of Visual inspection with acetic acid is very subjective and depends with the level of skill of health care provider as well as availability of procedure supplies and adhering to Via procedure guidelines. The aim of this study was to determine the Extent to which Visual Inspection with acetic acid guidelines are adhered to in selected health facilities in Embu county prior to intervention and after intervention. An intervention study design was used. In particular, fourteen health care providers who were the initial study respondents were taken through an intensive VIA training for two days didactic and a four days clinical practice with guidance of preceptors. The facilities where respondents were recruited from were selected using a purposeful sampling method. Prior to intervention, a baseline data was taken that included use of questionnaires and observational checklist to determine adherence to VIA guidelines. The health care providers were then followed up for a period of four months where by 434 women were screened. The study area was Embu County in Kenya and the target population was the health services providers who provided VIA services in government facilities. The data was collected through self-administered questionnaires and observational checklists. In addition, secondary data was obtained from the health facility records and KDHS 2014. For data analysis, quantitative techniques of analysis were used. This study established that, despite all the respondents having some form of prior training on cervical cancer screening using VIA/VILLI, positivity rate was low before intervention. Cervical cancer screening guidelines were poorly adhered to prior to training compared to improved adherence after training. After intervention, healthcare providers were able to make the correct diagnosis and identify precancerous lesions. Cervical cancer screening uptake also scaled up. Baseline positivity was 0.8% and after training it was 14.1%. The study Concludes and Recommends that based on the key findings of this study, the MOH VIA training guidelines and curriculum should be revised to accommodate clinical practice for at least 4 days after 2 days didactic training with use of preceptors and cervical images.
Keywords
Visual inspection, Acetic acid guidelines, Cervical cancer
Introduction
Despite cervical cancer being a preventable disease, yet it is the second major cause of cancer associated morbidity and death among women in Kenya [1]. Therefore, a clear understanding of the degree of public health burden that cervical cancer places on some of the world's most vulnerable women, is critical. It is also crucial to understand the importance of screening and why it is the paramount option for decreasing cervical cancer mortality. Being a signatory to many Europe, Asia, America, Australia, Africa human rights agreements and declarations, Kenya as a Country was under obligation to address the pressing matters of reproductive health and control of non-communicable diseases [2]. Visualizing with acetic acid encompasses the following: First, the HCP does vaginal examination using a speculum, the dilute (3-5%) acetic acid (vinegar) is applied to the cervix. The presence of abnormal tissue often temporarily appears white when exposed to vinegar and then cervical color changes are observed with a naked eye. Possible conclusions by the HCP include either positive or negative precancerous lesions or outcome or possibly suspect cancer [3].
A sharp, distinct, well-defined, dense acetowhite areas, with or without raised margins touching the squamocolumnar junction (SCJ) is characteristic of a positive VIA test [4]. Various previous studies show a relatively higher sensitivity (81%) of VIA and a specificity (83%), a test that uses instrument sets and equipment usually available at healthcare centers, which is a little lower than cytology (86%). While sensitivity refers to percentage of all those with the disease that the laboratory test appropriately identifies as positive, specificity on the other hand is the proportion of all those without disease that the laboratory test correctly identifies as negative.
Imortantly, VIA allow "screen and treat" strategy as it provides immediate results and does not require laboratory tests. Further, this method ensures clients are treated on single visit approach, hence reducing loss to follow up. As a result, greater accuracy has been observed with visual tests compared to Pap smears. Since they provide immediate outcome, women who need treatment can as soon as possible at the health facility or be referred to another HCP. Worth noting is that VIA has a lower specificity compared to other methods, thus there is a potential for over treatment if visualization is not carefully and consistently supervised. There seems to be a marked improvement with practice on the ability of HCP to perform the procedure of VIA to identify a normal cervix correctly (specificity) according to Adsul, et al. [4]. At the center of ensuring the effectiveness of VIA is the need for effective training and quality assurance programs. Annex 3 shows VIA national screening guidelines.
