Impact of Caregiver Support on Patient Self-Care Outcomes with Heart Failure: A Systematic Review
Abstract
Aim
The purpose of this systematic review was to assess the impact on patient outcomes of caregivers' contribution to heart failure (HF) self-care. The reason for choosing this condition is because of the importance of involving the caregiver support in self-care patients with HF.
Methods
The review was guided by The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines; the search was conducted for years 2014 to 2019 utilizing three databases: CINHAL, PubMed, and Psych INFO.
Results
The systematic review revealed that caregivers contribute to self-care and patient confidence. Five studies reported a level of confidence for health behavior (exercise, medication adherence, and diet) as a significant predictor for caregiver contributions to patient self-care. One study found that patients who were cared for by their spouses experienced a risk for a low level of confidence compared to adults-children caregivers. Four studies reported the relationship between caregiver contribution to patient self-care and health related quality of life. Two studies found that caregiver contributions to patient self-care caused a significant reduction in readmission, hospitalization, and mortality of patients.
Clinical implication
The findings from this review have encouraged providers to conduct interventions that focus on quality of patient-caregiver relationships (e.g., mutuality).
Keywords
Caregivers, Hear Failure, Self-Care
Description and Rationale for Caregiver Population
An informal caregiver is someone who provides unpaid care to a family member or friend who is unable to coordinate self-care without support [1]. This support may include day-to-day activities such as mobility assistance, medical tasks such as checking daily medications, helping with injections, scheduling appointments, and discussing the patient's medical plan. This support may also be emotional, social or psychological [2]. Approximately 43.5 million informal caregivers provide unpaid care to family or friends with physical or mental disabilities [3,4]. The Family Caregiver Alliance3estimated that care provided by informal caregivers to family or friends was approximately $470 billion in 2013. Government policymakers saw the importance and value of caregivers under the legislation of the Family Caregiver Alliance in 1977. In 2018, the National Guidelines for Health and Care Excellence [5] (NICE 106) recommended that caregivers be included in the decision-making process during the planning of medical care. A meta-analysis of 569 medication adherence studies found that medication adherence rates were approximately 25% among patients with chronic illness. According to a mixed-method study by Sussman, et al. [6], which looked at family and friends support for chronic disease management, 35% of patients reported that family support is the most important aspect of chronic disease management. Although several interventional studies have been conducted to promote effective self-care HF, little research has been done to explore the extent to which informal family caregivers support health care activities, primarily because family caregivers are not identified in the family care experience [7].
Aims
The purpose of this systematic review was to assess the impact of informal caregiver contributions to HF self-care on patient outcomes. The reason behind choosing this condition is because HF is a chronic condition that significantly impacts the quality of life of patients living with the disease. Approximately one in five adults in the United States have HF; and approximately 50% of people who develop HF die during the first five years of diagnosis [8]. Heart failure presents a major challenge for health policy makers in primary and secondary intervention care [9] and has a significant impact on the physical and mental health of caregivers who provide personal care and support for self-care planning [10].
Self-Care and Caregiver
Self-care is an approach that enables individuals to solve problems as they arise, practice new health behaviors, and gain emotional stability [11]. Self-care, in the literature on heart failure, is defined as daily activities that address key behaviors such as medication, diet, and exercise [12].
Self-care is initiated by HF patients with varied levels of support from informal caregivers (CGs) such as family members or friends. Wingham, et al. [9] noted that caregivers need to have a clear picture of the patients they care for; caregivers need to know how to participate in care giving activities. The care activities should include monitoring and planning for daily life activities, providing complex medications that may require modification, and adherence to dietary restriction.
Furthermore, caregivers should be involved in discussions about care to develop their abilities to support self-maintenance and self-management experiences. The National Institute of Health and Care Excellence Clinical Guidelines 108 for HF [5] recommended that caregivers be involved in discussion about self-care management plan. Most caregivers, however, have little knowledge about how to expand their competence to support self-care [9]. Researchers agree that it is critical to engage caregivers in self-care activities to achieve positive health outcomes for HF patients [6,7,9-11].
