A Narrative Review of Training Approaches to Address Low Volume High Risk Pediatric Resuscitation Skills
Abstract
The aim of this article is to present nursing professionals with clinical practice processes-aligned with current literature- that educators and nursing leaders at one institution have used to ensure that nurses are proficient with emergency response skills. The comprehensive overview of a combination of efforts to ensure nurses' proficiency with emergency response skills for a pediatric patient in cardiopulmonary arrest provides a logical context to narratively discuss present day literature on the topic. Critical reflection of lessons learned highlights (1) The necessity of collaboration and support from executive leadership and (2) The need for psychologically-safe, spaced practice with real-time feedback as essential factors to ensure the success of these types of educational initiatives. Evidence-based processes, framed using nursing care of the pediatric patient in cardiopulmonary arrest, extend practical advice and real-life examples that all nurses who face low volume high risk skills across a wide range of practice settings can use to inform training processes in their own organizations.
Introduction
It is critical for nurses to be efficacious in their ability to successfully respond to a medical emergency; however, depending on the setting (for example, pediatrics), some nurses could go years without needing to use these skills. Even though pediatric cardiopulmonary arrest is a low volume event, when it does happen, nurses and the entire resuscitation team need to be highly skilled to ensure the best patient outcomes. Over the last decade, resuscitation science has increasingly confirmed the importance of performing high-quality cardiopulmonary resuscitation (CPR) to attain an increase in survival from cardiac arrest [1-3]. Historically, resuscitation training has been offered every 2 years through formats such as the American Heart Association's (AHA) Basic Life Support (BLS) [4] and Pediatric Advanced Life Support (PALS) [5] certifications. However, more recent evidence suggests that one-time or biannual training may not be the optimal training frequency for supporting the ongoing translation of knowledge learned into clinical practice [6,7]. Mulholland and colleagues [6] sought to find evidence in support of their structured clinical question, "Should responders to paediatric arrests (population) receive resuscitation training (intervention) more frequently than national guidelines recommend (comparator) to ensure optimum retention of CPR skills (outcome)" [6] (p. 821). Upon critical appraisal of the body of literature that compared the effect of training frequency on CPR skill performance, authors concluded, "there is insufficient evidence to confirm an optimal training frequency... [however], annual resuscitation training is insufficient to maintain effective CPR skill performance" [6] (p.823). Similarly, Doymaz, et al. [8] assessed pediatric residents' retention of knowledge and clinical skills over time following AHA PALS [5] certification. Authors discovered that participants' clinical skills performance declined within the first 8 months after PALS certification and continued to decline as the time from the last certification increased. Further, Ciurzynski and colleagues [9] noted that "more frequent retraining other than the current widely accepted standard of biannual BLS certification, may help nurses increase their competence and comfort in their ability to be first responders to a child experiencing cardiopulmonary arrest" [9] (p.E1). As a result, the purpose of this article is to present nursing professionals with clinical practice processes-aligned with current literature-that one institution has used to ensure that nurses are proficient with emergency response skills. These evidence-based processes-although framed using nursing care of the pediatric patient in cardiopulmonary arrest-offer practical advice and real-life examples that all nurses who face low volume high risk skills across a wide range of practice settings can use to inform training processes in their own organizations.
Background
The clinical practice processes will be described using a chronological, team-based narrative that takes the reader on a journey over time as technology, resources, scientific evidence, and organizational priorities have evolved. The intention is to provide the reader with practical examples and lessons learned throughout these various approaches, which nurses could then tailor for implementation in any combination based on the unique needs of their local setting. Each exemplar is then discussed in the context of current evidence, with the goal of providing the reader with up-to-date resources based on present-day trends. This team's ongoing journey began while the first author was working as a clinical nurse specialist (CNS)/Nursing Professional Development (NPD) Educator in a Pediatric Intensive Care Unit (PICU) in the mid to late 1990s. Her interprofessional colleagues requested an educational series that focused on practicing team skills related to the most challenging resuscitation events that they might experience. Details about this early initiative, as well as subsequent efforts to address nurses' resuscitation skills, are described below in the context of current literature.
Deliberate Practice Low-Fidelity Mock "Mega-Codes"
This first educational program focused on deliberate practice, low-fidelity, mock "mega-codes". These were pre-scheduled based on mutually convenient times for interprofessional team members. Because they were planned well in advance, the NPD Educator was able to pre-assign roles and rotate team members as needed to provide both skill mastery as well as a challenging experience. Evidence supports the necessity to take on new challenges in order to improve performance in the healthcare setting [10]. The target audience for the mega-code practice sessions were PICU attending physicians/fellows, medical residents, nurses, respiratory therapists, and the nursing supervisor. Given this advanced audience, complex PICU cases were used so the team could simulate in situ requirements throughout the scenario. As a novice educator at the time, the CNS found using a toolkit with ready-to-use resources (e.g., McPhee [11] and Illinois Emergency Medical Services for Children [12]), including fully developed scenarios, extremely valuable. Throughout the hour-long session that provided continuing education credit for participants, team members used real-life equipment on a low-fidelity mannequin. Participants reported that practicing in a real patient room on a monthly basis using complex scenarios resulted in high levels of satisfaction and confidence in their ability to respond to a real patient in clinical distress. The perceptions of participants were validated using data from quality reviews following real resuscitation events at that institution, which are consistent with findings shared in the literature. For example, Hawani and colleagues [13] examined resuscitation skills and team performance during 82 simulated pediatric resuscitation events from 2016 to 2019 and concluded that in situ code simulation was a helpful way to enhance team performance and improve the quality of cardiac resuscitation. Further, Halm and Crespo [14] systematically examined published studies reporting resuscitation skill acquisition following a variety of training formats. Authors agree "practice helped nurses acquire, improve, and retain skills over time." [14] (p.516).
