Cavernous Hemangioma of the Temporal Muscle
Abstract
Haemangiomas are benign vascular neoplasms characterized by an abnormal proliferation of blood vessels. These tumours are common in infancy and childhood and commonly involve subcutaneous or mucosal tissues. Fewer than 1% are intramuscular hemangiomas occurring within skeletal muscle, they occur more often in trunk and extremity muscles, whereas involvement of the temporal muscle is extremely rare. Herein, the case is reported of a 42-year-old male who presented with a round, painless mass in the right temporal fossa, which was interpreted as an intramuscular haemangioma after a magnetic resonance imaging scan. The lesion was surgically excised, and histopathologic examination confirmed the diagnosis of cavernous hemangioma. In this report, clinico-pathological findings are described in an additional case of haemangioma involving the temporal muscle, and a review is made of the international literature on this subject.
Keywords
Temporal muscle, Benign tumour, Haemangioma
Introduction
Intramuscular haemangiomas are rare tumours accounting for 0.8% of all haemangiomas and approximately 14% of cases are localized in the musculature of the head and neck. The masseter (36%), followed by the trapezious (24%), are the muscles most frequently affected, whereas intramuscular haemangiomas of the temporalis muscle are extremely rare. Intramuscular hemangioma mostly seen in young adults and no sex preference are noted. According to Scott, hemangiomas arise in abnormal embryonic sequestrations that retain their embryonic characteristic. Minor trauma or excessive muscle contraction are believed to play a role in the growth of the mass by stimulating blood flow in the preexisting tumor [1]. Until now there have been few reports about hemangiomas of the temporal muscle. We add another case of cavernous hemangioma and review of the international literature.
Case Report
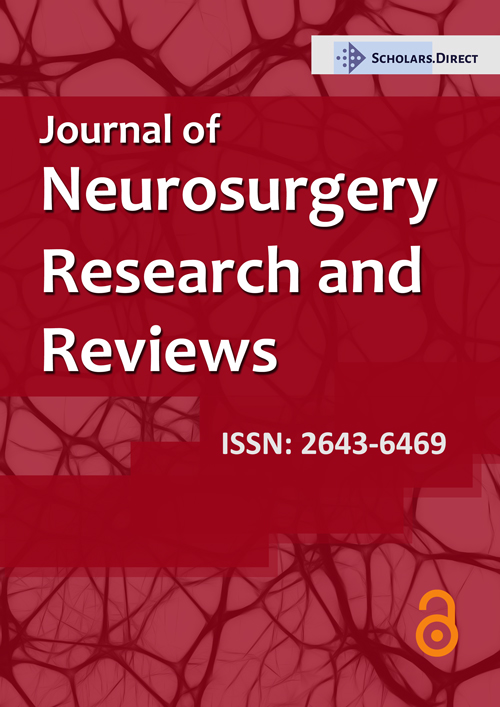
A 42-year-old man, otherwise healthy, was admitted to our departement, with a 4-month history of a slowly growing painless mass in the right temporal region. There were no other symptoms, and no history of trauma. The results of his neurologic and physical examinations were normal, except a solid immobile mass lesion approximately 5 cm in diameter in his right temporal fossa. No pulsation or bruit was observed, the overlying skin was also normal, and no adenopathy was noted. The patient had been treated for headache at a neurosurgical department before he noticed a swelling on his right temporal region. Subsequently, a magnetic resonance imaging (MRI) scan was performed which revealed a 5 × 4 × 2 cm ovoid mass within the right temporal muscle. The tumor had isointense signal on T1 weighted sequences and a high signal on T2 weighted sequences (Figure 1), the mass was not invading the surrounding tissues. Computed tomographic (CT) scan showed no erosion of the bone and no calcifications (Figure 1).
