Unexpected Intracranial Metallic Foreign Body in Child: Case Reports in Non-War Area and Literature Review
Abstract
Introduction: The occurrence of an intracranial metallic foreign body in children is often due to home accidents, child abuse or wars. Our aim was to highlight more this phenomenon quite rare, becoming from nowadays of public health and to compare adapted treatments to originator ones of the Literature. Two children with both brain injury due to metal after domestic accident, operated in 2018 and closely followed-up during 3 years were gathered. Their cases are reported, and their features discussed according to Literature.
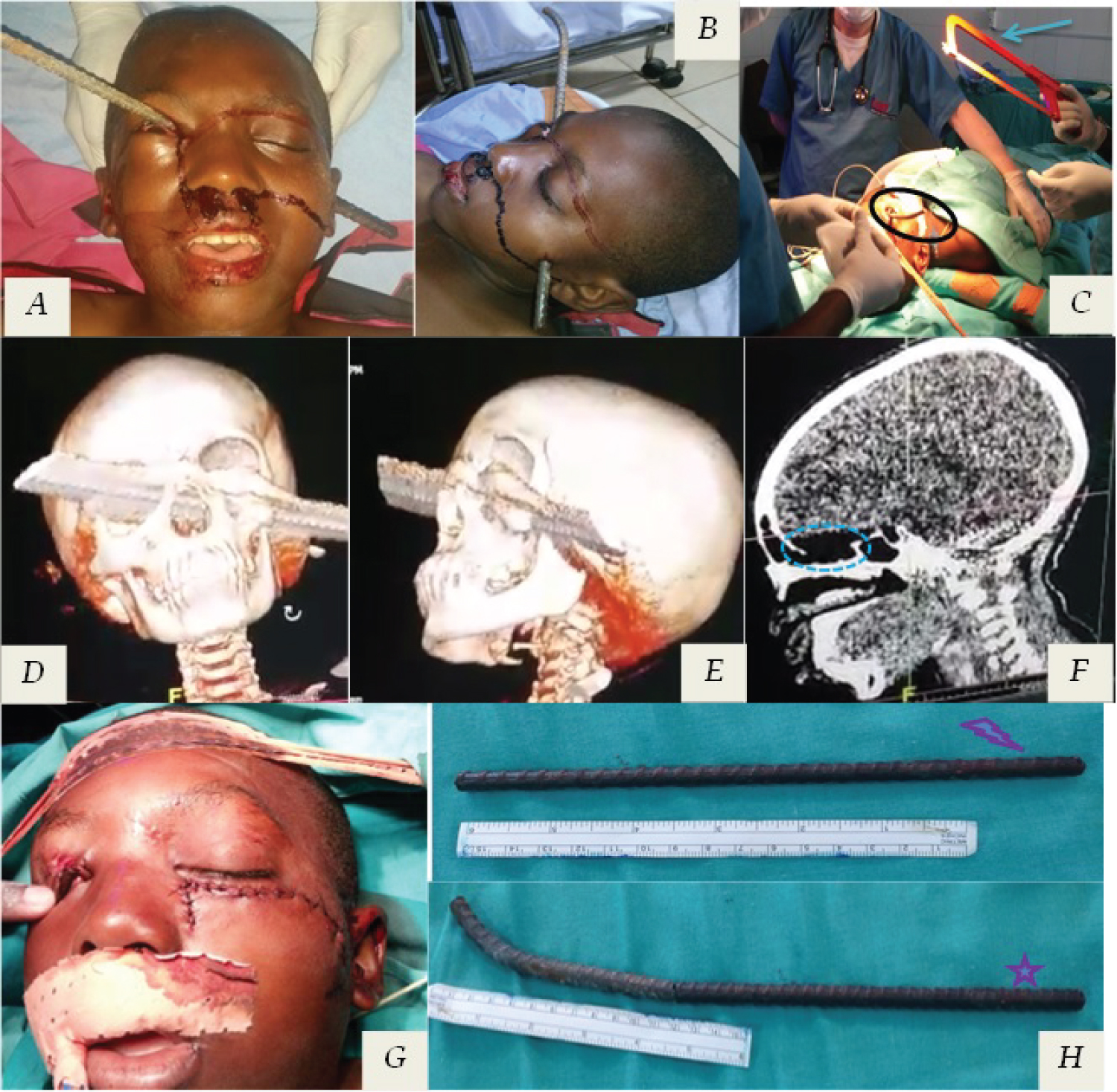
Cases presentation: Children were 13-month-old and 12-year-old all operated less than 24 hours after the trauma. It was a masonry nail long of 5 centimetres (cm) for the infant and ø8 (millimetres = mm) iron rod long of 48 cm for the teenager. The mechanism was the fall at home from his height or from a mangoes-tree. The entry zone was the left-occipital in the first case and the right inner canthus in the second. The metallic foreign body was surgically removed in both cases and without complications. The follow-up during 3 and half years was also neurologically uneventful.
