A Case of Severe Acute Hyperphosphatemia Secondary to Ingestion of Phosphoric Acid Solution Treated with Continuous Renal Replacement Therapy
Abstract
We report a case of severe acute hyperphosphatemia with serum phosphate levels > 12.92 mmol/L (above laboratory detection levels) in a Filipino gentleman from ingestion of phosphoric acid solution. He also developed hypocalcemia, metabolic acidosis and acute kidney injury. He was treated with continuous renal replacement therapy. His hyperphosphatemia and electrolyte abnormalities improved with dialysis but he subsequently demised due to associated complications from severe caustic injury.
Keywords
Hyperphosphatemia, Continuous replacement therapy, Phosphoric acid solution ingestion
Introduction
Acute hyperphosphatemia due to phosphate load is typically attributed to sodium-phosphate laxatives, tumor lysis syndrome or rhabdomyolysis. It can lead to acute renal failure secondary to acute phosphate nephropathy and in addition cause hypocalcaemic tetany, cardiac arrhythmia and arrest. Treatment usually involves cessation of the offending agent, hydration to enhance renal excretion, oral phosphate binders, and hemodialysis if such measures are not successful [1].
We report a case of severe acute hyperphosphatemia with serum phosphate levels > 12.92 mmol/L (above laboratory detection levels) secondary to ingestion of phosphoric acid based cleaner in an attempt at deliberate self-harm. We are not aware of any cases of acute hyperphosphatemia of such severity in patients with normal renal function, treated with continuous renal replacement therapy that achieved resolution of the electrolyte and metabolic abnormalities.
Case Report
A 41-year-old Filipino gentleman presented to the emergency department (ED) with generalized abdominal pain after intentional ingestion of approximately 100-150 ml of Maintex Lime Go Restroom Cleaner, a phosphoric acid based cleaner, in an attempt at deliberate self-harm. He also reported throat pain with hematemesis. He did not have any significant past medical history and was not on any chronic medications.
On arrival to the emergency department, the patient was alert. On examination, he had a pulse rate of 97 beats per minute and a blood pressure of 123/88 mmHg. He was tachypneic with a respiratory rate of 29 breaths per minute. His posterior pharyngeal wall was noted to be erythematous. Abdominal examination revealed generalized tenderness without guarding or rebound. Bowel sounds werepresent but sluggish. Rectal examination revealed dark coffee ground stools. Cardiovascular and respiratory examination was unremarkable (Table 1).
The admission electrocardiogram (ECG) and chest X-ray were unremarkable.
Our clinical impression was that of acute hyperphosphatemia secondary to phosphoric acid solution ingestion with hypocalcemia, HAGMA from exogenous acid ingestion and lactic acidosis. There were also concerns of gastrointestinal bleed.
We decided to initiate intermittent hemodialysis (IHD) in view of severe metabolic acidosis. Shortly upon admission to the intensive care unit (ICU), the patient developed bradycardia, which led to apulseless electrical activity (PEA) collapse. Cardiopulmonary resuscitation was initiated immediately. He was intubated and mechanically ventilated. He was started on continuous veno-venous hemodiafiltration (CVVHDF) without anticoagulation in view of hemodynamic instability.
His CVVHDF effluent dose was prescribed according to the international guidelines and divided equally between dialysate and replacement fluid. The filter clotted once because of high transmembrane pressure (TMP). His filtration fraction was also elevated. Regional citrate anticoagulation was not ideal in this situation in view of hyperlactemia and hypocalcemia. Hence, CVVDHF was changed to continuous veno-venous hemodialysis (CVVHD), to reduce the risks of further episodes of filter clotting that could potentially delay treatment.