Intensive Care Unit (ICU)-focused, team-based resuscitation practice sessions were successful; however, many times patients deteriorate outside the ICU setting and it is imperative that first responders have the basic knowledge and skills to handle approximately the first 5 minutes until advanced help arrives. Internal audits of this institution's in-hospital-but outside the ICU-arrests, combined with observations during mock codes, exposed a need for BLS review among first responders. Additionally, educators believed it was important to assess the emergency response activation system processes (i.e., how to call for help) under usual conditions. Therefore, the next phase of the planned education along this journey focused on unannounced events in a variety of settings outside the ICU where any member of the healthcare team might come across a person in need of life-saving measures.
First Five Minutes Low-Fidelity Mock "Mini-Codes"
Like many other low volume high risk skills, nurses and other members of a healthcare team are often uncomfortable executing initial resuscitation steps-including chest compressions and bag-mask ventilation-as well as activating an emergency response team [15-17]. Unlike adult counterparts, pediatric resuscitation events do not usually result from a primary cardiac cause; instead, they are often the result of progressive respiratory failure or shock [1,2,18,19]. "In these patients, cardiac arrest is preceded by a variable period of deterioration, which eventually results in cardiopulmonary failure, bradycardia, and cardiac arrest." [19] (p.S92) Using the scientific evidence-"early appropriate therapy has the potential to improve a child's clinical status before it irreversibly deteriorates" [16] (p.e35)-as the impetus, the objective to orchestrate a first five minutes low-fidelity mock "mini-code" program was to offer clinicians an opportunity to participate in a situation that required immediate attention to the ABCs (airway, breathing, and circulation) of pediatric resuscitation.
Each session provided clinicians the opportunity to practice psychomotor skills required in the first five minutes of a pediatric resuscitation event, but it was also important to rehearse how to do so under typical workplace conditions, without forewarning. The decision to use an unannounced ("secret shopper") approach is supported as a best practice when one wants "...to evaluate the usual behaviors and performance of [the] staff by circumventing the Hawthorne effect to improve metrics..." [20]. The Hawthorne effect "refers to a tendency in some individuals to alter their behavior in response to their awareness of being observed" [21]. Use of a standardized scenario enacted across multiple encounters-routine in academiane [22,23] and emerging as an effective approach in the healthcare setting-can capture an accurate representation of usual care rather than participants' best behavior [20,24,25]. Supporters believe that this evidence-based strategy is an ideal approach for systematically addressing gaps in practice or processes [25]. Weiner and Schwartz [25] advocate the approach "to identify and address performance deficits through cycles of continuous quality improvement" [25] (p. 1186). Continuous quality improvement with respect to nurses' resuscitation skills was indeed the ongoing goal for the current authors. Unannounced to front-line staff members, NPD Educators selected dates, times, and specific clinical units by reaching out to the unit-based nursing leaders at the beginning of the anticipated shift. Clinical units that were uncharacteristically busy and/or had no physical space to place a low-fidelity mannequin were postponed or re-scheduled.
Brief bedside scenarios were initiated using one of the static (infant/child/adult) mannequins. One NPD Educator would act out the role of the parent/caregiver (i.e., the Standardized Patient) of a child in distress while the other NPD Educator assisted first responders as they worked through the few minutes until a full resuscitation team would typically arrive. Using a stopwatch and evaluation tool, NPD Educators discreetly monitored: (1) First responder actions (recognizes need for and elicits help, ABCs); (2) Second responder actions (states how to call a code, obtains automated external defibrillator [AED]/defibrillator, assists with CPR); and (3) Additional participant actions as available and necessary (brings un-opened code cart, places backboard, etc.). The entire scenario, including discussion and debriefing, was strictly limited to 10-15 minutes. Educators intentionally ended with positive affirmations and the dissemination of a Certificate of Participation to first and second responders and other participants.
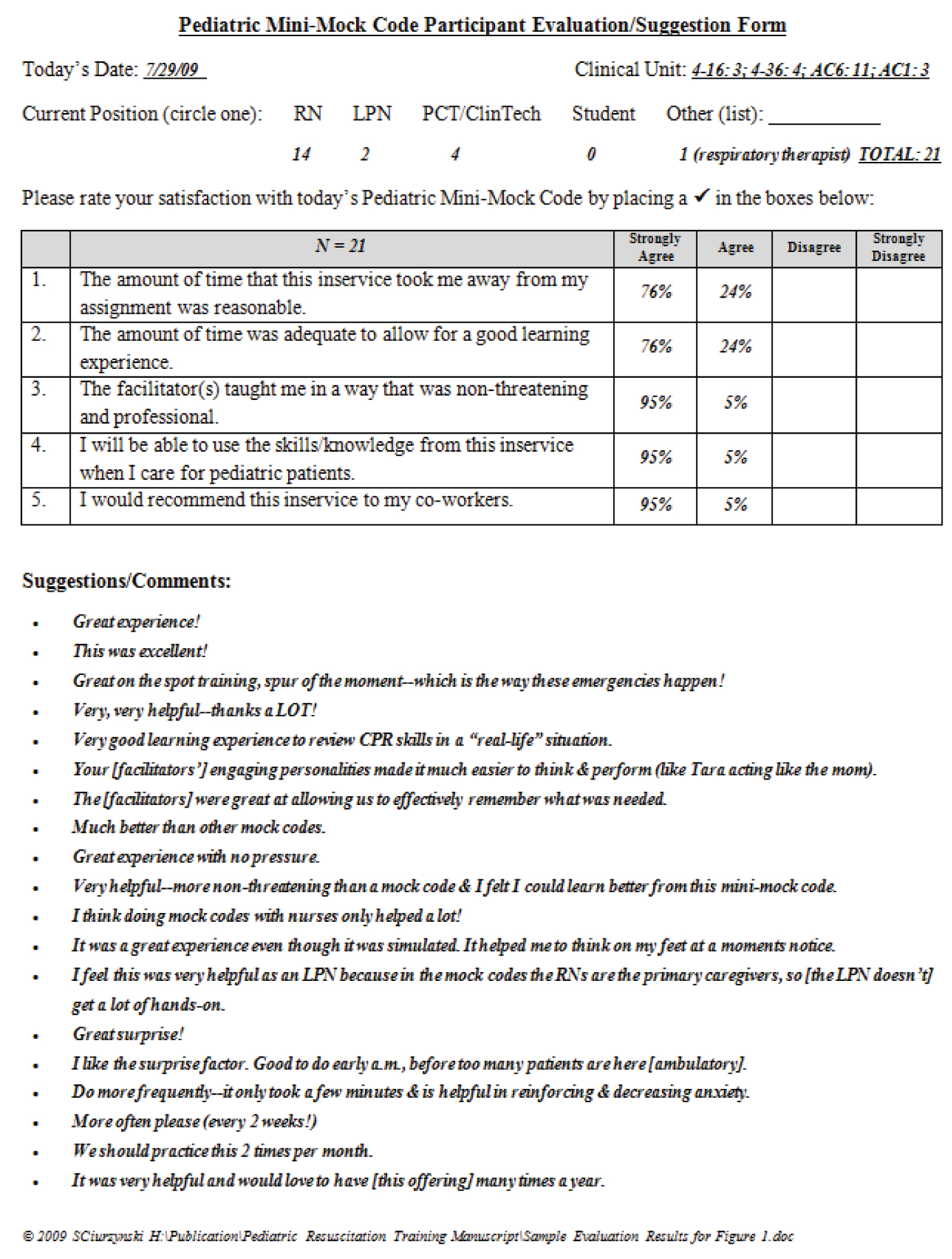