Discussion/conclusion: Metallic intracranial foreign bodies are encountered mostly in wartime or high violence area, rarely in domestic games. None Angio-CT-scan was performed. Surgical removal must be as earlier when possible but should not omit a prior radio-clinic exploration with better anatomical radio-analysis (on the CT-scan). The spectacular appearance of non-missile penetrating head injuries incites a rapid surgery in order to limit complications, particularly infectious ones.
Keywords
Child, Foreign body, Metal, Penetrating brain injury
Introduction
Nonmissile penetrating head injuries (NMPHI) by foreign bodies in children are a rare entity [1,2]. They mostly occur in home accidents, child abuse or attempted-infanticide; while frequently diagnosed incidentally [3,4]. These foreign bodies are more often of wood, eventfully they may in metallic as needles, nails or iron rods [4], suggesting a personalized approach of care. Foreign body injuries in children are most frequent before 3-years-old, around learning period of walking or objects explorations by mouth for infants [5,6]. Several pediatric cases studies have been described worldwide within NMPHI, almost always emphasizing its rarity without any geographic incidence or type of causal foreign body, since quite often linked to violence or road-traffic accidents [1-6]. Also, a well consensus care remains not acquired, although many algorithms have been established since 2016, perhaps due to the lack of data from randomized studies [1]. Our illustrating cases are a useful pretext to highlight more this phenomenon; especially since sometimes foreign bodies can go unnoticed and appearing in children generally hardly plaintive.
Material and Method
Two children with both brain injury due to metal after domestic accident, admitted in Emergency Care Hospital and operated in 2018 and closely followed-up during 3 years were gathered. Their cases were retrospectively reviewed and reported and their features discussed according to Literature data.
Cases Report
The first case was of a 13-month-old infant admitted in 2018 for a penetrating brain injury by a nail (Figure 1). The mechanism was of a slipping fall on a wall under construction during a home game. The nail was masonry rusty one with flat head (5 x 55 mm) implanted in a wall, which had perforated the skull by the flat end; the entry point was the left occipital and the wall end was cut before the admission. There were neither convulsion, loss of consciousness or focal neurodeficit (Initial Glasgow Coma Scale = 15/15). After radiological definitions and the tetanus serum administration, the metallic foreign body long of 5 cm was surgically removed with the remove of bone splinter and duroplasty (Figure 1). There was no neurological deficit or blindness after surgery. The patient discharged after 14 days of antibiotics and without complications. His follow-up was once per week during 1 month and every trimester till 1 year. There was no neurological event until he started school this year 2021-2022.
The second case was of a 12-year-old teen admitted one week after the infant for also a penetrating brain injury by an iron bar (Figure 2). It was of a mangoes-tree fall (around 4 metres) during a household game without loss of consciousness. The iron bar was also implanted on a house under construction. The entry point was the inner canthus of the right orbit with an exit zone at the left pretragal region. The vision was conserved and the left ocular motility difficult to examine (Initial Glasgow Coma Scale = 15/15). The CT-scan showed the intracranial damage as well as the path of the 8 iron rod. This was long of 48 cm, sawn at its base at home before hospital. The tetanus serum was also administrated. Admitted in operating theatre, 15 cm were also sawn before the complete surgical removal as the right-left direction (Figure 2); without craniotomy and with surgical debridement of face wounds. The evolvement was with dysosmia, inconstant left phosphenes and left oculomotor palsy partially regressive among months with a discharge after 14 days of antibiotherapy (Cephalosporin and 5-NitroImidazole). The follow-up was without other particular event.