Methods
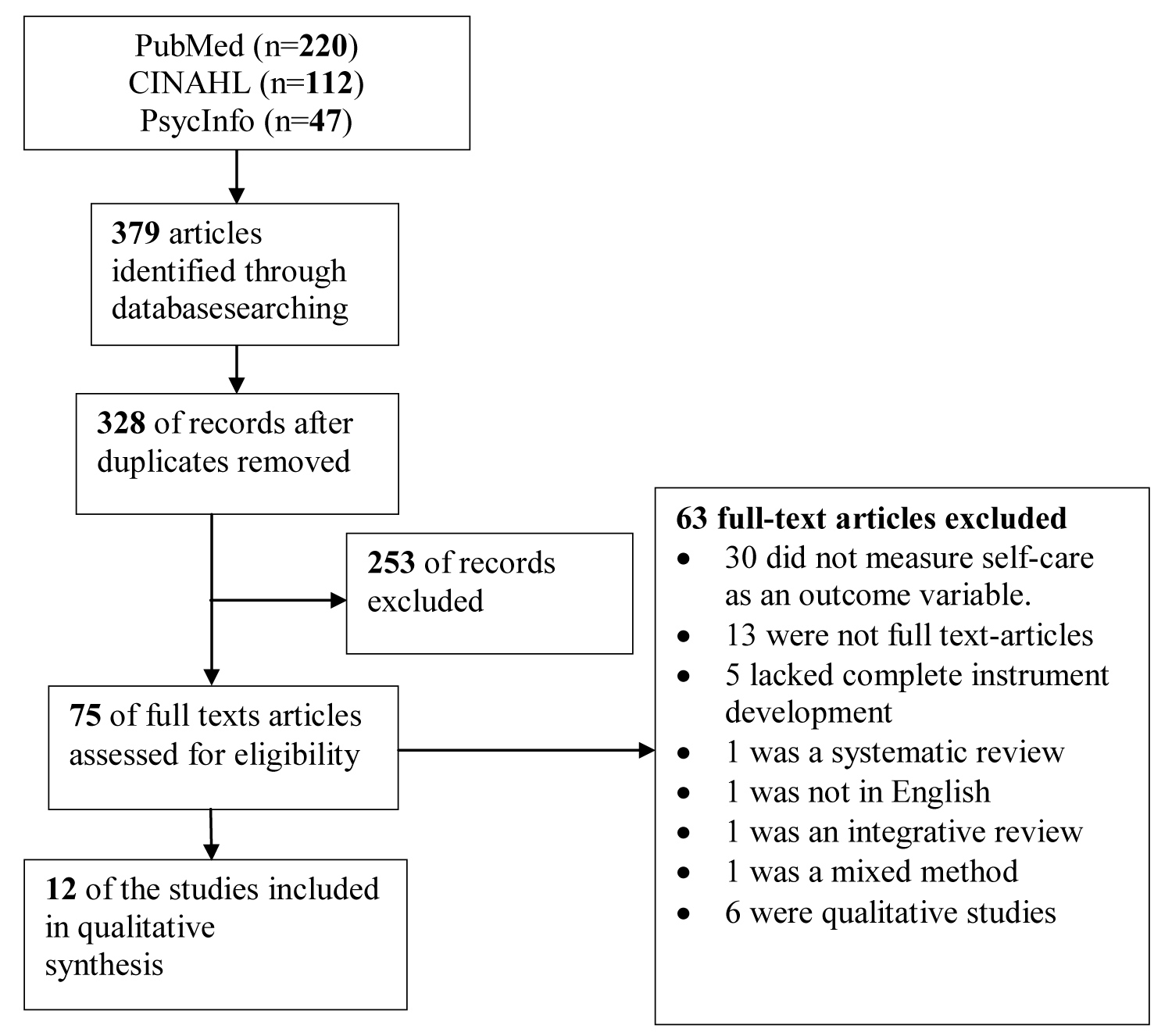
This Systematic Review way was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [13]. PRISMA ensures the transparent and thorough reporting of systematic review [14]. The search was conducted for years 2014 to 2019 utilizing three databases: CINHAL, PubMed, and Psych INFO. This five-year period was chosen to synthesize the current findings of literature with evidence-based practice. To extract the appropriate articles, the following key words were used in PubMed: "Self-management OR self-care" AND "family caregivers OR informal caregivers OR relatives OR family" AND "heart failure." The same search strategy was followed with the Cumulative Index to Nursing and Allied Health Literature (CINAHL) and Psych Info. The search was limited to English, peer-reviewed, year of publication, and full text research articles. There were no limitations on geographical location or type of patient outcomes because this systematic review aimed to identify all possible self-care outcomes and to involve all possible studies for the purpose of this review.
Eligibility Criteria
Studies were included in the systematic review if they (a) Used a quantitative methodology; (b) Included participants with HF who were > 18 years old; (c) included an informal caregiver; (d) explicitly measured patient outcomes. Studies were excluded in the systematic review if they (a) used a qualitative methodology; the traditional way for systematic review is only including empirical study with statistical outcomes [15]; (b) Included formal caregivers.
