Reframing Therapeutic Nursing Relationships in Acute Care Using the CTNR-A Model
Abstract
Background: A high nurse-patient ratio exists in acute care settings in which a team-based care delivery is utilized to optimize patient care flow efficiency. Within this structure, nurse-patient relationships exist in an individualistic context. Over time, nursing has drifted towards a more task-focused approach which challenges nurses to consistently achieve relational aspects of care in a team-based nursing care delivery model.
Aim: Using an innovative model of nursing care, the aim is to cultivate and redefine collaborative therapeutic nurse-patient relationships within a complex acute care environment where nursing teams' real and/or potential barriers that can impede the caring processes.
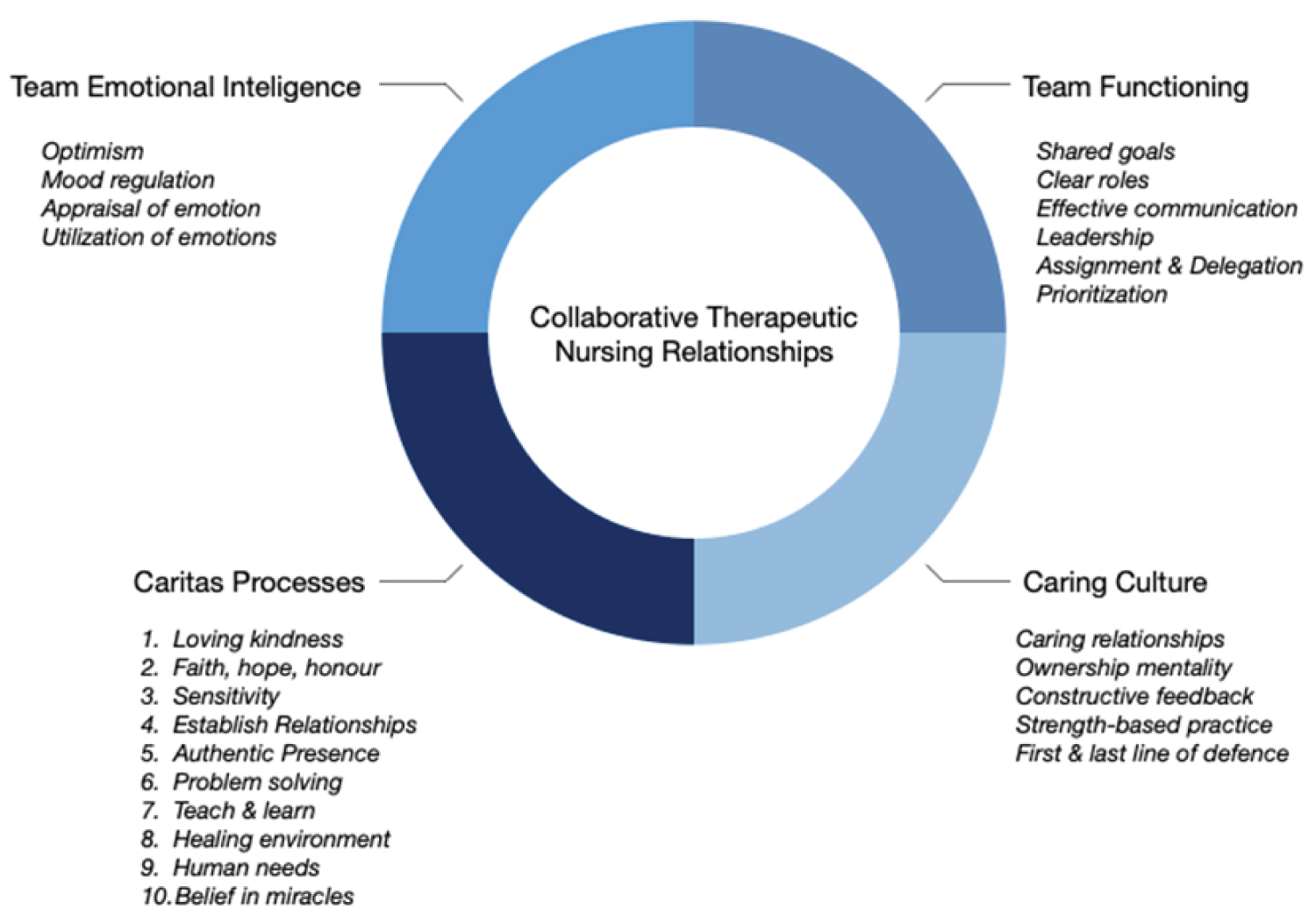
Method: The Collaborative Therapeutic Nursing Relationships Model for Acute Care (CTNR-A) endeavors to blend team-based care principles with Watson's theory of transpersonal caring within acute care settings to conceptualize and strengthen the nurse-patient relationship. The model integrates four essential components: Team emotional intelligence, team functioning, caritas processes, and caring culture. Beyond the merit of each individual concept, this brings together all four concepts under one framework that establishes a clear direction on how to promote open dialogue towards meaningful care amongst nursing teams in complex acute care environments.