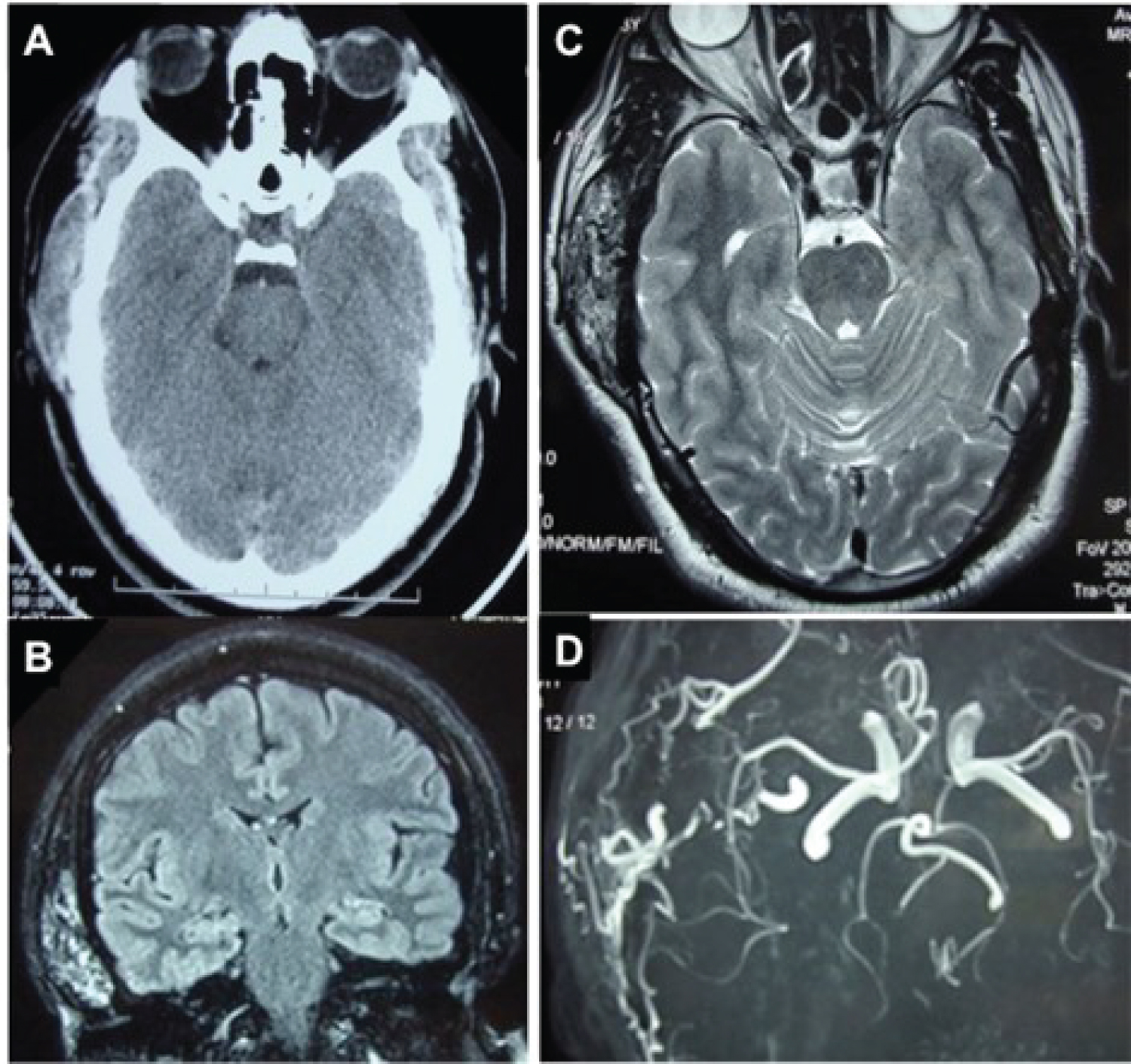
Because there were a cosmetic deformity, growth of the lesion and intractable pain, we decided a surgical treatement. The patient was operated on under general anesthesia, surgical excision was performed through a hemi-coronal flap, skin flap was elevated from the underlying temporal fascia; a dark red soft well-demarcated tumor lying in the temporal muscle was encountered. The lesion was excised totally, there was no evidence of infiltration in the surrounding muscle (Figure 2). Histopathologic examination of the specimen confirmed the diagnosis of cavernous hemangioma. The patient was discharged from the hospital on the third postoperative day. Postoperative follow up during 1-year period showed no recurrence.
Discussion
Intra-muscular haemangiomas were first described by Liston [2] in 1843 and classified in 1972 by allen and enzinger depending on the vessel size [2]. The capillary variant (small vessels) occurs more frequently and represents 68% of intra-muscular haemangiomas, followed by the cavernous (large vessels) and mixed type (small/large vessels) with an incidence of 26% and 6%, respectively [3]. In our patient, pathologic findings revealed a cavernous hemangioma that was identified through cavernous vascular structures divided by hyalinized fibrous septa.