Discussion
Penetrating brain injuries out of traffic accidents are mostly generated by violence or war [7]. Unexpected cases may occur in adults during work accidents and in children during home playings or domestic accidents; these are about nonmissile penetrating cranial injuries [8]. The insecure children games around building sites may represent a factor of occurrence.
Several items must be taken into account in the management and the prognosis of these injuries, such as the velocity of the impact, the type of object and the entry and exit points of the foreign body. Brain damage increases with velocity in the form of concentric area of necrosis or cavitation and blast. Our cases are of low-velocity injuries different from missile ones, as there are no concentric zones of necrosis or cavitation, but a haemorrhagic necrosis along the wound track [9]. The fall is a common mechanism in young children as noticed in our cases [10,11]; this may result in penetrating head injury especially in case of an unexpected material in the impact area. The height of the fall affects the velocity of the impact. Falls of height above 91 cm (= 3 feet = 2 times height of child) are mostly cause of intracranial lesions in children [10,11].
Anatomical parameters like the entry and exit points, as the track of the penetrating trauma determine the extent of lesions and thus the prognosis of the child. Therefore, a favourable prognosis is guaranteed by the non-involvement of vital centres and large vessels, as it turned out in our two cases [9]. The entry point may be a natural orifice of the skull (orbit, nose, mouth or ear) - as in our infant case - or anywhere on the skull (artificial orifice) by crossing it as in our teenage case [8]. In our first case, no major structure was affected, thus allowing us to consider a good prognosis.
The diagnosis as the removal procedure of intracranial metallic foreign body should be prompt. According to de Holanda and al, the initial Glasgow Coma Scale (GCS) of the patient remains the lead prognostic factor; with very good long-term evolvement for patients of GCS = 14-15. In addition, the prompt removal is defined by the trajectory, size and shape of the projectile. A prior neuroradiologic evaluation should be an overriding concern [8,12]. Some teams recommend a systematic preoperative Angio-CT scan [8]. For us, this should be dictated by the entry and exit points of the projectile adjoining large vessels areas.
The removal of the foreign body proves to be necessary due to the remaining external part of the foreign body, this of course after a good analysis of the anatomy around (large vessels and noble brain structures) [7]. Thus, the surgical approach needs to be as large as possible for a better perioperative control of these, even though there is no brain mass effect. The removal direction usually used to be as a return route with visual control, as in our first case. In the second one, the projectile was withdrawn in the opposite direction cause of the difficulty to achieve a wide approach with wide visual control. This wide approach is mainly recommended in penetrating brain injury such as wide dural reconstruction with craniectomy as exists or not a midline shift [8]. Also in that case, the trajectory of the foreign body passed through the skull base and close to its large vessels and the cranial pairs, particularly the optic nerve and chiasma. Open surgery would have required manipulation of these structures with a non-negligible risk of injury of these. We preferred removing the foreign body without approaching the skull base, for us to be as conservative as possible.
A surgical decisional algorithm proposed in 2016 recommends a single removal in case of injury without transdural attained and a craniotomy with antiepileptic drugs and antibioprophylaxy in case of transdural break-in [8,12]. This was clearly respected in our reported cases. Our team could as well recommend these procedures as much as possible; notwithstanding our case series remains very small and a larger sample size might suggest some nuances of the surgical management. The use of antiepileptic medication and antibiotherapy in NMPHI are questionable so far in Literature. Many teams suggest them (Southern Asia and Eastern Europe, Southern America…) [1,2,7,8]; just like us, in cases of dural breach and brain attain (Craniocerebral wound) at least for a short period to avoid immediate complications: 2 or 3 weeks for antibiotics and at least one month for anticonvulsants.
Complications which cause mortality in early stage are intracerebral haemorrhage, contusion, major vascular injury and meningitis. Late complications maybe avoid by early treatment [7]. Early surgical exploration by a multidisciplinary team approach is essential to attain good recovery and a favorable outcome [11,13].
After 3 and half years of follow-up, we did not notice any high functions changes in both children, as behaviour, psycho-ability, attention or intellect. According to Badhiwala and al, behavioural or neuropsychiatric changes may occur after penetrating head injuries in child; especially in frontal lobe involvement [14].