Outcomes and process measures were obtained using a variety of sources: (1) Data collected from an observation/feedback tool; (2) Documented time to recognition of and intervention for pediatric emergencies; (3) Observations of CPR quality (correct ratios, adequate depth and rate, correct hand placement); and (4) Reports of staff satisfaction and perceived helpfulness of the in-service as elicited during debriefing. Findings were shared with key stakeholders through unit-specific quarterly evaluation summaries provided to the Nurse Manager and CNS; and annual end of year evaluation summaries provided to the organization's Pediatric Resuscitation Committee. The overwhelming majority of participants rated this educational initiative as a positive experience (see Figure 1 as an example of aggregate feedback from participants that was shared with nursing leaders). Educators were able to report improvements in processes and outcomes over time across every clinical unit. Upon reflection, authors noted that one of the keys to this initiative's success was directly related to collaboration between the NPD Educators and the organization's nursing leadership team. For example, following one of the mock mini-codes in the ambulatory pediatric setting, NPD Educators discussed with the Nurse Manager the discovery of significant delays when administering rescue breaths due to absence of a bag-mask device at the patient's bedside. Some staff said they would administer mouth-to-mouth breathing while waiting for the bag-mask device to arrive on the code cart. The manager was able to use this data to justify the need for additional bag-mask devices or mouth-to-mouth barrier devices in every patient room in their ambulatory clinics. Another process that was improved as a direct result of this initiative included a change in house-wide policy based on nurses' pleas to store the AED/Defibrillator with the pads-cable attached (rather than the paddles-cable)-which prevents unnecessary delays in providing early defibrillation by first responders using the AED mode on the manual defibrillator. Finally, working with real-life emergency equipment (instead of always using a "mock code cart" for training) identified the need for practical solutions to other process delays. For example, during several of the mock mini-codes, nurses could not remember the hospital policy for selecting the appropriate weight-based AED/multifunction pads. Nurses were delighted when clinical unit leaders followed their recommendations to add clearly labeled bins for the 3 different sizes of multifunction pads to the standard emergency equipment.
Among the staff testimonials shared following this institution's roll out of these mock "mini-codes" were comments of praise (Figure 1) about how the unexpected nature of the simulation "helped [learners] to think on [their] feet at a moment's notice...which is the way these emergencies happen!" Wise and colleagues [17] also assessed clinician performance using unannounced resuscitation scenarios; however, they used a phased approach that included presentation of a video depicting the "ideal first 5 minutes of a code" prior to skill demonstration during a mock scenario in a free-standing academic pediatric hospital (p. 235). Likewise, Delac and colleagues [15] also focused resuscitation training efforts on what nurses needed to do in the first five minutes of a patient crisis. They implemented monthly, pre-scheduled, in situ mock codes with videotaped debriefing across medical-surgical and telemetry units. Authors reported that among the 250+ registered nurses who participated, they witnessed a 65% improvement in initiation of CPR within the first minute of arrival. Unlike the current author's low tech, low budget, 10-15 minute "mini-code" program described earlier, the latter example [15]-later confirmed by Pirie, et al. [26]-highlights the complexity and technical aspects surrounding a successful team-based simulation program. As nursing professionals are exploring options to meet the training needs for low volume, high risk resuscitation skills, it is important to consider availability of resources (such as video equipment and a high-fidelity mannequin), including time (unit staff, simulation center personnel, educators), as well as ongoing challenges with coordination across interprofessional colleagues' schedules.
High-Fidelity Simulation of Interprofessional Team-Based Mock Codes
High-fidelity simulation has emerged as an effective method of training healthcare professionals on clinical knowledge and skill performance among a variety of topics-such as interprofessional communication, patient handoff, and team dynamics [26-31]. Interprofessional simulation enables the opportunity to enhance awareness of each member's competence and contributions toward a team-based approach for delivery of high-quality healthcare [32]. The narrative of this institution's ongoing journey now brings the reader to 2008, where an interprofessional partnership (physician and NPD Educator) began co-leading bimonthly interprofessional mock codes. The locations for these mock codes alternated between a dedicated simulation space and in situ (in an unoccupied patient room on one of the pediatric inpatient units). These leaders and their colleagues were tasked with using newly-purchased high-fidelity simulators to enhance medical residents' educational programming in the context of an interprofessional team. Scenarios were created which highlighted various aspects of pediatric emergency response, and both the physician and NPD Educator actively participated in facilitating the debriefing afterward. Each mock code was one hour in length, with 10-15 minutes devoted to implementation of the scenario and 45-50 minutes devoted to debriefing. Participants were informed that each mock code was going to be videotaped for educational purposes. Recordings from the simulated resuscitation scenario were then used to review key learning objectives during the debriefing, which is consistent with practices widely described in the literature.