Conclusion: The nature of team-based acute care nursing can overshadow the meaningful therapeutic nurse-patient relationship that is influenced by a conflicting caring culture and task-orientation. Collaborative Therapeutic Nursing Relationships Model for Acute Care (CTNR-A) provides a valuable opportunity to rejuvenate and re-align nursing to a culture of 'caring' in these most difficult times.
Keywords
Nursing, Therapeutic relationship, Watson's theory of caring, Team, Acute care, Relational caring
Introduction
Acute care hospital nursing encompasses the largest percentage of nursing's workforce. In Canada, there are over 400,000 registered (RN) and licensed practical nurses (LPN) and with 58.5% working in acute care hospital settings [1]. A high nurse-patient ratio exists in this clinical setting. Therefore, a team-based care delivery model is utilized to optimize patient care flow efficiency yet risks a task-focused approach to patient care. By focusing on labor division, relational aspects of care are often missed, overlooked, or neglected [2]. Seeing the patient and not just the diagnosis is a continued challenge in this environment. Johnson describes that "patients have become invisible…caring and compassion have been overshadowed by the science of nursing" [3]. Traditional nurse-patient relationships exist within an individualistic context, or "the autonomous one-to-one relationship between the health care provider and patient." [4]. The individualized orientation of relationships presents a challenge for team-based models to consistently achieve relational aspects of care where nursing care is shared and team dynamics are involved [4].
Watson's transpersonal caring theory emerged as a middle-range theory and quickly became the groundwork of caring science in nursing. It emphasizes a transpersonal caring relationship and caring moments between nurse and patient to guide comprehensive biopsychosocial patient care [5]. Regrettably, over time, the caring tenets of some nursing theorists have drifted in practice. Innovations in treatments, technology, and science have caused a fundamental shift in nurses' provision of care to become focused on checklists and procedures [6].
This discussion aims to explore the barriers to therapeutic nurse-patient relationships within acute care nursing teams. The authors will present an introductory model titled Collaborative Therapeutic Nursing Relationships Model for Acute Care (CTNR-A) stemming from an innovative paradigm that strives to blend team-based care principles with Watson's theory of transpersonal caring within acute healthcare complexities to re-conceptualize the individual nurse-patient relationship.
Watson's Theory of Transpersonal Caring
Watson's theory forms the groundwork for nursing's most profound philosophical principles. The theory highlights the central role of humanistic care and transpersonal connections between nurse and patient as an essential blend of science and art [7]. The three foundational concepts are 'carative' processes (Figure 1), transpersonal caring relationships, and the caring occasion/moment that guide nurses in delivering humanistic care [7-9]. Watson proposed that ten carative processes form the core competencies of biopsychosocial care in nursing [7,10].
Carative processes differentiate medicine's curative nature to the altruistic and human dimensions of nursing work. This approach is purposeful, deliberate, and practiced mindfully. It recognizes that the caring moment is fostered within the transpersonal caring relationship and can occur with any patient interaction, no matter how short the interaction. With a caring consciousness, the nurse connects with a patient spiritually, allowing for a rich and dynamic connection beyond the physical interaction [8].