Between September 2005 and May 2009, almost a 4 year period, a total of 19,579 women were screened from six African Countries. The results were as follows: VIA positive 10.1%, suspicious for cancer 1.7% on examination. 87.7% of all VIA positive clients got cryotherapy treatment within a week of VIA screening. Single visit approach saw 39.1% of women to be screened and provided with treatment on the same day [1]. The women who did not receive 'screen-and-treat' single visit approach did not receive for several reasons such as inadequate cryotherapy equipment or them not working at the time of screening and the fact that some clients required consent from their spouses.
Visual Inspection with Acetic Acid Training
In resource limited settings such as Kenya, it has become almost impossible to implement the current cervical cancer prevention approaches, that is, the use of cytology and multiple visits for diagnosis. For that reason, the Alliance for Cervical Cancer Prevention (ACCP) therefore, has taken upon itself as a priority to assess alternative approaches. The use of VIA and VILI to identify precancerous lesions including utilization of cryotherapy treatment technique for precancerous lesions are some these approaches. Following the experiences of ACCP from their training of HCPs (nurse and doctors) on these techniques, stakeholders now agree that first, the training should be in a clinical setting or a simulated clinical setting; secondly, it should be competency based and; thirdly, it should incorporate both didactic and practical hands-on sessions [5]. In a study done by Veena [6], non Health care providers were trained using the same principles of didactic and practical training, the only difference is that practical training took four weeks and they were able to identify precancerous lesions.
A competency based training, that is not only practical and focused, but also accessible, culturally appropriate, feasible as well as being easy to understand for the intended audience, are important attributes necessary for any program to be effective or successful. Similarly, an effective VIA training program has four key components it focuses on: firstly, the general principles of training; secondly, training for VIA; thirdly, training for cryotherapy and last but not least, the training for quality assurance and supervision [5].
There is also low uptake of screening, lack of adherence to the guidelines and deficient training programs lacking the practical element as part of the problem. The subjective nature of VIA test, makes this all the more important. According to KDHS report [7]. 13.45 million Females who are 15 and above years of age, who were at risk of developing cervical cancer. The same report further indicated that the annual number of cervical cancer cases was 4,802, out of which 2,451 dying every year [8,9]. Despite the widespread screening efforts, cervical cancer deaths and invasive cervical cancer cases have not reduced. Hence, the author proposed that with appropriate training of health care workers and adherence to screening guidelines, VIA was a powerful screening tool that should be able to detect early precancerous lesions for a timely intervention [8]. Although, a policy environment in Kenya on use of VIA for cervical pre-cancer screening is there, with the help of NGO's most hospitals have VIA/VILLI screening programs The current training program lacks practical component which contributes to the ineffectiveness of the training. Practical components should be incorporated to the current training program to improve outcomes. However, evidence showed that VIA positivity rate in Embu county was 1% [10], thus falling short of the WHO threshold of 10-15% in any given population as per World Health Organization (WHO). Irrespective of having an enabling policy atmosphere to endorse universal access to reproductive health, a disconnect between the policies and action still exists, leaving a gap that requires to be filled.
Research Methodology
Embu county, located nearly 130 kilometers north-east of Nairobi, is one of the fourty seven counties in Kenya covering an area covers of 2,818 square kilometers, as shown in Appendix 9. According to the latest household population census, 2019, there were about 516,212 people living in Embu county. The major ethnic communities in the county are the Mbeere, Embu and the Akamba. It is made up of four sub counties of Runyenjes, Manyatta, Mbeere South and Mbeere North. The Embu county is home to Mwea National Reserve and three of the famous seven Kenya's hydroelectric dams along the river Tana namely: Kamburu, Kindaruma and Kiambeere dams. The key economic undertakings in the area include tea, coffee, macadamia and dairy farming among others. Importantly, the Embu county has 75 health public facilities, 2 non-governmental facilities, 24 faith based facilities and 41 private facilities. The health personnel ratios in Embu are 111 nurses for every 100,000 people, 21 doctors for every 100,000 people and 21 clinical officers for every 100,000 people. The screening services offered in Embu County mainly are VIA/VILLI and papsmear. Cryotherapy is only done in facilities with the machine. Although cryotherapy was available in Embu County Referral Hospital, it was not functional by the time of this study. In general, the prevalence of cancers in Embu County is 0.5%, while that of cervical cancer is 0.2%. According to a report by DHIS, [10], on female cancer cases, the prevalence of cervical cancer in 2015, 2016 was 7.9% and 13.2%, respectively.