Debriefing practices: Of particular usefulness for current readers is "Standards of Best Practice: Simulation Standard VI: The Debriefing Process" authored by Decker, et al. [33], with the key message that "Research provides evidence that the debriefing process is the most important component of a simulation-based learning experience". (p. S27) Additionally, Waznonis published findings from (1) An integrative review of the literature that examined various debriefing methods and evaluations for simulation debriefing [34]; and (2) A mixed-methods study of simulation debriefing practices among nursing faculty [35]. She noted that educators used a variety of options-such as videos, scripts, worksheets, media (Internet chat, discussion boards, blogs, etc.), lectures, games, storytelling, peer feedback, educator feedback, multidisciplinary feedback, simulator log feedback, self-assessment, and verbal or written debriefings [35] She concluded, "regardless of the methods and approaches to debriefing, evaluation of the effectiveness of the debriefing should occur regularly ([35], p118)."
Similarly, Lee and colleagues [30], in their systematic review and meta-analysis, aspired to determine the effectiveness of debriefing methods that can maximize learning outcomes when simulation was used in nursing education. Through the systematic review of 18 studies and meta-analysis of 7 studies, authors concluded that "structured debriefings between learners and instructors are vital in simulation education, as they can improve learners' learning outcomes, including performance skills, critical thinking, clinical reasoning, clinical judgment, satisfaction with the simulation and debriefing, problem solving, and debriefing quality [30] (p.11).
Psychological safety: Although the aforementioned bimonthly interprofessional mock codes were well received (as evidenced by paper evaluations that were completed at the end of each simulation session) by medical residents in the local setting, several nurses expressed substantial hesitation when urged to participate. Co-leaders noted consistently lower participation rates among nurses-despite ongoing offers to provide patient coverage during the training times. Educators subsequently learned that nurses were anxious about appearing unskilled in performing low volume resuscitation tasks in front of their nursing peers and physician colleagues. This local discovery has also been subsequently described in the literature. Specifically, nurses' desire for a culture of psychological safety was similarly described by Connolly, et al. [28] during their synthesis of learners' experiences of interprofessional simulation; and by Waznonis [34], in her integrative review of the literature, noting the availability of instruments to measure an environment of psychological safety (privacy, confidentiality, trust/safety, and attitudes) during simulation debriefing. Similarly, Delac and fellow clinical educators [15] observed actual resuscitation events over the years, noting that nurses often responded "...with emotions such as fear, anxiety, [and] confusion, which result [ed] in immobilization" [15] (p.244-245). Interestingly, they discovered that "...it was not exclusively the new or recent graduate nurses who were anxious during a code. Equally anxious were the highly skilled and proficient nurses" [15] (p. 245-246). Reducing nurses' anxiety surrounding emergency response is particularly important because authors discovered "...the fight or flight response experienced by most nurses resulted in delays initiating cardiopulmonary resuscitation, regardless of their years of experience or background" [15] (p. 245-246).
With the knowledge that local nurses were uncomfortable practicing essential low volume high risk skills in front of physician colleagues, NPD Educators recognized the need for additional nursing-specific training that focused on ensuring a culture of psychological safety while practicing nursing-specific skills during a pediatric emergency.
New Hire Orientation to Nursing-Specific Resuscitation Skills
Nurses who care for children need to be prepared for what to do in the event of a pediatric emergency. At this institution, all nurses who cared for children were required to attend a 3-day pediatric service orientation program, of which the third day was dedicated entirely to recognition and management of the decompensating pediatric patient. Although the specific content for the day was updated on an as-needed basis to meet ongoing educational needs, the basic format for the day was: (1) Didactic content to introduce the pediatric rapid response team processes as well as an overview of basic life support and pediatric emergency response; (2) Three independent skills stations (pediatric airway management, code cart review, and AED/defibrillator use); and (3) A return-demonstration of resuscitation skills rehearsed throughout two pediatric mock code scenarios. The two pediatric mock codes highlighted the importance of effective team dynamics when executing an organized emergency response and was extremely well-received by nursing attendees. Throughout the entire resuscitation day, educators intentionally maintained a psychologically safe learning atmosphere and offered positive affirmations and encouragement to learners as they practiced various skills. This new hire orientation to pediatric emergency response was initially followed up with completion of BLS for general care nurses and PALS for ICU nurses; however, early recognition of and team-based response to a deteriorating patient outside the ICU setting remained an area of critical need. Consequently, an additional layer of team-based training was warranted.
Team-Based Training in Early Assessment, Recognition, and Stabilization
The Pediatric Emergency Assessment, Recognition, and Stabilization (PEARS) course was first available in late 2007 [36]. The course was developed by the American Heart Association and co-branded with the American Academy of Pediatrics [37], with a goal to fill a training gap that existed between the Basic Life Support course (which focuses on basic CPR skills for infants and children) [4] and the Pediatric Advanced Life Support course (targeting critical care providers) [5]. The PEARS course concentrates specifically on assessment and early recognition of a child who is having signs of distress or failure and treating them until advanced life support is available-supporting the concept that early recognition is key to preventing tragic outcomes for the patient [37].
