Laparoscopic Splenectomy in a 35-Week Pregnant Women with ITP: A Case Report
Abstract
Background: Thrombocytopenia in pregnancy, is defined as platelets less than 150000 per microliter. Idiopathic thrombocytopenic purpura is an acquired autoimmune disorder, characterized by a decrease in plateles less than 150000 per microliter of blood and due to autoantibody binding to platelet antigen causing their premature destruction by the reticuloendothelial system, and in particular the spleen, and finally it causes coagulation disorders. ITP may have a profound effect on pregnancy in the form of severe thrombocytopenia, which may put a person at risk of bleeding to put before and after delivery.
ITP may affect the neonate and expose the neonate to intracranial hemorrhage and long term neurological complications. The final treatment is to remove the spleen. The technique of splenectomy, whether it is performed by laparotomy or by laparoscopic method, plays a significant role in causing complications after surgery. The purpose of introducing this patient is to review the latest evaluation and treatment of resistant ITP in the third trimester of pregnancy.
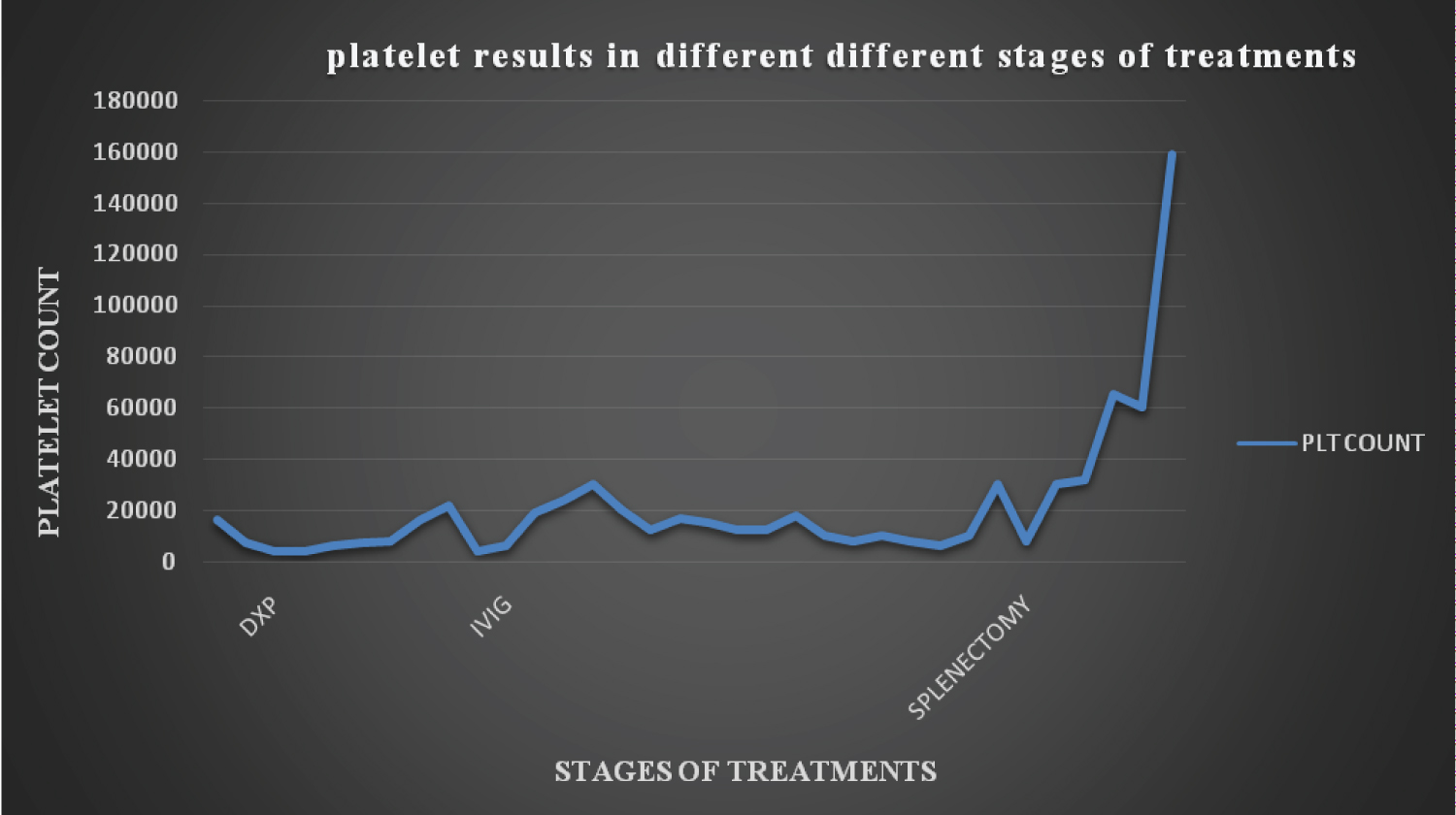
Case report: The patient, a 28-year-old woman, primary gravid, without a history of pregnancy at a gestational age of 35 weeks, with a history of platelet drop in the previous 3 years, platelet drop now, gingival bleeding, epistaxis and petechiae and purpura lesions, was referred from Garmsar Hospital to Kausar Semnan Hospital. The patient was treated with corticosteroid and IVIG, but after 13 days, there was no adequate and stable response to medical treatment, and the patient was diagnosed with treatment-resistant ITP and underwent laparoscopic splenectomy surgery. After surgery, the patient was transferred to the intensive care unit. Platelet one hour after surgery, 32000 per microliter of blood, and 65000 per microliter of blood 6 hours after surgery.