Research Design and Rationale
This study was multi-phased and multi-site. In Phase one, a baseline survey was undertaken to assess the extent of VIA positivity rate in Embu county in the selected facilities. This was followed by a qualitative assessment to determine adherence to VIA screening guidelines. In Phase two, training on cervical cancer screening was done using a curriculum that meets the ACCP recommendations and in line with Kenya VIA and cryotherapy training guidelines. A pretest was administered before the theory training and a posttest after the theory training. A two day theory training was followed by four day clinical training in a health campaign set up at Dallas dispensary Embu. Every two trainees were mentored by a preceptor for the period of clinical training. In phase three, the trained health care providers offered VIA screening in their facility and they were followed up for a period of four months as data was collected on ability to identify precancerous lesions. The effectiveness of screening outcome was verified by the screening preceptors, who are experts in cervical pre-cancer screening. A qualitative assessment using checklists was done at the end of the four months follow-up period to evaluate adherence to VIA screening guidelines.
This was an intervention study design. According to Cresswell & Plano [11], Interventional method study design emphasizes on collecting data post-intervention and intervention and post-intervention phase.
This design aimed at evaluating the effectiveness of VIA training on improving knowledge, and skills amongst health workers as well as outcomes among clients in selected hospitals in Embu County.
Study Population
This study targeted all health care workers offering VIA screening to women 25-49 years in the selected county hospitals in Embu county in Kenya. Embu county has a total females population of 287,531, out of which 86,259 were reproductive age and eligible for cervical cancer screening. The study participants were 14 trained health care providers.
Sampling Techniques
The researcher employed purposeful sampling technique to select seven government health facilities already offering VIA in the county. There are 4 hospitals and 12 health centers owned by government in this county. From the seven facilities selected randomly, two nurses offering VIA from each facility were purposefully sampled, trained for six days and followed for a period of four months as they screened women for cervical cancer in presence of a preceptor to determine the outcomes of the training.
Sample Size Determination
Due to the intensity and nature of the training, the curriculum accommodated 14 participants in didactic training.
Inclusion Criteria
Health care workers who do VIA and consented to the study to ensure minimum attrition. Health care providers passionate about VIA, this is because they would take personal initiative and interest in the VIA screening and would stay in the course of the study without feeling unnecessary pressure. Health care providers likely not to be transferred from their facility during the period of study. This was to ensure minimal drop out in the course of the study.
Exclusion Criteria
All health care workers who doubled up as facility managers in their health care facilities were excluded from the study. When managers are involved in such an intensive study, the balance between the hospital management activities, study may crush and since the study is not part of the manager's job description, may suffer lack of commitment.
Data Collection Techniques
Questionnaires, observational checklists and structured interviews for key informants were used in this study. Self-administered semi-structured questionnaire were used to collect quantitative data. Likewise, observational checklist for VIA providers to assess adherence to screening guidelines were used. In addition, secondary data was obtained from the health facility records and KDHS, 2014 and facility cervical cancer screening and treatment registers. The Pre-test and post-test were administered during the training phase. In particular, observational checklists were used to evaluate the level of compliance to the VIA screening guidelines.
Data Analysis
Both qualitative and quantitative analysis techniques were used. To ensure quality, the principal researcher closely monitored and supervised the data collection process. The cleaning and coding of quantitative data from tools was done before transcribing the data into Statistical Package for Social Sciences (SPSS) data analysis software version 21.0. Frequency distributions based on background characteristics, was used to demonstrate the distribution of the study population through univariate analysis. A cross tabulation was done after data entry for bivariate analysis. Cohen's Kappa Co-efficiency was used to show accurateness of VIA diagnosis through agreement between trainees and preceptors.