Review Process
All screened articles were organized and retrieved using a Microsoft word document and RefWorks reference management software. Articles titles and abstracts were assessed for eligibility after removing duplicates. Then, the full-text articles were retrieved and extracted into a table. The data were extracted based on the following methods: Authors' name, year of publication, country name, design and sample size, purpose, key variables and instruments, and findings. The validity of the studies was assessed using the Systematic Review of Observational Studies (QATSO) checklist Quality Evaluation Tool [16], which was slightly updated to suit the analysis (Table 1). The QATSO consists of items for assessing external validity, bias, and confounding, and the validity/reliability of outcomes measurement. The total quality score is the total score divided by 100 items multiplied by the total number. Studies were referred to as bad (0-33%), satisfactory (34-66%), and good (67-100%) [16].
Results
Selection of the studies
The electronic search extracted 379 articles (Figure 1); 51 duplicate articles were removed. The remaining 328 articles and abstracts were screened for eligibility and 253 articles were excluded because of inclusion and exclusion criteria. The remaining full-text articles (75) were further screened for eligibility. Of these, 63 articles were excluded because these articles: (a) Did not measure self-care as outcomes (30); (b) did not have full text articles (13); (c) lacked complete instrument development (concept identification, item construction, validity and reliability testing) (5); (d) did not measure patient outcomes (5; (e) was not in English language (1); (f) were qualitative studies (6); (g) was systematic review (1); (h) was integrative review (1); (i) used a mixed method methodology (1). The remaining 12 studies were involved in the systematic review.
Study characteristics
The 12 studies reviewed for this paper were published between 2014 and 2019 (Table 2). The study samples' sample size ranged from 83 to 1192 participants. The samples represented four countries: Italy (n = 5), Lebanon (n = 1), Thailand (1), and the United States (n = 5). Studies from the United States involved White, African American, and Hispanic or Latino. The mean age for participants included in the review ranged, for patients, from 52 to 76 years old and for caregivers from 33 to 64 years old. Both male and female caregivers including spouses/partners, children, and sisters were included in the review, with a dominant percentage of females ranging from 50% to 90%. Six studies (60%) had a cross-sectional design. Of these 12 studies, six studies had an RCT (randomized controlled trial) design [17-22]. The remaining studies used a descriptive design.
Studies categorization
Relationship between caregiver contribution and patient self-management outcomes
The systematic review revealed that caregivers contribute to self-care and patient confidence. Five studies reported a level of confidence for health behavior (exercise, medication adherence, and diet) as a significant predictor for caregiver contributions to patient self-care [17,18,21-23]. One study found that patients who were cared for by their spouses experienced a risk for a low level of confidence compared to adults-children caregivers [24]. This was because the spouse caregivers in this study had poor physical and mental health compared to adult-children caregivers. However, in the same study also found that the level of confidence among patients mediated the high level of medication adherence and diet [24].
Caregiver and patient health related quality of life
Four studies reported the relationship between caregiver contribution to patient self-care and health related quality of life [17,20,25,26]. For example, two studies reported the inverse relationship between caregiver contributions to self-care and patient physical and mental health related quality of life (p = 0.77, 0.25) respectively [17,26]. However, two studies found the health quality of life related to emotional symptoms was a significant determinant of better self-care from caregivers to their recipients [25,26].
Caregiver and patient clinical outcomes
Three studies reported the impact of involvement of caregivers on patient self-care caused a significant reduction in readmission, hospitalization, and mortality of patients (p = 0.02) [17,26,27]. Also, the study by Deek, et al. [17] in their study found patients who involved their family centered- self-care intervention had lower readmission rates and fewer major vascular events (heart attack, cerebral vascular) than control group patients (p = 0.01).
Caregiver patient motivation for medication adherence and diet
Two studies reported the relationship between caregiver contributions to patient self-care and patient motivation for medication adherence and diet [18,19]. For example, the study by Stamp, et al. [18] showed that the motivation for medication and diet was significant among patients. Dunbar, et al. [19] found an inverse relationship between poor family function and high level of Na in diet among patients with heart failure.
Patient-caregiver Dyads and self-care Outcomes. Five studies demonstrated the influence of mutuality on self-care outcomes for HF patients [21,23-25,28]. Specifically, among the six studies, Vellone, et al. [21] investigated the three dimensions of self-care including self-maintenance, management and confidence.
Discussion
The purpose of this systematic review was to examine the impact of caregivers' contributions to self-care on patient outcomes. The findings revealed a link between the contribution of caregivers to patient self-care and patient outcomes. These findings are consistent with those of other reviews conducted among patients with other chronic diseases [28-31].