Conclusion: Pregnancy does not increase the incidence or severity of ITP, but platelet drop in pregnancy is a dangerous event. Splenectomy is the second line of treatment in ITP resistant and recurrent to the first line medical treatment. So far, few case reports have been published in the field of laparoscopic splenectomy in pregnancy, most of which were performed in the second or early third trimester, which was done due to ITP or splenic aneurysm, while this case was done in the 35th week of pregnancy due to ITP, which is unique in terms of gestational age.
Keywords
Idiopathic thrombocytopenic purpura, Pregnancy, Laparoscopic splenectomy
Introduction
Thrombocytopenia in pregnancy, is defined as platelets less than 150000 per microliter. If the number of platelets, is between 100000 and 150000 per microliter of blood, mild thrombocytopenia, and if it is less than 100000 per microliter of blood, thrombocytopenia is severe [1,2].
Thrombocytopenia may be clinically idiopathic or more commonly associated with one of the disorders, such as : acquired hemolytic anemia, severe preeclampsia or eclampsia, severe bleeding with blood transfusion, consumption coagulation disorders due to placental abruption, sepsis toxic, lupus erythematosus, antiphospholipid antibodies, megaloplastic anemia caused by severe folate deficiency, drugs, viral infections, allergics and extensive radiation [1].
Primary immune thrombocytopenia, commonly referred to as idiopathic thrombocytopenic purpura [3], is an acquired autoimmune disorder, characterized by a decrease in plateles less than 150000 per microliter of blood and due to autoantibody binding to platelet antigen causing their premature destruction by the reticuloendothelial system, and in particular the spleen, and finally it causes coagulation disorders [4].
ITP, can be divided into 2 types, acute and chronic. In the acute form, children are more affected, suddenly it appears and usually disappears by itself. Its chronic form is gradual and affects mostly adults [5].
In adults, idiopathic thrombocytopenia purpura is seen in young female. 72% of patients are female over 10-years-old and 70% of these female are less than 40-years-old. History and clinical examinations are normal, except for symptoms such as: Bleeding that occur due to platelet disorders. Purpura, epistaxia and gingival bleeding are common, hematuria and gastrointestinal bleeding less common, intracerebral hemorrhage is also rare.
ITP may have a profound effect on pregnancy in the form of severe thrombocytopenia, which may put a person at risk of bleeding to put before and after delivery.
ITP may affect the neonate and expose the neonate to intracranial hemorrhage and long term neurological complications.
The first line treatment is receiving glucocorticoids. The patient first receives high doses of corticosteroids which prevent the formation of platelet antibodies.
Immunotherapy: If severe bleeding occurs or the number of blood platelets needs to increase rapidly, in addition to cortisone, the patient receives special antibodies administered intravenously. They are form the premature breakdown of blood cells prevent [4].
The final treatment in the case of treatment-resistant ITP is to remove the spleen. Spleen removal is recommended when all prescribed drugs have been prescribed or there is life-threatening bleeding. Since the spleen plays a role in the immune system, patients are usually more disposed to infections after surgery [6].
Splenectomy is the standard treatment for ITP patients. The technique of splenectomy, whether it is performed by laparotomy or by laparoscopic method, plays a significant role in causing complications after surgery. The frequency of mortality and complications for splenectomy laparotomy is significantly higher than laparoscopic Splenectomy [7].
The first laparoscopic splenectomy was reported in 1991 [8]. The most common cause of death in laparotomy splenectomy is death due to bleeding.
Laparoscopic splenectomy begins after general anesthesia of the patient. A trocar is placed by the surgeon in the SCM region above the umbilicus in the midline of the abdomen and carbon dioxide gas is injected into the patient's abdomen.