In September 2008, the AHA approved designation for the local organization's training center to provide PALS and PEARS courses. While the PALS course was already a requirement for the pediatric emergency department and pediatric critical care nurses, the PEARS course was a brand-new initiative. Leaders instituted an expectation for all nurses caring for pediatric patients on general care units-including inpatient, outpatient, and specialty areas (rehabilitation and the cancer center)-to successfully complete this course. Initial efforts included: (1) The development of institutional policies; (2) Processes surrounding registration, compliance monitoring, and equipment; and (3) Training qualified instructors to teach the PEARS courses. The first PEARS class was held in July 2009, and the program has grown exponentially over the years. Learners who have taken the course have consistently expressed positive feedback through course evaluations and report that they feel better prepared to respond in an urgent or emergent pediatric situation. In addition, those which work in a non-critical care environment who had previously taken the PALS course find the PEARS content more applicable to their patient population and relevant to their daily practice.
The combination of nursing-specific new hire orientation skills, PEARS (or PALS) certification, and occasional practice at interprofessional mock codes, positively impacted nurses' ability to effectively respond to a pediatric patient in distress or failure. However, due to the distinct differences in epidemiology, pathophysiology, and common etiologies of pediatric cardiac arrest from adult and neonatal cardiac arrest, [19] many hospital clinicians outside the ICU shared that they did not retain confidence in their ability to perform the technical skills required if a deteriorating child could not be stabilized (i.e., progressed to full cardiac arrest).
Resuscitation Skills Practice Using a Real-Time Feedback Device
Between 2014 and 2015, nurses on a pediatric general care unit expressed to their NPD Educator concern about their ability to respond to a pediatric medical emergency. The concern was time-sensitive due to an upcoming move of the acute inpatient pediatric units into a new Children's Tower in 2015. This move temporarily placed the units at a significant distance from the pediatric ICUs, with an anticipated 5 to 10 minute delay in advanced responders arriving at a resuscitation event in the new building. Specifically, nurses conveyed concerns regarding their ability to provide high-quality CPR, utilize the defibrillator/AED without the presence of an advanced provider, and draw up initial emergency medications. The nurses' concerns were valid based on evidence published by the International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations for Pediatric Life Support that longer time intervals between start of CPR are associated with lower survival [18].
In the spring of 2015, the unit's NPD Educator and service line's Pediatric Service Educator developed a performance improvement project to improve the bedside nurses' proficiency in responding to a pediatric cardiac arrest on a general care pediatric inpatient unit. The performance improvement project involved 21 registered nurses (100% of that unit's nurses) participating in a 30-minute hands-on training session that focused on the following three metrics: (1) Quality of CPR, (2) Early defibrillation via the automatic external defibrillator (AED), and (3) Drawing up the first weight-based pediatric code medication (i.e., epinephrine). These same nurses attended a re-training session 6 months later focusing on the same content along with evaluation of knowledge and skill retention.
The nurses were randomly grouped into pairs. Each pair of nurses attended the 30-minute session consisting of a simulation scenario and measurement of CPR performance using software that provided real-time feedback of the quality of the CPR [38]. As the scenario continued, the nurses demonstrated proper defibrillator pad placement, setting the defibrillator to the AED function, and drawing up an initial weight-based dose of epinephrine. Knowledge of resuscitation was assessed by having nurses complete an 8-item knowledge questionnaire pre- and post-scenario. Results (with full report published by Ciurzynski, et al. [9]) illustrated that following attendance at the initial training, nurses' resuscitation knowledge improved a mean of 20 points from pre-test to post-test, p < 0.001. Six months later, however, this new knowledge was not retained, with scores decreasing from 97% to 85%, p < 0.001. Overall CPR performance skills increased from 89% to 94% during the initial training with use of the feedback device. This performance skill was maintained at 94% at 6 months despite the knowledge scores declining.
This project was subsequently expanded to include the three other general care pediatric inpatient units with positive feedback shared among nursing participants. Nurses on two separate occasions applied these skills with successful resuscitation of real pediatric patients, demonstrating the translation of a simulated practice of skills to the real world clinical setting; in particular, reduced anxiety and improved performance during actual events. Delac, et al. [15] reported that nurses who participated in a simulation mock code followed by videotaped debriefing reported improved confidence in initiating first responder interventions and their ability to use emergency equipment prior to arrival of advanced responders. Similarly, Couloures and Allen [29] simulated high-acuity and low frequency events for pediatric residents and discovered improvements in confidence, rhythm recognition, and resuscitation performance during actual events.
Resuscitation performance has also been studied by Donoghue and colleagues, [39] who conducted a prospective observational study from September 2016 to March 2019 to describe chest compression quality by individual providers in two pediatric emergency departments. In addition to compression monitor output (similar to the training feedback described above), authors reviewed videos from actual pediatric cardiac arrests during the study period. Findings confirm the vulnerability of healthcare professionals expected to perform low volume, high risk skills, suboptimal CPR quality. However, authors concluded, "[this] data collection methodology holds promise for longitudinally measuring the impact of education and quality improvement work on CPR performance in children, providing a direct link between training and performance at the level of individual providers" [39] (p.43).
Despite all of the benefits of simulated training presented thus far, an important consideration relates to resource allocation (workload demands). Pirie and colleagues [26] developed a mandatory simulation competency based procedural and resuscitation program in pediatric emergency medicine (CBME). Authors state, "Scheduling of both participants and instructors was and continues to be a challenge. Given the need to cover the clinical workload on CBME course days and individual's academic responsibilities, developing a balanced schedule was difficult" [26] (p.5). Another relatable challenge mentioned in this study was the limited number of instructors who have either simulation expertise or technical expertise. These workload demands are not unique; in fact, the current authors, like countless others, have needed to balance competing healthcare priorities amidst busy schedules while attempting to provide training on off-shifts and weekends. Not surprising was their eagerness to participate when new automated resuscitation technology became available at the local organization.