Logistical and Ethical Considerations
Research ethics committee approval
An ethical approval was obtained from University of Nairobi Ethical Committee reference number KNH-ERCIA/332. The approval was granted on 9th September 2019. The National Commission for Science and Technology (NACOSTI) issued the research permit reference number 291817 as shown in Appendix 10. The research permit was granted on 10th October 2019. Research authorization was also granted by the county commissioner Embu County and Ministry of Education Embu County. Authorization at the hospital level was obtained from the Embu county director of health who wrote to sub county MOH's to gain access to the specific hospitals in their jurisdiction. The letter was presented to the Nursing officer in-charge of the sampled health facilities, who gave permission to access MCH/FP rooms and administer research questionnaire to the health care professionals. They also released the health care workers for the 6 days training. In Embu level five Hospital, the county director's letter of research authorization was presented to the hospital chief executive officer, who gave permission to carry out the study in the hospital.
Results
Demographic data for health care providers
The demographic data for the HSPs is summarized in Table 1. According to the findings in Table 1, out of the fourteen health care providers, majority were male 92.9% (n = 13), 78.6% (n = 11) had diploma level of education, half 50% (n = 7) of the respondent had been in the same facility for more than five years. In terms of religion, 50% (n = 7) were Protestants. This implies that they were qualified to work in a referral health facility. Since, they had also worked for a considerable number of years in the facility; they were in a good position to respond to questions regarding cancer screening in the facility. The females outweighed males workers in the health facility which was beneficial to the study since women would prefer to be screened by their fellow women as this process involves exposure of genitals.
Extent to which VIA screening guidelines are adhered to in the facilities prior to intervention
The study sought also to find out the extent to which VIA screening guidelines were adhered to in the facilities. The Findings in Table 2 show that majority of the respondents used Zesta brand of acetic acid to perform VIA. Out of the three commonly used brands of acetic acid, only American garden has the recommended 3-5% concentration. The findings also revealed that the brand of acetic acid used bear some percentage of acetic acid although it does not conform to the recommended percentage used for VIA which is 3-5%. The majority of the HCPs applied acetic acid on the cervix for one or two minutes, they thought that cotton applicator stick to be used to apply acetic acid to the cervix, should be enough to cover the Squamous columnar junction. Women of reproductive age 25-49 years in Kenya were eligible for VIA, and it was important to visualize squamo columnar junction before applying acetic acid. However, half of the respondents thought women above 50 years were not eligible for VIA because their squamous columnar junction was not obvious.
VIA Standard Procedure Observational Checklist
Before the training, the fourteen health workers were evaluated using an observational checklist on their abilities in VIA. The checklist was divided into two categories; preparation and visual inspection with acetic acid categories. Their abilities ranged from very satisfactory to very unsatisfactory where satisfactory implied the health employee completed the steps/task conforming to the guidelines/standard procedures and unsatisfactory implied the converse of satisfactory. During the baseline evaluation stage only data for twelve participants was used since two of them lacked supplies to carry on the procedures.
NB/ Cryotherapy observational checklist was not used because in 6 out of the 7 facilities, no one was trained on cryotherapy. Embu county referral hospital which had a cryotherapy machine and one trained personnel, the machine had broken down.
Table 3 shows that; "Remove the speculum and place it in a bucket with soapy water or 0.5% chlorine solution for 10 min for decontamination" section was the only procedural stage where all the participants scored 100% of 'Very satisfactory' implying that it was well executed. However, there are other procedural stages like 'Examining the cervix and establishing whether it is suspicious of cancer' 'Using the light source to identify the cervical os, the Squamo-columnar junction (SCJ) and the transformation zone', 'Soaking a clean cotton swab with 3-5% acetic acid (vinegar) and applying to the cervix for 2 minutes', 'Careful inspection of the SCJ: Checking for any raised and thickened white plaques or acetowhite epithelium and if there is a lesion, inspect it to determine if the lesion has clear borders, and if it is touching the SCJ. Note the size of the lesion', and 'If necessary, re-apply the vinegar for another minute. Then use a cotton swab to remove mucous or blood that is obstructing your view. Inspect the SCJ again' that majority of the participants did not perform above the neutral level implying need for intervention. From the observational checklist, the study established that participants did not know how to identify SCJ, did not time their duration of contact between vinegar swab and cervix and none had a watch to time the two minutes, most health care workers just dubbed the vinegar swab on the cervix, and they did not know what an ACETOWHITE lesion looks like.