Then, other trocars are placed in different areas of the abdomen, and after positioning the patient, and releasing the splenic vein and artery, the spleen is released, enters the endobag, and is cut into pieces and finally removed. Finally, the drain is fixed for the patient, the gas is discharged, and the fascia and skin are sutured [9].
In this report, a rare case of a 35-week pregnancy with ITP, resistant to treatment, who underwent laparoscopic splenectomy, is introduced. The purpose of introducing this patient is to review the latest evaluation and treatment of resistant ITP in the third trimester of pregnancy.
Case Report
The patient, a 28-year-old woman, primary gravid, with no history of pregnancy, at a gestational age of 35 weeks, with a history of platelet drop in the previous 3 years, for which reason she was hospitalized and was diagnosed with ITP, and was treated with oral prednisolone. She has stopped taking the medicine herself.
A patient with 35 weeks of pregnancy and deficiency of platelets (12000 per microliter of blood), gingival bleeding, epistaxis, petechiae and purpura lesions, was referred from the health center to Garmsar Hospital (July 14th) and 1 unit of platelets was injected for them and the platelets reached 16000 per microliter of blood and the patient was referred to kwosar Semnan hospital (July 15th) to continue the treatment under the supervision of a hematology specialist and in the diagnostic procedures in PBS, no other pathological point was seen, apart from the deficiency of platelets, and the description of the tests is as follows (Table 1).
Echocardiography was also normal (EF: 55%, PAP: 10).
According to pregnancy ultrasound, placental abruption was rejected and no pathological findings were seen in fetus, placenta and uterus. According to ultrasound, the gestational age was 34 weeks and 2 days, and the position of the fetus was cephalic.
The NST performed for the fetus was REACTIVE.
Abdominal and pelvic ultrasound did not show any pathological lesion.
The patient underwent corticosteroid therapy (dexamethasone, 40 mg, daily/up to 4 days) and IVIG injection (60 gr daily/up to 3 days), Intramuscular injection of Rho(D)immune globulin (3000 microgram/for a day) and Oral azathioprine (150 mg daily/up to 10 days), It was done, and after 13 days, there was no proper and stable response to medical treatment, so the patient was diagnosed with treatment-resistant ITP (with 8000 platelets). For splenectomy, a surgical consultation was requested.