The findings of this review demonstrate the evolution of self-care science in the contribution of caregivers to HF self-care. These findings indicate that patients' physical and psychological health determines patients' self-care outcomes [27]. These findings from our review are consistent with findings from other reviews of family care and their impact on the physical and mental health of the patient [32]. As far as the caregiver is concerned, the strain, the quality of life, and social support are linked to the caregiver in the context of self-care [25]. Health care providers should take caregivers' situation into account when they are involved in patient self-care. The review also highlighted the importance of a dyadic approach to interventions such as educational supplements and archetypes of dyadic caregivers. These findings indicate that the dyadic approach plays a significant role in patient self-care outcomes [26, 27].
Overall, although the studies involved in this systematic review showed a significant impact on patient self-care outcomes, there was a discrepancy between the results. There are three causes that explain the discrepancy in findings. First, there are differences in the cultural background of the populations studied. Second, the sample size ranges from 83 to 1192 participants. Third, age ranging from 52 to 76 years of age. As a result, this discrepancy in findings suggested that caregivers' experiences may differ across age groups, populations, patient comorbidities, and cultures, indicating the need to understand the perceptions of caregivers about their contribution to HF self-care.
Limitations
These findings demonstrate the limitations of the studies reviewed. First, the majority of the studies used secondary data analysis with cross-sectional design. Most of the studies in this review lack probability sampling, which confines causality and generalizability of the findings to populations with heart failure. Furthermore, a plurality of the studies used self-report measures of caregiver contributions to patient self-care, which could present recall bias and a misestimate of caregiver contributions. Also, these studies used dissimilar definition criteria for caregiver contributions to patient self-care. As a result, more studies are needed to measure caregiver contributions to patient self-care objectively and consistently.
Moreover, this review is susceptible to assorted limitations, which are deep-rooted in the systematic review. This review is subject to selection and reporting bias because this systematic review was confined to English full-text studies, year of publication, and only quantitative studies retrieved from three electronic databases. As a result, non-English reviews, books, theses or dissertations, and studies obtained through a manual search or references list were not included.
Implications for Clinical Practice and Future Research
The findings from this review have various implications for the clinical and research arena. Clinically, we need to educate healthcare providers about the importance of involvement of caregivers in patient self-care activities and all educational sessions. Also, it is imperative to encourage providers and practitioners to conduct interventions that focus on quality of patient-caregiver relationships (e.g., mutuality) to improve patient self-care and caregiver contributions to self-care. Most of the studies included in this analysis used secondary data analysis with cross-sectional designs and various measures of self-care. Therefore, future studies are needed to measure caregiver contributions to patient self-care using objective measures; longer follow-up periods are also essential to assess long-term self-care activities on outcomes, such as readmission, mortality, and quality of life. More longitudinal studies are needed to examine the impact of caregiver contributions to patient self-care on outcomes.
Conclusion
This systematic review sought to incorporate findings of quantitative studies to examine the impact of caregiver contributions to self-care on HF patient outcomes. Findings showed that caregiver strains, gender, and caregiver quality of life were related to greater caregiver contributions to patient self-care. Also, findings showed mixed results concerning the relationship between caregiver roles regarding symptoms and the treatment evaluation process. Furthermore, the findings highlighted that self-confidence mediates and moderates the relationship between patient self-care and outcomes. The findings of this systematic review accentuate the significance of the caregiver role, specifically the dyadic approach and mutuality. Given these findings, it is important to merge interventions focusing on a dyadic approach.
References
- (2015) Carers Trust.
- Wolff JL, Spillman BC, Freedman VA, et al. (2016) A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA internal medicine 176: 372-379.
- National policy statement. (2019) Family Caregiver Alliance.
- Freedman VA, Spillman BC (2014) Disability and care needs among older Americans. The Milbank Quarterly 92: 509-541.
- (2018) Chronic heart failure in adults: Diagnosis and management. The National Institute for Health and Care Excellence Guidelines.
- Sussman T, Yaffe M, Mccusker J, et al. (2014) A mixed methods exploration of family members'/friends' roles in a self-care intervention for depressive symptoms. Chronic illness 10: 93-106.
- Braveman P, Gottlieb L (2014) The social determinants of health: It's time to consider the causes of the causes. Public health reports 129 (Suppl 2): 19-31.
- Heart failure fact sheet (2019) Centers for Disease Control and Prevention.
- Wingham J, Frost J, Britten N, et al. (2015) Needs of caregivers in heart failure management: A qualitative study. Chronic illness 11: 304-319.