Likert Scale
1 = Very Unsatisfied (VU), 2 = Unsatisfied (U), 3 = Neutral (N), 4 = Satisfactory (S), 5 = Very Satisfactory (VS)
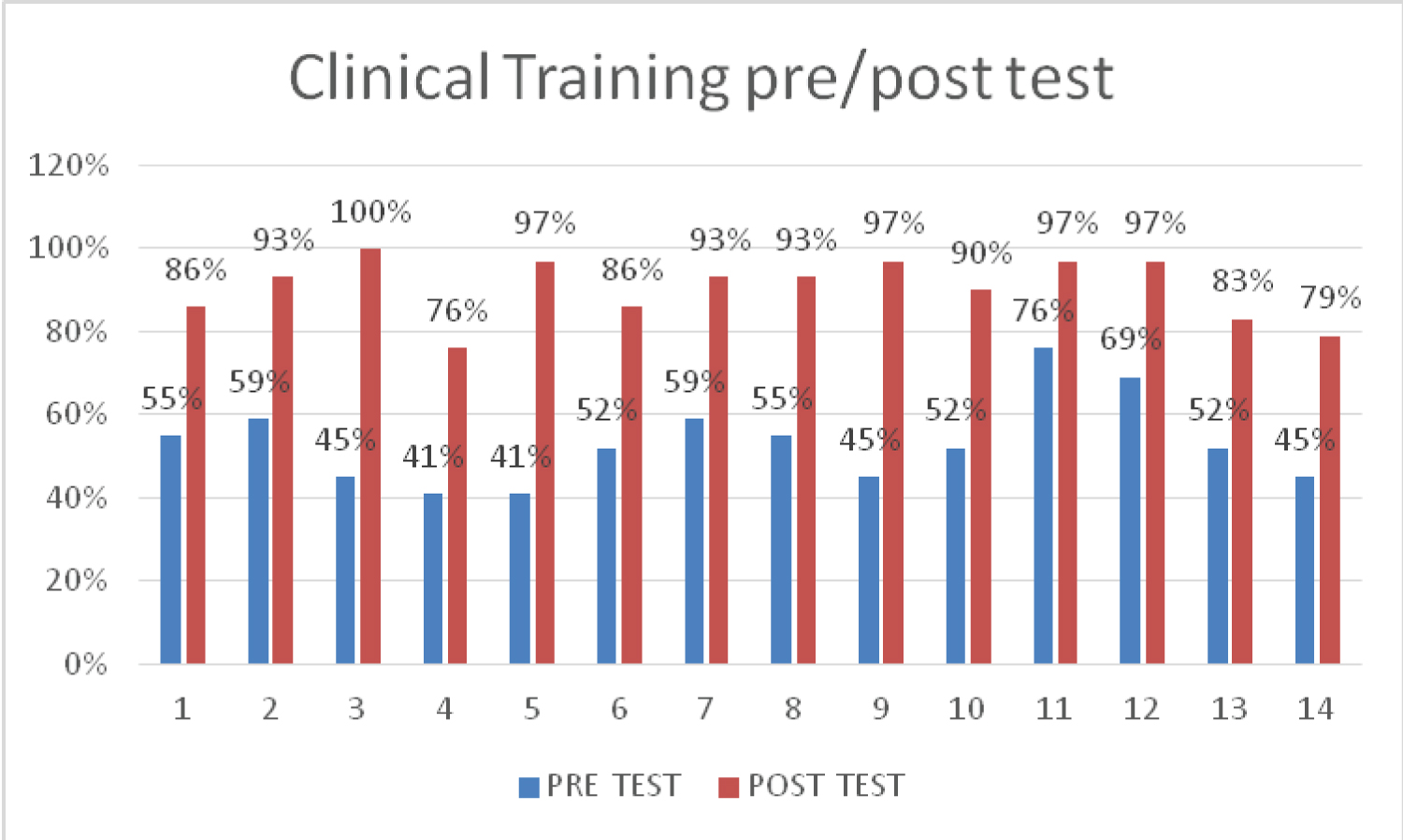
VIA and Cryotherapy Clinical Pre-/Post-Training Test
Upon the start of the didactic training, all participants were given a pretest and a post-test at the end of didactic training. Figure 1 shows the VIA and Cryotherapy clinical training test performance for the fourteen health care providers during the theory training session. The figure signifies the level of preparedness of clinical health care workers on their abilities on performing VIA and Cryotherapy procedures before and after the theory training. During the pre-training assessment the participants had a mean score of 53.3%, SD of 10.18, the minimum score being 41% and the maximum being 76%. Nevertheless, during the post-training assessment there was a significant improvement with the respondents having a mean score of 90.5%, SD of 7.43 with the least score being 76% and the highest scoring 100%. Post- and pre-training test results signified a positive impact the training had on health workers. This shows a significant improvement from pre-training performance to post-training results.