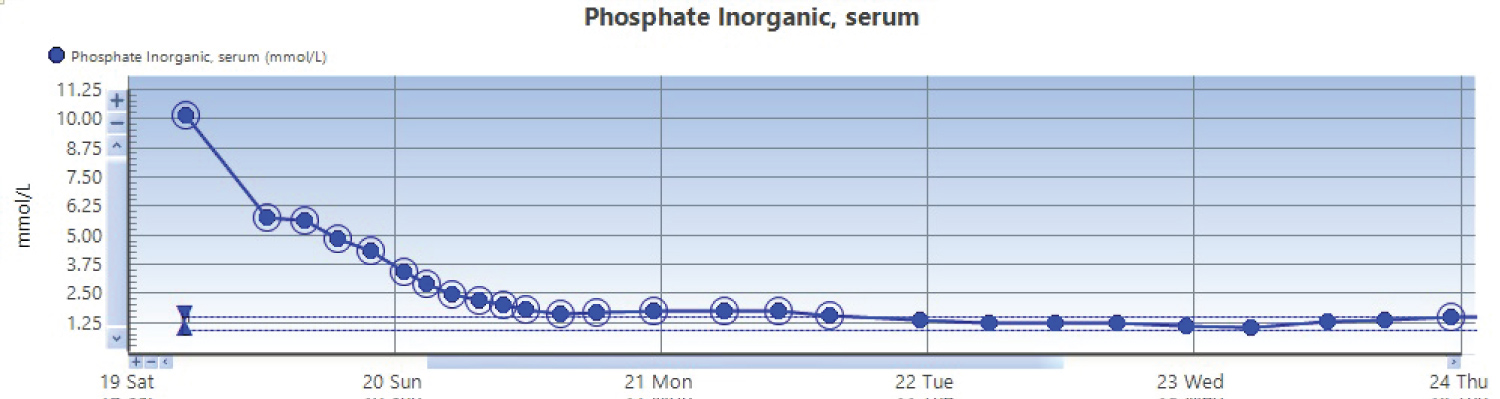
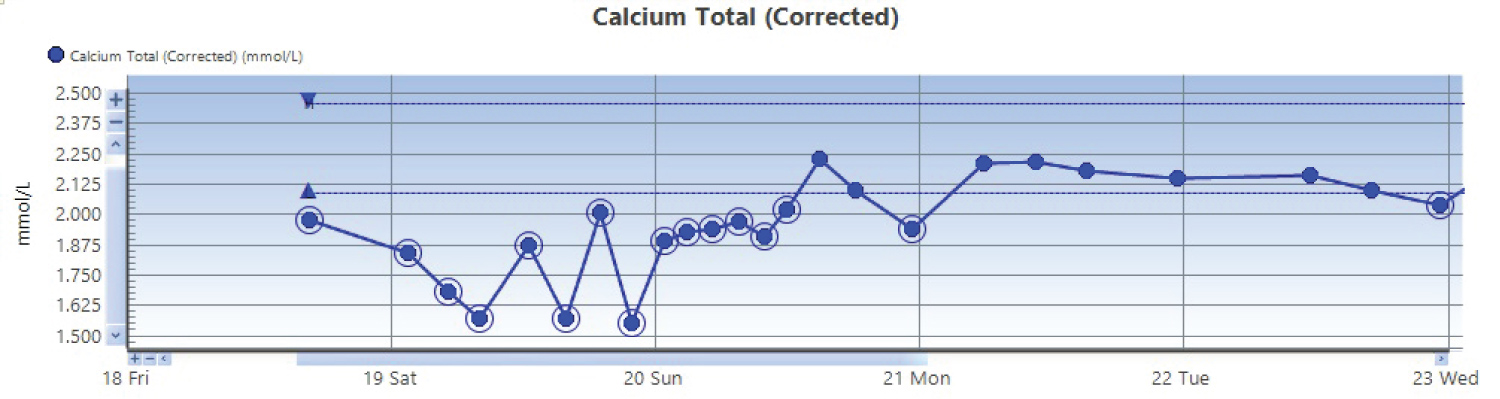
After 4 days of CRRT (CVVHDF and CVVHD), patient's phosphate level dropped to 1.36 mmol/L (Figure 1). Hypocalcemia also resolved with a corrected calcium level of 2.21 mmol/L (Figure 2). His metabolic acidosis, predominantly secondary to lactic acidosis, attributed to hypoperfusion from hemodynamic instabilityand acute liver failure, improved after 5 days on CRRT. However, he continued to have anuricacute kidney injury, which was attributed to acute phosphate nephropathy, septic and ischemic acute tubular necrosis and required CRRT throughout his admission.