Therapeutic Relationship Barriers in Acute Care Nursing Teams
Conflicting caring culture
Technical nursing skills are measurable, yet subtle, quiet moments of transpersonal caring are not. These caring moments quickly fade into the busy nursing unit's background, often going unrecognized and undervalued [2,5]. In acute care, nurses are responsible for managing, prioritizing, and coordinating a large caseload of patients, significantly impeding their ability to maintain therapeutic relationships due to a constant cognitive shift from competing priorities among patients [11]. Factors such as systemic constraints, inadequate resources, and suboptimal working conditions narrow the focus of care to measurable clinical tasks as the only priority that cannot be left incomplete, such as medication administration and clinical procedures [12]. A conflicting caring culture has prioritized meeting patients' lower-order needs, thus practicing in a task-focused manner due to personal, team, and organizational influences that reduce nursing care to quantifiable care tasks. It has assimilated nurses with the best intentions to practice in this way to survive [9,13].
Task orientation
Consequently, nurses concede to strategies that prioritize basic, measurable patient care needs. Cognitive stacking is necessary when managing multiple complex patients. It is an "accumulative measure for quantifying tasks and priorities a nurse needs to perform at any given time for a group of patients during an assigned shift" [11]. Care rationing is a maladaptive response where therapeutic communication, teaching, coordinating care, and proper patient surveillance are not optimized and may receive lesser priority due to the perceived pressure to promptly complete tangible tasks [14]. An innovator in humanistic psychology, Maslow described a hierarchy of needs beginning with physical, safety needs that progress to self- actualization [15]. In alignment with these principles, Watson's theory of caring proposes that "meeting only lower-order needs may not help a person toward optimal health. Attention must be given to higher-order needs" [16].
Ontological principles of caring science have always existed in the healing professions, but we have become lost along the way as educational, professional, and organizational practices have desensitized our shared sense of humanity [9]. Diminished holistic care raises the issue of moral distress for nurses who are conflicted between completing complex daily tasks and the desire to engage more authentically with their patients [1,17].
Care delivery
Patients have described the essential principles of care delivery as "professional knowledge, human connection, joint decision making between the patient and the nurse, individualized treatment plans, caring attention, promptness to addressing individualized needs, continuity of care, and having nurses coordinate the care with other disciplines." [18]. Developing therapeutic relationships is more easily achieved within a primary-care delivery model as each nurse has control over their patient's care [18]. This model embraces the individualistic nature of relationships and professional presence in nursing practice [4]. The challenge becomes finding effective ways to translate these patient-centered moments that are achievable in a primary care model into the team-based model required in acute care settings. The individualistic nature of therapeutic relationships is a significant challenge to maintain within a team comprised of nurses with differing values and motivation to meet a patient's needs beyond physical, measurable care acts [19].
CTNR-A model
While individuals' committed efforts cannot be understated, a larger shift is required at the team level to nurture a healthy caring culture. A single nurse cannot offer the highest quality of care without collaboration amongst team members and an integrated care process to manage continuity of care and therapeutic relationships [4,20,21].
The authors offer the CTNR-A model (Figure 1) as an introductory framework grounded in fouressential components (team emotional intelligence, team functioning, caritas processes, & caring culture). The purpose of this model is to address real and/or potential barriers in cultivating therapeutic relationships within acute care nursing and also to guide the nursing teams to redefine therapeutic relationships. The model shifts away from the traditional, individualistic nature of therapeutic nurse relationships to the realities of team-based care delivery. Although further systematic research is needed to analyze the relationship between the four concepts, the authors believe that this model will provide guidance for clinical practice. The value of each concept is supported by rich data as they relate to relational nursing practice. However, this model offers a unique perspective on how to integrate all four concepts to create a more robust framework to support caritas processes within team nursing in acute care. The four main concepts in this model exist together to shift the individualistic nature of therapeutic relationships to a shared, collaborative relationship amongst the entire nursing team and patients.