Self-Directed Spaced Practice Using Automated Resuscitation Technology
In 2015, the organization was introduced to the Resuscitation Quality Improvement Program (RQI)®, which is an innovative approach to maintain CPR competency [40,41]. The program was developed in a collaborative effort between the AHA and Laerdal Medical in response to the 2010 AHA guidelines, recommending a competency-based approach to resuscitation skills [42]. The AHA suggested more frequent assessment and skills training rather than the traditional 2-year certification. The RQI® program provides learners with low-dose, high frequency (i.e., every 3 months) exposure to BLS [4] and Advanced Life Support (ALS) [5] education [40]. This innovative educational approach utilizes automated simulation mannequins [43-45] to provide performance feedback on CPR skills, in combination with self-directed online e-learning content on a quarterly basis [40].
After a 2-year trial in this organization's adult critical care area, the RQI® program was implemented in the children's hospital in July 2017; the final chronicle in this paper's narrative journey. Those participating included providers (attending/fellow physicians, medical residents, nurse practitioners and physician assistants), nurses, and respiratory therapists. Part of the success of this program is that it allows staff to stay at the bedside, caring for patients, rather than pulling them away to attend a class. The simulation mannequins [43-45] and required equipment (i.e., bag-mask devices, step stool, and laptop) are packaged in an all-inclusive cart, which allows for easy transportation from unit to unit. Nursing Professional Development Educators worked with hospital leaders to determine a cart schedule to ensure that all staff had access to the carts on a routine basis. Due to the large size of this medical center, the carts are rotated on a weekly basis so a cart is located on each unit for at least 2-3 weeks/quarter. In addition, one cart is always located in a private room where it can be accessed 24/7 for those individuals who may prefer to complete the skills in a non-public location. The online, didactic components can be accessed from any computer that meets the program's technical requirements. Each quarter, RQI® participants receive an email notifying them that new learning is available. In addition, reminders are sent at pre-determined intervals for those who have not yet completed the quarterly requirements. Nurse Managers and supervisors have access to the RQI® system and can review compliance reports at any given time. Additionally, automated compliance notifications are sent on a quarterly basis to individuals who are not compliant and Nurse Managers or supervisors.
Beyond providing real-time feedback on resuscitation quality to the clinician and monitoring training compliance, there is also an opportunity to observe and track CPR skills performance and knowledge over time using RQI® analytics [40,41]. The level of detail provided in the reports allows the NPD educator to develop focused and individualized training when indicated. Furthermore, there are ongoing efforts to examine the relationship between more frequent training through use of the RQI® program and the potential impact on patient outcomes.
To date, emerging evidence suggests that this novel approach to resuscitation training has the potential to produce the desired outcomes while mitigating the challenges (e.g., time, space, bulky/complex equipment, available experts, and psychological safety) in busy healthcare settings. For example, Donoghue and colleagues [46] conducted a prospective observational study using the RQI® program, with the goal to measure CPR performance by emergency department providers in a children's hospital during real patient events and to examine the direct relationship with their CPR training. Over a 15-month study period, 159 providers completed four consecutive RQI® sessions to practice low volume, high-risk resuscitation skills; and 28 children received chest compressions under video-recorded conditions. Authors used a combination of video review and chest compression monitor devices to examine 49 observations of chest compressions performed by 32 RQI®-trained providers in the pediatric emergency department setting. Findings confirm that high-frequency CPR skill training results in "improved performance during training sessions for all skills; [and] a significant association was found between number of sessions and adherence to compression rate guidelines during real patient events" [46] (p.1).
Critical Reflection on Lessons Learned Along this Journey
Upon reflection about the key successes afforded the authors throughout their pursuit of excellence related to resuscitation skills across their organization, two main themes emerged. First is the necessity of establishing and sustaining interprofessional partnerships among key leaders with shared vision. Secondly, as clearly evident in this narrative review, ongoing spaced practice with real-time feedback is essential to ensure optimal outcomes when healthcare team members are faced with low volume high risk skills. Each of these points are discussed below, with practical recommendations for nursing professionals integrated.
Partnership with key leaders
Throughout this paper, the authors have discussed various methods for implementing pediatric resuscitation skills training over the past twenty years. It is critical to point out that none of these efforts would have been successful without the executive leadership support provided by the Chief Nursing Officer (CNO). For example, it was through the strong partnership and open dialogue between the CNO and the NPD Pediatric Service Educator(s) where essential institutional support was provided to ensure the successful implementation of the performance improvement project with 6-month practice sessions using real-time feedback. There are countless competing initiatives for time and resources provided by front-line nursing staff, and executive leadership support is critical for the successful implementation of educational initiatives designed to enhance nurses' competence and confidence in their provision of nursing care.
Responding to the ongoing and ever-developing needs of the nursing staff caring for patients in an acute care pediatric hospital setting is one of the fundamental responsibilities of the CNO. Ensuring that pertinent clinical care issues are identified and addressed, key stakeholders are actively involved not only in problem-identification but also in seeking appropriate solutions and navigating consensus-building discussions as essential elements of this tapestry. Developing nursing leaders within the organizational structure to explore all opportunities to best prepare front line nursing staff to provide the most up-to-date, evidence-based care of the pediatric patient population is a central tenet of a strong leadership structure.
Incorporating the AHA PEARS [36] class into the required elements of the nursing and Advanced Practice Provider (i.e., Nurse Practitioners and Physician Assistants) staff caring for pediatric patients across the institution-not only within the children's hospital, but also across the larger medical center-was a relatively easy discussion to navigate. Adopting the PEARS course as required educational content would ensure that all front-line care providers had the pediatric assessment knowledge necessary for timely recognition and appropriate intervention for a pediatric patient who exhibited signs of clinical deterioration. The addition of this educational requirement into compulsory procedures involved the hiring of a PALS/PEARS Coordinator, as well as the identification and recruitment of pediatric instructors who had the knowledge and skills to teach course content. This was strongly endorsed at the Pediatric Nursing Leadership level. Instructors are supported at the pediatric unit level-through compensation for their time and, whenever possible, incorporating this responsibility into their standard hours. The didactic time for mandatory course completion every 2 years was able to be accommodated into the pre-existing educational time built into the non-productive time for each full-time nursing equivalent (FTE) and was supported at the Nursing Practice Executive level within the institution.