Despite improvement in his electrolyte and metabolic abnormalities, he continued to be haemodynamically unstable requiring inotropic support. The patient subsequently demised from other medical issues including hemorrhagic shock secondary to a bleeding duodenal ulcer because of ischemic necrosis, and acute liver failure secondary to ischemic hepatitis. He also had possible intestinal ischemia and ventilator associated pneumonia (VAP) which may have contributed to his demise.
Discussion
Hyperphosphatemia attributed to an acute phosphate load occurs typically due to oral sodium-phosphate laxatives and has been well documented to cause acute phosphate nephropathy and nephrocalcinosis. Its proposed mechanisms include hypovolemia, a large phosphate load at the distal nephron with calcium phosphate precipitation [1]. The symptoms and signs associated with hyperphosphatemia are usually secondary to the associated hypocalcemia. This may include muscle cramps, tetany, paresthesia, seizures, coma, hypotension and arrhythmias. Additionally, acidosis can cause intracellular phosphate to shift extracellularly, increasing urinary losses, further increasing calcium phosphate precipitation.
Reported treatment strategies are varied. Acute extracellular fluid expansion with IV fluids can help increase the urinary excretion of phosphorus, although it should be done judiciously in the patients with acute kidney injury who can be oliguric. Acidosis can be managed with IV sodium bicarbonate. Oral phosphate binders can be used to reduce further absorption. Dialysis can be considered, although one should be aware that IHD is significantly more efficient in phosphate removal than peritoneal dialysis [2].
Caravati (1987) reports a similar case of phosphoric acid ingestion with the patient successfully treated with an oral phosphate binder, aluminum hydroxide. Although the patient's phosphate level was 7.1 mmol/L, which was significantly lower than our patient's and the patient did not have significant caustic injuries [2]. Song, et al. (2021) reports a patient with underlying chronic kidney disease stage 5 presenting with acute hyperphosphatemia (serum phosphate level of 6.23 mmol/l due to non-compliance to medications and dietary indiscretion. The patient was successfully treated with oral phosphate binders and IHD [3].
A study by Tan, et al. compared the effects of CVVHDF and IHD on serum phosphate concentration and showed that CVVHDF induced a greater reduction in serum phosphate during the first 48 hours and conferred superior subsequent control of hyperphosphatemia [4]. It is evident from our case that CRRT is an efficient form of treatment in the setting of severe hyperphosphatemia, especially if the patient is hemodynamically unstable.
It is important to consider dialysis as an early treatment option in cases such as ours where hyperphosphatemia is severe, especially if there is concurrent metabolic acidosis, even if the renal function appears to be normal. Of note, he received CVVHDF for the first 2 days which was changed to CVVHD subsequently in view of concerns of recurrent filter clotting and anticipated disruption in the delivery of therapy. Despite the change in modality, phosphate removal was efficient with both CVVHDF and CVVHD.
Conclusion
Ingestion of phosphoric acid solution can result in acute hyperphosphatemia and metabolic acidosis with associated hypocalcemia and acute kidney injury from acute phosphate nephropathy. Early continuous renal replacement therapy or haemodialysis can potentially reverse the electrolyte abnormalities and reduce the risks of associated complications.
Ethical Disclosures
The team was unable to obtain informed consent from the patient as he had demised during his admission. He is a foreigner to Singapore and we have not been able to contact his next of kin subsequently to obtain consent.
Declaration of Competing Interests
The authors declare that they have no competing interest(s) to disclose.
References
- Jahan S, Lea-Henry T, Brown M, et al. (2019) An Unusual Case of Acute Phosphate Nephropathy. Kidney Int Rep 4: 1023-1026.
- Caravati EM (1987) Metabolic abnormalities associated with phosphoric acid ingestion. Ann Emerg Med 16: 904-906.
- Song SH, Goo YJ, Oh TR, et al. (2021) A Case Report of Very Severe Hyperphosphatemia (19.3 mg/dL) in a Uremic Patient Taking Honey and Persimmon Vinegar. Electrolyte Blood Press 19: 51-55.
- Tan HK, Bellomo R, M'Pis DA, et al. (2001) Phosphatemic control during acute renal failure: intermittent hemodialysis versus continuous hemodiafiltration. Int J Artif Organs 24: 186-191.
Corresponding Author
Pei Shan Lee, Department of General Medicine/Renal Medicine, Sengkang General Hospital, Singapore
Copyright
© 2022 Lee PS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.