On July 27, the patient underwent laparoscopic splenectomy surgery in the presence of a gynecologist and a neonatologist to manage possible preterm labor.
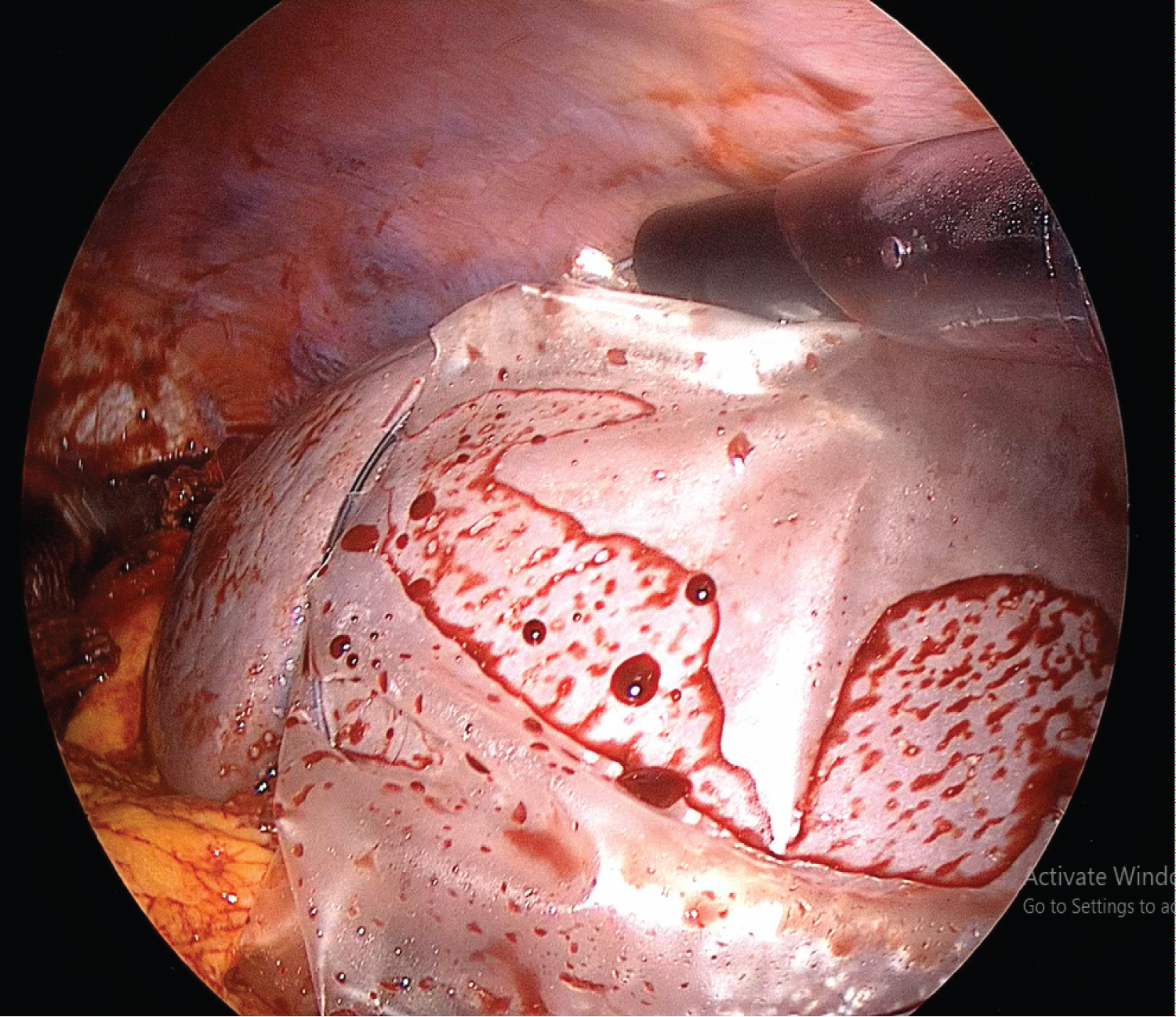
Under general anesthesia, prep and drape were performed, Then, using the Has son method, a size 10 trocar was inserted in the midline 5 cm above the umbilicus, and carbon dioxide gas was injected into the abdomen through it. Then through that camera lens 30 was entered into the abdomen and another size 10 trocar was inserted in the left sub costal region and a size 5 trocar was inserted in the subxiphoid region under the observation of the camera. After opening the LESSER SAC, by opening the gastrosplenic ligament with a ligature, the tissue and adhesions around the splenic umbilicus were dissected with a ligature and then the splenic artery was double ligated with a golden clips (Figure 1) and the injection of 1 unit of platelet apheresis was started immediately.
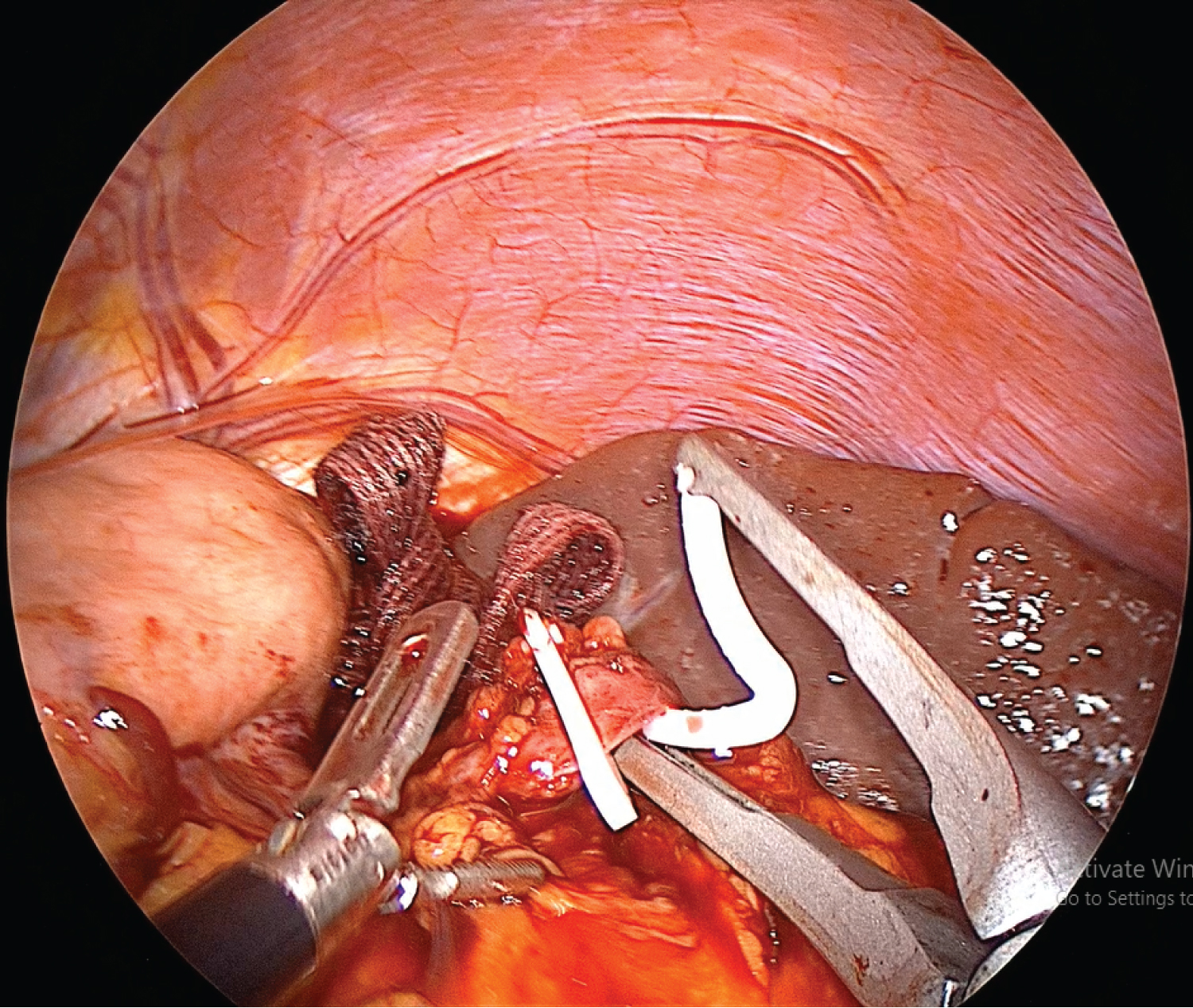
Then 9 units of RD platelets were injected and the splenic vein was double ligated with golden clips. After ensuring the absence of another vascular branch in the splenic umbilicus the splenic umbilicus and then the splenocolic, splenornal and splenophrenic ligaments were separated with a ligature and the spleen was freed. Then the spleen entered the endobag (Figure 2) and it was removed piece by piece from the size 10 trocar in the left sub costal area.
After ensuring complete hemostasis in the surgical site, the intra-abdominal gas discharged and the trocars were removed. Then the wound was treated with trocars, sutures and dressings, and the conscious patient was transferred to recovery.
In recovery, NST and pregnancy ultrasound (BPP: 8.8) were performed and the complete health of the fetus was confirmed and the patient was transferred to the intensive care unit.
Platelet one hour after surgery, 32000 per microliter of blood and 65000 per microliter of blood 6 hours after surgery was reported (Figure 3).
The patient was PO 6 hours after the surgery and was discharged from the hospital 48 hours later (July 29) with a good general condition to continue the pregnancy and plan for NVD.