Caritas processes
The caritas processes offered within Watson's theory have long been regarded as essential processes for providing high-quality patient care and developing therapeutic nursing relationships [7-10,15]. The caritas processes have practical applications in acute care. Cara [10] demonstrated this in her work A Pragmatic View of Jean Watson's Caring Theory, the practical application of clinical caritas processes (CCP) within a clinical story. Cara asserted that "aiming to preserve our human caring heritage, this paper offered some suggestions and ideas in order to help nurses grasp and utilize Watson's caring theory in their work environment." [10]. The authors acknowledge the merit of Cara's work which provides a practical context. However, the approach is consistent with the traditional individualistic approach to therapeutic nursing relationships (Babiker et al., 2014) [4]. Consider the caritas processes' practical application below.
"From his faint smile I can sense that he is depressed. Probably since part of his leg has to be amputated some more. However, I cannot make this assumption and will have to discuss his perceptions and feelings pertaining to his lived experience (CCP#3, CCP#5, CCP#10). While I help him settle in his room, I arrange his environment so that he can feel at ease (CCP#8). Right away, I use the time we have together to ask about himself, his feelings, and his priorities for his care plan and hospitalization (CCP#5, CCP#10). He explains that he wants to be home for Christmas because his son and grandson are coming to visit. Consequently, we will have to plan everything according to his priority. [Although caring takes "too much time" according to some people, I have found, through experience that focusingon the patients' priorities and meaning will often help them participate more actively in their healing process." [10].
Caritas process, along with the concepts; team functioning, caring culture, and emotional intelligence, must exist congruently within the realities of acute care where multiple nurses are involved in providing care in order for it to be consistent.
Team functioning
Responsible time management, delegation, and prioritization are required to care for multiple patients. Quality care in the current healthcare environment relies on the entire team's relationship with the patient, as one nurse cannot safely provide comprehensive care for many clients simultaneously [4,21-23]. Ghorob and Bodenheimer [20] advocated for a 'teamlet' model of care delivery, which allows team members to cultivate smaller, defined teams with more clearly-defined workflows, increased visibility to patients, and increased accountability to complete the care. The 'teamlet' model includes daily huddles to clarify and prioritize care needs and real-time communication during interactions, which can happen more readily in smaller working groups [20]. Team orientation, communication, and better delegation and assignment skills are also integral and allow team members to reduce work overload and share care activities [21].
Caring culture
The theoretical principles of a caring culture in nursing teams are the 6Cs; "care, compassion, competence, communication, courage, and commitment." [4]. Shared goals, frequent interactions, and clear, concise communication remain central to a healthy team's functioning as a collective unit with specialized knowledge [24]. A qualitative descriptive study uncovered five core practical processes for enhancing a caring culture and collaboration, collectively described as (1) building caring relationships; (2) developing an ownership mentality; (3) providing constructive feedback; (4) applying the strengths-based practice, and (6) acting as the first and last lines of defense [24]. These processes are part of the Interprofessional Caring Model and are projected to have profound clinical implications when used as a framework to build a valued caring culture and collaboration amongst healthcare teams [24]. An emphasis on reorienting and building caring cultures exists within contemporary nursing literature [6,25-27]. The core value of this endeavor within team-settings is to provide consistent, and quality nursing care shared amongst all team-members that a patient comes in contact with [4,24].
Team emotional intelligence (EI)
EI has long been regarded as a critical concept to cultivate quality care in nursing [19]. Five concepts of EI include awareness of emotions, regulating emotions, self-motivation, empathy, and social skill [28]. EI from a team-perspective has received growing attention as a critical component of high-quality care delivery and cohesiveness [29-31]. Quoidbach and Hansenne [32] applied EI within a team setting to evaluate team functioning and cohesiveness. The results demonstrated from a team-level that EI encompasses four key variables (1) overall EI, (2) optimism/mood regulation, (3) appraisal of emotion, and (5) utilization of emotion with varying levels of implication [32]. Optimism and mood regulation were classified as the most crucial EI concept within a team as even one member with high EI can influence the whole team's emotional climate, encouraging motivation to practice in a humanist and relational manner [32]. A nurse with EI will intentionally apply empathetic methods of interaction with others in their practice and are less likely to make rushed decisions or compromise their fundamental nursing values. Nurses are expected to possess an awareness of their own EI to be self-aware and resist potential assimilation within a team that struggles with conflicting values. Quoidbach and Hansenne argued that these results offer a promising connection of team EI and high-quality care delivery and emphasize that further research is required to better understand practical applications of EI as part of a team's functioning and culture [32].