- Clark A M, Sapling M, Harkness K, et al. (2014) Determinants of effective heart failure self-care: A systematic review of patients' and caregivers' perceptions. Heart 100: 716-721.
- Riegel B, Lee CS, Dickson VV (2011) Self-care in patients with chronic heart failure. Nature Reviews Cardiology 8: 644-654.
- McGreal MH, Hogan MJ, Walsh-Irwin C, et al. (2014) Heart failure self-care interventions to reduce clinical events and symptom burden. Research Reports in Clinical Cardiology 5: 243-257.
- Moher D, Liberati A, Tetzlaff J, et al. (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of internal medicine 151: 264-269.
- Liberati A, Altman DG, Tetzlaff J, et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Annals of Internal Medicine 151: 65.
- Ankem K (2008) Evaluation of method in systematic reviews and meta-analyses published in LIS. Library and Information Research 32: 91-104.
- Wong WC, Cheung CS, Hart GJ (2008) Development of a quality assessment tool for systematic reviews of observational studies (QATSO) of HIV prevalence in men having sex with men and associated risk behaviours. Emerg Themes Epidemiol 5: 23.
- Deek H, Chang S, Newton PJ, et al. (2017) An evaluation of involving family caregivers in the self-care of heart failure patients on hospital readmission: Randomised controlled trial. Int J Nurs Stud 75: 101-111.
- Stamp KD, Dunbar SB, Clark PC, et al. (2016) Family partner intervention influences self-care confidence and treatment self-regulation in patients with heart failure. European Journal of Cardiovascular Nursing 15: 317-327.
- Dunbar SB, Clark PC, Stamp KD, et al. (2016) Family partnership and education interventions to reduce dietary sodium by patients with heart failure differ by family functioning. Heart Lung 45: 311-318.
- Srisuk N, Cameron J, Ski CF, et al. (2017) Randomized controlled trial of family-based education for patients with heart failure and their carers. Journal of Advanced Nursing 73: 857-870.
- Vellone E, Chung ML, Alvaro R, et al. (2018) The influence of mutuality on self-care in heart failure patients and caregivers: A dyadic analysis. J Fam Nurs 24: 563-584.
- Wu JR, Reilly CM, Holland J, et al. (2017) Relationship of health literacy of heart failure patients and their family members on heart failure knowledge and self-care. Journal of Family Nursing 23: 116-137.
- Lee CS, Vellone E, Lyons KS, et al. (2015) Patterns and predictors of patient and caregiver engagement in heart failure care: A multi-level dyadic study. Int J Nurs Stud 52: 588-597.
- Hooker SA, Schmiege SJ, Trivedi RB, et al. (2018) Mutuality and heart failure self-care in patients and their informal caregivers. Eur J Cardiovasc Nurs 17: 102-113.
- Lyons KS, Vellone E, Lee CS, Cocchieri et al. (2015) A dyadic approach to managing heart failure with confidence. J Cardiovasc Nurs 30: S64-71.
- Bidwell JT, Vellone E, Lyons KS, et al. (2015) Determinants of heart failure self-care maintenance and management in patients and caregivers: A dyadic analysis. Res Nurs Health 38: 392-402.
- Bidwell JT, Higgins MK, Reilly CM, et al. (2018) Shared heart failure knowledge and self-care outcomes in patient-caregiver dyads. Heart Lung 47: 32-39.
- Bidwell JT, Vellone E, Lyons KS, et al. (2017) Caregiver determinants of patient clinical event risk in heart failure. Eur J Cardiovasc Nurs 16: 707-714.
- Locher JL, Robinson CO, Bailey FA, et al. (2009) The contribution of social factors to under eating in older adults with cancer. J Support Oncol 7: 168-173.
- Montague T, Gogovor A, Ahmed S, et al. (2015) Contributions and challenges of non-professional patient care: A key component of contemporary canadian healthcare. Healthc Q 18: 18-22.
- Santos M, Sousa C, Pereira M, et al. (2019) Quality of life in patients with multiple sclerosis: A study with patients and caregivers. Disabil Health J 12: 628-634.
- Willink A, Davis K, Mulcahy J, et al. (2017) Use of paid and unpaid personal help by medicare beneficiaries needing long-term services and supports. Issue brief 1-9.
Corresponding Author
Nader R. Alnomasy, Frances Payne Bolton School of Nursing, Case Western Reserve University, 1218 Barker Blvd, Apt. A. Kent, 44240, Cleveland, Ohio, USA, Tel: 607-222-1036.
Copyright
© 2020 Alnomasy NR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.