The aetiology of these lesions is unknown, although trauma or hormonal changes are considered important factors in the proliferation of embryonic vascular tissue. Even a congenital theory has been proposed on account of the high incidence of haemangiomas during the first years of life. Intra-muscular haemangiomas usually present as a slow-growing mass with distinct margins, mobile and do not exhibit any of the vascular signs such, discoloration of overlying skin or pulsation. More than 90% of intramuscular hemangiomas are misdiagnosed.
The differential diagnosis includes: Neurofibroma, lipoma, dermoid cyst, enlarged lymph nodes, soft-tissue sarcoma, myositis ossificans and temporal arteritis [4].
MRI is the method of choice in defining the vascular nature of the tumour. On T1 weighted imaging, haemangiomas are iso-intense or hypo-intense to muscle. With T2 imaging, the lesions are hyper-intense on account of the volume of stagnant blood, clearly differentiated from the normal muscle and fibro-fatty septa [5]. CT scan is helpful for evaluation of bone involvement.
Arteriography is helpful in delineating major vascular feeders for pre-operative embolization.
Generally, surgical excision including a rim of normal surrounding tissue is the mainstay of treatment, as it permits a histological evaluation of the mass and it reduces the local recurrence rate [6]. Moreover, careful surgical dissection during excision of a temporal muscle hemangioma is important to prevent injury to the temporal and auricular branches of the facial nerve.
Indications for surgical treatment include: patient age, repeated severe haemorrhagic episodes, site and size of the tumour, depth of invasion, rate of growth, intractable pain, cosmetic deformity and suspicion of malignacy [4]. Heckl, et al., instead, advocate only a strict clinical and radiological follow-up for at least 2 years and reserve surgical treatment only in the presence of capillary haemangioma due to its more aggressive behaviour (high rate of recurrence, invasive growth), in case of lesion progression and when quality of life is reduced (presence of intractable pain, aesthetic problems and functional impairment) [6].
Local recurrence, related primarily to incomplete resection, is different for the three pathological subtypes. Rates of recurrence of 28%, 20%, and 9% have been reported for mixed type, capillary, and cavernous intra-muscular haemangiomas, respectively [7]. There was no recurrence in our patient 6 months after the surgery.
Conclusion
Cavernous hemangiomas are benign vascular tumors that should be suspected when swelling occurs in the temporal region accompanying radiologic findings, which suggests vascular origin. Care should be taken to avoid facial nerve injury even for smaller lesions. Long term clinical and radiological follow up are necessary to detect any relapse.
Conflicts of Interest
The author has no conflicts of interest to declare.
References
- Eryilmaz MA, Varsak YK, Gül Z, et al. (2014) Intramuscular cavernous hemangioma of the temporalis muscle. J Craniofac Surg 25: 1400-1401.
- Bucci T, De Giulio F, Romano A, et al. (2008) Cavernous haemangioma of the temporalis muscle: Case report and review of the literature. Acta Otorhinolaryngol Ital 28: 83-86.
- Giudice M, Piazza C, Bolzoni A, et al. (2003) Head and neck intramuscular haemangioma: Report of two cases with unusual localization. Eur Arch Otorhinolaryngol 260: 498-501.
- To EW, Tsang WM, Pang PC, et al. (2001) Cavernous hemangioma of the temporalis muscle: Report of a case. J Oral Maxillofac Surg 59: 1229-1232.
- Buetow PC, Kransdorf MJ, Moser RP Jr, et al. (1990) Radiologic appearance of intramuscular hemangioma with emphasis on MR imaging. AJR Am J Roentgenol 154: 563-567.
- Heckl S, Aschoff A, Kunze S (2002) Cavernous hemangioma of the temporal muscle. Neurosurg Rev 25: 66-67.
- Lopez-Cedrun JL, Urtasun Fernandez J, Melendez Baltanas J (1996) Hemangioma of the temporalis muscle: A case report and review of the literature. J Oral Maxillofac Surg 54: 1130-1132.
Corresponding Author
Hatim Belfquih, MD, Department of Neurosurgery, Avicenne Military Hospital, 40000, Marrakech, Morocco, Tel: +(212)-6-61-33-86-23.
Copyright
© 2021 Belfquih H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.