Discussion
The CTNR-A is an introductory model that can be applied to acute care nursing teams that function as 'teamlets' and is intended to redefine therapeutic nursing relationships amongst multiple nurses and patients. Each of the four concepts presented within the CTNR-A model all have merit in promoting therapeutic nurse-patient relationships. Nevertheless, the authors propose that integrating all four of these concepts in practice can strengthen the shared therapeutic relationships amongst the entire team. Moving forward, nursing teams are encouraged to critically appraise their effectiveness in applying each of the four concepts within the CTNR-A model. By doing this, it gives rise to the opportunity to improve seamless and consistent relational care to care delivery. There is tremendous opportunity for the team to reflect on their strengths and create opportunities for change. This reflexive practice may reveal that one or more concepts may need to be strengthened and therefore opens the door for further dialogue on how to engage in therapeutic relationships more fully from the lens of the team.
For example, an RN, LPN, and unregulated care provider work as a 'teamlet' when providing care. As a team leader, the RN ensures proper team functioning by prioritizing, delegating, and assigning care activities to the most appropriate provider at the right time to optimize the scope of practice, team-roles, and efficiency. Team functioning cannot exist in a silo, and shared goals are essential to orient the team beyond task-based care and are closely connected to a caring culture. The team's EI will allow for reflective practice and promote an environment where emotions are acknowledged and appraised to support a healthy and safe work environment. Together, a caring culture will naturally provide comprehensive and relational care to patients using the caritas processes during each caring moment. While each provider cannot be with each patient simultaneously in team-based care, blending the four CTNR-A concepts can fortify collaborative therapeutic relationships for each patient and the team as a whole.
Further research is required to fully explore how the CTNR-A model support team-based relational care. This will allow for a deeper understanding of each concept's correlation to collaborative therapeutic nursing relationships and provide concrete applications to implement in practice.
Summary
There are exciting opportunities to strengthen a team-based nursing approach in acute care environments by infusing the principles of Watson's theory of caring. The nature of team-based acute care nursing can overshadow the meaningful therapeutic nurse-patient relationship that is influenced by a conflicting caring culture and task-orientation. Therefore, the CTNR-A model provides opportunity to rejuvenate and re-align nursing to a culture of 'caring' in these most difficult times. Further systematic research on the CTNR-A is invited to expand understanding of the relationships between the model's concepts and application to shift the traditional autonomous relationship of nurse-patient to one shared between team and patient.
References
- Canadian Nurses Association (2021) Nursing statistics.
- Duffy JR, Culp S, Padrutt T (2018) Description and factors associated with missed nursing care in an acute care community hospital. J Nurs Adm 48: 361-367.
- Johnson JA (2015) Tasks and technology versus compassion and caring in nursing: Are they mutually exclusive? J Nurses Prof Dev 31: 338-340.
- Babiker A, El Husseini M, Al Nemri A, et al. (2014) Health care professional development: Working as a team to improve patient care. Sudan J Paediatr 14: 9-16.
- Pashaeypoor S, Baumann SL, Sadat Hoseini A, et al. (2019) Identifying and overcoming barriers for implementing Watson's human caring science. Nurs Sci Q 32: 239-244.
- Adams LY (2016) The conundrum of caring in nursing. Int J Caring Sci 9: 1-8.
- Alligood MR (2017) Nursing theorists and their work-ebook. Elsevier Health Sciences.
- George JB (2011) Nursing theories: The base for professional nursing practice. (6th Edn). Boston : Pearson, USA.
- Smith MC, Turkel MC, Wolf ZR (2012) Caring in nursing classics: An essential resource. Springer Publishing Company, USA.