As previously mentioned, the children's hospital was poised to move into a newly-constructed tower in the summer of 2015. The two-phased approach for the move-in which the general care units and the PICU would be housed in separate but connected buildings for slightly over 2 years-created some understandable anxiety for front-line nurses, both on the general care floors as well as in the PICU. Developing a curriculum that would focus on the essential elements of provision of care for approximately the first 5 minutes of a pediatric resuscitation strengthened the confidence of the bedside nursing staff that they had the knowledge and skills necessary to best support the patient until the pediatric code team arrived.
Spaced practice with feedback is essential to ensure optimal outcomes
Guidelines set forth by the AHA stress the importance of provision of mock code training and assistive device technology for ensuring optimal patient outcomes related to in-hospital cardiac arrest [42]. Bhanji and colleagues [42] reported that "improving healthcare professionals' ability to recognize and respond to patients at risk of cardiac arrest; improving resuscitation performance (including CPR); and ensuring continuous quality improvement activities to optimize future performance through targeted education" were all essential components of resuscitation education in the healthcare setting [42] (p. S561). The expression spaced practice has been used to refer to training delivered in multiple separate sessions over a period of time, where the content is either distributed across multiple sessions or is practiced repetitively [47]. At the current institution, authors have demonstrated an ongoing commitment to these tenets through provision of mock codes, new hire orientation resuscitation skills training, mandatory PEARS training for healthcare professionals caring for children outside a critical care environment, 6-month practice sessions using a real-time feedback device, and incumbent staff 3-month practice through RQI® technology.
There is emerging evidence that suggests a correlation between hospitals that offer more in-depth mock codes and patient survival following in-hospital cardiac arrest (IHCA) [48]. Nallamothus and colleagues [48] conducted structured interviews with interprofessional team members at top-performing hospitals within the United States who had high IHCA survival rates, who described their mock code experiences as "(1) Unplanned and held on a regular basis, (2) Conducted in actual patient rooms rather than simulated environments, (3) Multidisciplinary, and (4) Included structured post-debriefing" [48] (p. 160). The current article demonstrates an evolution of pediatric resuscitation skills training which includes components of all four of these findings. Future efforts should focus on assessing the effect of mock code training efforts' on patient survival outcomes, both within this institution as well as at other institutions.
Conclusion
This article has presented nursing professionals with clinical practice processes-aligned with current literature-that educators and nursing leaders at one institution have used to ensure that nurses are proficient with emergency response skills. These evidence-based processes, framed using nursing care of the pediatric patient in cardiopulmonary arrest, extend practical advice and real-life examples that all nurses who face low volume high risk skills across a wide range of practice settings can use to inform training processes in their own organizations. The comprehensive overview of a combination of efforts to ensure nurses' proficiency with emergency response skills for a pediatric patient in cardiopulmonary arrest provided a logical context to discuss present day literature on the topic. Critical reflection of lessons learned throughout the pursuit of excellence related to resuscitation skills highlights (1) The necessity of collaboration and support from executive leadership and (2) The need for psychologically-safe, spaced practice with real-time feedback as essential factors to ensure the success of these types of educational initiatives.
References
- Soar J, Maconochie I, Wyckoff MH, et al. (2019) International consensus on cardiopulmonary resuscitation and emergency cardiovascular support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Circulation 140: e826-e880.
- Nolan JP, Maconochie I, Soar J, et al. (2020) Executive summary 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 156: A1-A22.
- Kaplow R, Cosper P, Snider R, et al. (2020) Impact of CPR quality and adherence to advanced cardiac life support guidelines on patient outcomes in in-hospital cardiac arrest. AACN Adv Crit Care 31: 401-409.
- (2021) Basic Life Support (BLS). American Heart Association.
- (2021) AHA pediatric training for healthcare providers: Pediatric advanced life support (PALS). American Heart Association.
- Mulholland M, Molloy S, Coulter P, et al. (2021) How frequently should paediatric cardiopulmonary resuscitation skills be taught? Arch Dis Child 106: 821-824.
- Su E, Schmidt TA, Mann NC, et al. (2000) A randomized controlled trial to assess decay in acquired knowledge among paramedics completing a pediatric resuscitation course. Acad Emerg Med 7: 779-786.
- Doymaz S, Rizvi M, Orsi M, et al. (2019) How prepared are pediatric residents for pediatric emergencies: Is pediatric advanced life support certification every 2 years adequate? Glob Pediatr Health 6: 1-8.
- Ciurzynski SM, Gottfried JA, Pietraszewski J, et al. (2017) Impact of training frequency on nurses' pediatric resuscitation skills. J Nurses Prof Dev 33: E1-E7.
- Williams D, Ledger A (2020) Starting work as a doctor: Challenge is essential. Clin Teach 17: 36-40.
- McPhee K (2018) Deliberate practice mock codes for new graduate nurse. J Nurses Prof Dev 34: 348-351.
- (2012) Pediatric mock code toolkit. (2nd edn), Illinois Emergency Medical Services for Children (EMSC).
- Hazwani TR, Harder N, Shaheen NA, et al. (2020) Effect of a pediatric mock code simulation program on resuscitation skills and team performance. Clin Simul Nurs 44: 42-49.
- Halm MA, Crespo C (2018) Acquisition and retention of resuscitation knowledge and skills: What's practice have to do with it? Am J Crit Care 27: 513-517.
- Delac K, Blazier D, Daniel L, et al. (2013) Five alive: Using mock code simulation to improve responder performance during the first 5 minutes of a code. Crit Care Nurs Q 36: 244-250.