Conclusion
Nonmissile penetrating brain injuries are of spectacular appearance. In all severe cases, the removal of the projectile remains well codified and must be as early in order to limit complications, particularly infectious ones. The removal requires an anatomical study based on the CT-scan. In view of the low incidence and in order to evaluate the interest of antibiotic prophylaxis and anticonvulsant treatment, it would be necessary to carry out a multicentric trial including craniocerebral wounds with or without foreign bodies.
Statement for Ethics
Ethical approval was not required for this study in accordance with national guidelines.
A written informed consent was obtained from the parents of the two children whom cases are presented, for publication of their medical cases with any accompanying images if applicable.
Establish Facts and Novels Insights
Established facts
• Penetrating head injuries by foreign bodies in children are a rare.
• They are usually of child abuse, home accidents or wars.
• The surgical management and the prognosis depend of the velocity of the impact, the type of object and the entry and exit points of the foreign body.
Novels insights
• Penetrating head injuries in child maybe of falls and low-velocity.
• Low-velocity injuries reduce brain damages.
• The surgical removal should be prompt defined by the trajectory, size and shape of the projectile.
Conflict of Interest Statement
The authors have no conflict of interest to declare.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Contributions
Alain JIBIA: Conceptualization - Writing & Reviewing - Surgery – Supervision; Cyrille CAPEL: Reviewing and Final Approval; Yannick MOSSUS: Surgery - Analysis - Final Approval; Serge NGOUATNA: Anaesthetist - Analysis - Final Approval; Dominique DJOMO TAMCHOM: Anaesthetist - Analysis - Final Approval.
Data Availability Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
- Drosos E, Giakoumettis D, Blionas A, et al. (2018) Pediatric nonmissile penetrating head injury: Case series and literature review. World Neurosurg 110: 193-205.
- Chowdhury FH, Haque MR, Hossain Z, et al. (2016) Nonmissile penetrating injury to the head: Experience with 17 cases. World Neurosurg 94: 529-543.
- Hull KL, Denton-Beaumont R (2019) An unsuspected intracranial foreign body on the acute medical unit. BMJ Case Rep 12: e230010.
- Pelin Z, Kaner T (2012) Intracranial metallic foreign bodies in a man with a headache. Neurol Int 4: e18.
- Passali D, Gregori D, Lorenzoni G, et al. (2015) Foreign body injuries in children: A review Acta Otorhinolaryngol Ital 35: 265-271.
- Gökçek C, Erdem Y, Köktekir E, et al. (2007) Intracranial foreign body. Turk Neurosurg 17: 121-124.
- Tabibkhooei A, Taheri M, Rohani S, et al. (2018) Penetrating brain injury with a metal bar and a knife: Report of two interesting cases. Neuroradiol J 31: 203-206.
- De Holanda LF, Pereira BJA, Holanda RR, et al. (2016) Neurosurgical management of nonmissile penetrating cranial lesions. World Neurosurg 90: 420-429.
- Karim T, Topno M (2010) An unusual case of penetrating head injury in a child. J Emerg Trauma Shock 3: 197-198.
- Burrows P, Trefan L, Houston R, et al. (2015) Head injury from falls in children younger than 6 years of age. Arch Dis Child 100: 1032-1037.
- Farrell CA (2013) Canadian Paediatric Society, Acute Care Committee Management of the paediatric patient with acute head trauma. Paedriatr Child Health 18: 253-258.
- Zyck S, Toshkezi G, Krishnamurthy S, et al. (2016) Treatment of penetrating nonmissile traumatic brain injury Case Series and Review of the Literature. World Neurosurg 91: 297-307.
- Mzimbiri JM, Li J, Bajawi MA, et al. (2016) Orbitocranial low-velocity penetrating injury: A personal experience, case series, review of the literature, and proposed management plan. World Neurosurg 87: 26-34.
- Badhiwala JH, Blackham JR, Bhardwaj RD (2014) Neuropsychiatric changes following penetrating head injury in children. Surg Neurol Int 5: 154.
Corresponding Authors
Alain JIBIA, MD Neurosurgeon, Centre Hospitalier Essos, Avenue Germaine Ahidjo, 5777 Yaoundé; Neurosurgery Unit, Surgery Department of Essos Hospital Centre Yaoundé; Neurosurgery Unit, Surgery Department of Yaoundé Emergency Centre, Cameroon, Tel: (+237)-690849859
Copyright
© 2022 JIBIA A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.