- Cara C (2003) A pragmatic view of Jean Watson's caring theory. IJHC 7: 51-62.
- Potter P, Wolf L, Boxerman S, et al. (2005) Understanding the cognitive work of nursing in the acute care environment. J Nurs Adm 35: 327-335.
- Patterson ES, Ebright PR, Saleem JJ (2011) Investigating stacking: How do registered nurses prioritize their activities in real-time?. Int J Ind Ergonom 41: 389-393.
- Lusignani M, Giannì ML, Re LG, et al. (2017) Moral distress among nurses in medical, surgical, and intensive-care units. J Nurs Manag 25: 477-485.
- Zhu X, Zheng J, Liu K, et al. (2019) Rationing of nursing care and its relationship with nurse staffing and patient outcomes: The mediation effect tested by structural equation modeling. Int J Environ Res Public Health 16: 1672.
- Clark CS (2016) Watson's human caring theory: Pertinent transpersonal and humanities concepts for educators. Humanities 5: 21.
- Watson J (1985) Nursing: Human science and human care: A theory of nursing. Jones & Bartlett Publishers.
- Sims S, Leamy M, Levenson R, et al. (2020) The delivery of compassionate nursing care in a tick-box culture: Qualitative perspectives from a realist evaluation of intentional rounding. Int J Nurs Stud 107: 103580.
- Jost SG, Bonnell M, Chacko SJ, et al. (2010) Integrated primary nursing: A care delivery model for the 21st-century knowledge worker. Nurs Adm Q 34: 208-216.
- White DE, Grason S (2019) Creating a culture of care in nursing education. Int J Nurs Health Care Res 10: 1122.
- Ghorob A, Bodenheimer T (2015) Building teams in primary care: A practical guide. Fam Syst Health 33: 182-192.
- Goh PQL, Ser TF, Cooper S, et al. (2020) Nursing teamwork in general ward settings: A mixed-methods exploratory study among enrolled and registered nurses. J Clin Nurs 29: 3802-3811.
- Campbell AR, Layne D, Scott E, et al. (2020) Interventions to promote teamwork, delegation, and communication among registered nurses and nursing assistants: An integrative review. J Nurs Manag 28: 1465-1472.
- Yoder-Wise PS, Waddell J, Walton N (2019) Leading and managing in Canadian nursing. Elsevier Health Sciences.
- Wei H, Watson J (2019) Healthcare interprofessional team members' perspectives on human caring: A directed content analysis study. Int J Nurs Sci 6: 17-23.
- Bennett B (2017) A culture of caring: How nurses promote emotional wellbeing and aid recovery following a stroke. Br J Neurosci Nurs 13: S8-S17.
- Cook LB, Peden A (2017) Finding a focus for nursing: The caring concept. Adv Nurs Sci 40: 12-23.
- Tang FWK, Ling GCC, Lai ASF, et al. (2019) Four Es of caring in contemporary nursing: Exploring novice to experienced nurses. Nurs Health Sci 21: 85-92.
- Kaya H, Senyuva E, Bodur G (2017) Developing critical thinking disposition and emotional intelligence of nursing students: A longitudinal research. Nurse Educ Today 48: 72-77.
- Barrick MR, Stewart GL, Neubert MJ, et al. (1998) Relating member ability and personality to work-team processes and team effectiveness. J Appl Psychol 83: 377-391.
- Prati L, Douglas C, Ferris GR, et al. (2003) Emotional intelligence, leadership effectiveness, and team outcomes. Int J Organ Anal 11: 21-40.
- Rapisarda BA (2002) The impact of emotional intelligence on work team cohesiveness and performance. Int J Organ Anal 10: 363-379.
- Quoidbach J, Hansenne M (2009) The impact of trait emotional intelligence on nursing team performance and cohesiveness. J Prof Nurs 25: 23-29.
Corresponding Author
Cameron Albright, BScN, RN, Nova Scotia Health Authority, Nova Scotia, Canada, E-mail: Cameron.Albright@nshealth.ca
Copyright
© 2021 Albright C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.