- Hunt EA, Walker AR, Shaffner DH, et al. (2008) Simulation of in-hospital pediatric medical emergencies and cardiopulmonary arrests: Highlighting the importance of the first 5 minutes. Pediatrics 121: e34-e43.
- Wise KM, Zinkan JL, Rutledge C, et al. (2020) Development of a "First Five Minutes" program to improve staff response to pediatric codes. Am J Crit Care 29: 233-236.
- Maconochie IK, Aickin R, Hazinski MF, et al. (2020) Pediatric life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations, Resuscitation 156: A120-A155.
- Topjian AA, Raymond TT, Atkins D, et al. (2020) Part 4: Pediatric basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation.142: S469-S523.
- Chung AS, Bogoch S, Mody S, et al. (2019) Videotaped unannounced standardized patient encounters to evaluate interpersonal and communication skills in emergency medicine residents. AEM Educ Train 4: 419-422.
- Prera A (2021) What is the Hawthorne effect. Simply Psychology.
- Kurz JM, Mahoney K, Martin-Plank L, et al. (2019) Objective structured clinical examination and advanced practice nursing students. J Prof Nurs 25: 186-191.
- Hickey MT (2021) Objective structured clinical examinations as a method of competency evaluation in a primary care nurse practitioner program. Nurse Educ 46: 317-321.
- Glassman PA, Luck J, O'Gara EM, et al. (2000) Using standardized patients to measure quality: Evidence from the literature and a prospective study. Jt Comm J Qual Improv 26: 644-653.
- Weiner SJ, Schwartz A (2014) Directly observed care: Can unannounced standardized patients address a gap in performance measurement? J Gen Intern Med 29: 1183-1187.
- Pirie J, Fayyaz J, Gharib M, et al. (2016) Development and implementation of a novel, mandatory competency-based medical education simulation program for pediatric emergency medicine faculty. Adv Simul 6: 17.
- Andreatta P, Saxton E, Thompson M, et al. (2011) Simulation-based mock codes significantly correlate with improved pediatric patient cardiopulmonary arrest survival rates. Pediatr Crit Care Med 12: 33-38.
- Connolly F, De Brún A, McAuliffe E (2021) A narrative synthesis of learners' experiences of barriers and facilitators related to effective interprofessional simulation. J Interprof Care 1-12.
- Couloures KG, Allen C (2017) Use of simulation to improve cardiopulmonary resuscitation performance and code team communication for pediatric residents. MedEdPORTAL 13: 10555.
- Lee JH, Lee H, Kim S, et al. (2020) Debriefing methods and learning outcomes in simulation nursing education: A systematic review and meta-analysis. Nurse Educ Today 87: 104345.
- Niu Y, Liu T, Li K, et al. (2021) Effectiveness of simulation debriefing methods in nursing education: A systematic review and meta-analysis. Nurse Educ Today 107: 105113.
- Lazzara EH, Benishek LE, Dietz AS, et al. (2014) Eight critical factors in creating and implementing a successful simulation program. Jt Comm J Qual Patient Saf 40: 21-29.
- Decker S, Fey M, Sideras S, et al. (2013) Standards of best practice: Simulation standard VI: The debriefing process. Clin Simul Nurs 9: S27-S29.
- Waznonis AR (2014) Methods and evaluations for simulation debriefing in nursing education. J Nurs Educ 53: 459-465.
- Waznonis AR (2015) Simulation debriefing practices in traditional baccalaureate nursing programs: National survey results. Clin Simul Nurs 11: 110-119.
- (2021) PEARS® Pediatric emergency assessment, recognition and stabilization. American Heart Association.
- Ralston ME, Zaritsky AL (2009) New opportunity to improve pediatric emergency preparedness: Pediatric emergency assessment, recognition, and stabilization course. Pediatrics 123: 578-580.
- Laerdal Medical (2021) Resusci anne advanced skill trainer: Mobile ALS training for advanced healthcare professionals.
- Donoghue AJ, Myers S, Kerrey B, et al. (2020) Analysis of CPR quality by individual providers in the pediatric emergency department. Resuscitation 153: 37-44.
- (2021) Resuscitation quality improvement program (RQI)®. American Heart Association.
- (2021) RQI®: Resuscitation quality improvement. An American heart association and laerdal program. RQI Partners.
- Bhanji F, Mancini ME, Sinz E, et al. (2010) Part 16: Education, implementation, and teams: 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 122: S920-S933.
- Laerdal Medical (2021) Resusci baby QCPR: High-performance training for infant resuscitation.
- Laerdal Medical (2021) Resusci junior QCPR: High-Performance training for pediatric resuscitation.
- Laerdal Medical (2021) Resusci anne QCPR: High-performance CPR skills for first responders.
- Donoghue A, Heard D, Griffin R, et al. (2021) Longitudinal effect of high frequency training on CPR performance during simulated and actual pediatric cardiac arrest. Resuscitation Plus 6: 100117.
- Cheng A, Nadkarni VM, Mancini MB, et al. (2018) Resuscitation education science: Educational strategies to improve outcomes from cardiac arrest: A scientific statement from the American Heart Association. Circulation 138: e82-e122.
- Nallamothu BK, Guetterman TC, Harrod M, et al. (2018) How do resuscitation teams at top-performing hospitals for in-hospital cardiac arrest succeed? Circulation 138: 154-163.
Corresponding Author
Susan M Ciurzynski, PhD, RN NPD-BC, MS, VCE, FNAP, Professor of Clinical Nursing, Director of Clinical Scholarship, and Assistant Director, Doctor of Nursing Practice (DNP) Program, University of Rochester School of Nursing, Elmwood Ave, Rochester, NY 14642, USA; Senior Advanced Practice Registered Nurse, Golisano Children's Hospital, University of Rochester Medical Center, Elmwood Ave, Rochester, NY 14642, USA, Tel: 1-585-276-6068, Fax: 1-585-273-1270.
Copyright
© 2022 Ciurzynski SM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.