VIA and Cryotherapy Observational Checklist Evaluation
After the four days training, the fourteen clinical health workers went back to their facilities to practice. They were followed up for a period of four months with the supervision of a preceptor as they screened the VIA eligible women. They were evaluated with VIA and cryotherapy observational checklists to check their ability to follow laid down guidelines and make correct diagnosis of VIA. The participants' abilities were classified from 'very satisfactory' to 'very unsatisfactory' where satisfactory implied that the procedure was executed conforming to the guidelines/standard procedures for either VIA or cryotherapy treatment for precancerous lesions. On the other hand, unsatisfactory inferred that the test did not meet the standard for procedure.
Evaluation
The VIA evaluation checklist was subdivided into two major groups; preparation and visual inspection with acetic acid categories. The Table 4 below show that after the training there was a tremendous improvement on clinical health workers abilities to perform VIA in comparison to Table 4, which was conducted prior to the training. All the participants adhered to the VIA guidelines in all levels of the procedure.
Discussions
For VIA cervical cancer screening and treatment, the Ministry of Health Kenya has come up with guidelines that are standard operating procedures, to which every skilled VIA provider should be able to adhere to. The researcher used observational checklists to observe health care providers as they provided the screening service to clients and likerts scale to gauge performance against steps that were to be followed. Questionnaires were also used with guidelines specific questions. It is important to note that in one facility, there were no screening reagents, specifically vinegar and for that reason, observational checklist was not used. It is also important to note that cryotherapy observational checklist was not used at baseline data collection stage, as there was no one trained and with skills on how to treat a precancerous lesion using cryotherapy. Furthermore, the only facility which was referral center for cryotherapy treatment, Embu County referral Hospital, the cryotherapy machine had broken down. Assessment of adherence to guideline also involved use of questionnaire to assess knowledge on some of the standards to performing VIA. On the brand of acetic acid used, majority of participants used Zesta, which is a brand that does not meet the standard threshold of acetic acid concentration adequate to create a reaction with cervical cells to show presence or absence of precancerous acetowhite changes. Another brand used was cloves at which again falls short of 3-5% recommended concentration, and again others used American garden brand, which meets the recommended threshold of acetic acid concentration for cervical cancer screening. Only 21.4% of participants used the correct acetic acid. This could be a factor determining the positivity rate as weaker concentrated acetic acid may fail to react with cervical dysplastic cells showing true outcome of VIA result.
On whether the percentage of acetic acid was indicated on the bottle, majority of respondents responded it was. It is important for screening to be done with brands that clearly show case manufacturers acetic acid concentration. The study went further to assess if the respondents were aware of the percentage of acetic acid recommended for VIA screening, Majority of the respondents 64.3% indicated that 2% concentrated acetic acid was sufficient for VIA, whereas the recommended percentage is 3-5%. The baseline knowledge showed that majority of the participants did not know the recommended acetic acid percentage concentration for VIA screening. On assessment of knowledge on how long a soaked swab with acetic acid should be applied on cervix, respondents noted it should be either be one minute, two minutes, three minutes or just random bathing of cervix with acetic acid. The recommended time for this application according to Kenya cervical cancer screening and treatment guidelines is 2 minutes. Majority of respondents 57.1% indicated that one minute was sufficient to apply the acetic acid on to the cervix. On the size of cotton applicator stick sufficient to apply sufficient acetic acid to cervix, respondents indicated that it should be either be big enough to cover cervical os or enough to cover the squamo columnar junction. The ideal practice is that a big enough cotton swab should cover the entire SCJ. On the eligible population for VIA cervical cancer screening in terms of age, majority 92.9% indicated that all women of reproductive age 15-49 years are eligible. The Kenya VIA screening guidelines recommends VIA screening age to be 25-49 years. On assessment of knowledge as to why the respondents thought women above 50 years are never screened for cervical cancer using the VIA method, half of the respondents indicated that their squamo columnar junction is not obvious, while others indicated its because Kenya cervical cancer screening guidelines on VIA indicate that age should not be screened and that at that age they should have papsmear. This shows that only half of the participants were aware of the actual reason as to why women above 50 years are not eligible for VIA. Women above 50 years do not have an obvious SCJ due to hormonal changes brought about by menopause. On the importance of visualizing SCJ before applying acetic acid, majority agreed it was important.
As the observational checklist on the procedure was being carried out, the major non conformity to procedural guidelines for VIA were noted. On verification of necessary instruments and supplies being ready, the performance generally was satisfactory at 58.3%, very satisfactory at 25% and neutral at 16.7%. Whereas the participants knew the supplies and instruments necessary, some had them in small quantities, like very small cotton applicator swabs that could not cover the SCJ, others had acetic acid in wrong concentrations. On the nature of light source used, the lights were mostly worn out non stable but functional light stands, others used their personal mobile gadget to provide lighting or natural lighting alone. Most of the respondents washed their hands before the procedure, which is a pointer for observation of infection prevention measure. It was noted that respondents inspection of external genitalia was mostly unsatisfying. On the step of inserting and adjusting the speculum to view the cervix, only 25% had very satisfactory technique. Mainly observations were lack of skillful technique to insert the speculum causing moderate discomfort to the clients. Respondents had very satisfying skill in fixing the speculum in an open position to visualize the entire cervix and satisfactory skills on moving the light source to clearly see the cervix. Once the speculum was in place in the vagina, majority of clients did not examine the cervix to determine if it was suspicious for cancer, hence they performed unsatisfactorily. On the use of light source to identify cervical os, the SCJ and the transformation zone, none of the participants were able to identify SCJ and transformation zone, hence the step was performed unsatisfactory. The researcher observed that the respondents were looking for the SCJ but they did not know how to visualize it. The identification of SCJ is a very important step to enable the VIA screening, interpretation of results and defining eligibility for treatment for those found to have precancerous lesions. On soaking the cotton swab in 3-5% acetic acid and applying to cervix for two minutes, again the performance of this step was dismal. None of the participant actually used a watch or clock to time themselves, they all estimated the time. Some participants just bathed the cervix within few seconds and were ready to interprete their findings.
On careful inspection of SCJ to check for any raised and thickened white plaques or acetowhite epithelium and if there was a lesion to determine if the lesion had clear boarders, if it touched SCJ while noting the size of the lesion, the observer noted that none of the health care provider had an understanding of what they were actually looking for to make diagnosis. All the participants performed very satisfactorily on removal of speculum and placing it in a bucket with chlorine solution for 10 minutes for decontamination. On inviting the clients to sit up and discuss her results and plan for follow-up, the observation here is that the results were not well explained, follow-up plan was not well communicated or right follow up plan given and sometimes results were being given casually as clients came off the couch. The majority of the respondents had challenges filling the MOH forms and registers that were available. This findings concur with those by Teoh, et al. that indicated that inadequate training contributed to lack of adherence to screening guidelines while VIA by trained and experienced female health workers is a safe, acceptable, and effective test that can save lives from cervical cancer even in remote areas with few resources as supported by Poli, et al. This is also in support of WHO [1] report which showed that absence of cervical cancer VIA screening and treatment guidelines can lead to lack of action and possibility that the diagnosis will be missed, thus increasing the possibility of overlooking patients who require repeated screening or investigation and treatment.
Conclusion
In the intervention phase, the Kenya MOH VIA screening training guidelines were used, supplemented with image and pictures for the purposes of the study from other sources, mainly JHPIEGO cervical cancer flash cards to help the participants get an in depth understanding of various outcomes of VIA treatment. Significantly, this enabled them to form a mental image even before they encountered real cervixes. Although, the MOH training curriculum for VIA is sufficient, however the aspect of clinical training for at least 4 days with the help of preceptors should be emphasized in this curriculum. This study has been able to demonstrate that combination of didactic training, clinical training and use of preceptors has the ability to pass the necessary VIA screening skills to healthcare workers in low resource set ups. Furthermore, VIA is very subjective in nature, thus the HCPs providing this service need frequent technical support and continuity of screening, to be able to maintain the skill. However, with good training and mentorship, then HCPs are able to make correct diagnosis of VIA. This will ensure that most precancerous lesions are identified and treated even before they become cancer, thus reducing the cervical cancer disease burden in Kenya. It is therefore important for facilities to adopt screen and treat approach to VIA, which ensures that women are treated the same day they are screened and thus reduction in instances of treatment defaulters or losses to follow-up. In the long term, effectiveness screening and treatment of precancerous lesions will reduce cervical cancer morbidity and mortality.
This study has observed that training HCPs in VIA increases their confidence in VIA procedure, are more likely to create awareness of the screening within the facility, hence increasing the VIA uptake. The researcher concludes that VIA training increases the adherence to VIA and cryotherapy guidelines as evidenced by the procedural observation of various steps in performance of these procedures, this in-turn increases the chance that the outcome of the procedure will be effective and reliable. In this study, baseline precancerous lesion positivity rate was 0.8% and after training and followup it was 14.1%. This study therefore concludes that proper adherence to VIA screening guideline improves VIA outcomes.
Recommendations
This study recommends the following:
i. The MOH VIA training guidelines and curriculum should be reviwed or updated to accommodate use of cervical images in training and the duration of training for VIA should be increased to at least 6-7 days. The Didactic training to take 2-3 days and clinical practice to take nothing short of 4 days. These changes can be effected by the national or county reproductive health policy makers.
ii. The MOH has incorporated cervical cancer-screening and treatment activities into the national health strategic plan, however, funds should be allocated to County governments to purchase the necessary equipment and supplies for VIA and cryotherapy.
iii. The MOH should offer cervical cancer screening and treatment free of charge in level 1 and 2 facilities, Just like other Reproductive health services are free.
iv. Preceptors should be part of clinical training because they mentor the trainees as they pass the relevant VIA skills to the participants.
v. MOH and county governments departments of health should ensure support supervision at least once per quarter to the health care workers trained on VIA.
vi. The health care facilities screening for VIA should be provided with job aids by MOH or supporting partners to help VIA providers to explain the procedure and possible outcomes to the clients, thereby increasing understanding and acceptance of VIA among clients.
References
- WHO (2012) Cervical Cancer Screening in developing countries report of a WHO consultation. World Health Organization, Geneva.
- WHO (2017) The World Health Organization's fight against cancer strategies that prevent, cure and care. World Health Organization.
- Ardahan M, Temel AB (2011) Visual inspection with acetic acid in cervical cancer screening. Cancer Nurs 34: 158-163.
- Adsul P, Manjunath N, Srinivas V, et al. (2017) Implementing community based cervical cancer screening programs using visual inspection with acetic acid in India: A systematic review. Cancer Epidemiol 49: 161-174.
- Asgary R, Cole H, Adongo P (2016) Acceptability and implementation challenges of smartphone-based training of community health nurses for visual inspection with acetic acid in ghana: mHealth and cervical cancer screening. BMJ Open 9: e030528.
- Veena S (2012) Manpower training for early Cervical Cancer detection. Acta Obstetricia and Gynecologica Scandinavica 91: 1124-1125.
- KDHS (2014) Kenya Demographic Health Survey Report.
- Kenyan Ministry of Health (2005) Reversing the trends: The second National Health Sector strategic plan of Kenya: Annual operation plan (NHSSP II) 2005-2010. Ministry of Health, Nairobi, Kenya.
- Division of Reproductive Health. National Cervical Cancer Prevention Program Action Plan 2005-2009.
- DHIS (2017) DHIS Annual Report KP 2017.
- Creswell JW, Plano Clark VL (2011) Designing and conducting mixed methods research (2nd edn), Sage Publications, Inc, Thousand Oaks, CA.
Corresponding Author
Evah MM, Doctor of Philosophy of Nursing Student, School of Nursing Sciences, University of Nairobi, P.O. Box: 30197, Nairobi 00100, Kenya, Tel +254723482308
Copyright
© 2022 Evah MM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.