Discussion
Pregnancy does not increase the incidence or severity of ITP, But the drop of platelets in pregnancy becomes a dangerous event due to the possibility of uncontrolled bleeding before, during and after delivery, So that according to the American hematology guidelines, a platelet drop of less than 10,000 at any time of pregnancy or less than 30,000 at the time of bleeding after the second trimester requires immediate treatment [4,10,11].
Corticosteroid and IVIG are the first line treatment for ITP in pregnancy. Anti-D immune globulin is also among the cost-effective treatments with appropriate response in Rh-positive pregnant patients. Immunosuppressive drugs are usually used in non-pregnant patients due to the possibility of being teratogenic, but in cases where the probability of benefit is greater than the possible risks, they are used in pregnant people to a limited extent [4,10,11].
Splenectomy is the second line of treatment in ITP resistant and recurrent to the first line medical treatment. The rate of response to treatment in people who underwent splenectomy is over 90%, in addition, the patient stays away from the possible side effects of medical drugs [10,11].
Laparoscopic splenectomy is the preferred method of splenectomy for several reasons, including smaller surgical incision, faster recovery, and less pain. The most important challenge in laparoscopy is the tolerance of the mother and the fetus to create pneumoperitoneum, which increases the possibility of miscarriage (5% in the second trimester and 12% in the first trimester), maternal and fetal acidosis (especially with CO2 gas). It seems that the laparoscopic method for preterm labor is without risk, however, the preferred time for laparoscopy is the second trimester of pregnancy. One of the possible risks for laparoscopy is the risk of damage to the uterus with the trocar, especially in the third trimester, which is minimized by placing the trocar in the open method (HASSON) [12].
Another challenge in laparoscopic splenectomy is the possibility of the presence of a subsplenium, which is less likely to be seen and accessed due to the large uterus and low vision. 15 to 30% of the general population has a subsplenium [13].
So far, few case reports have been published in the field of laparoscopic splenectomy in pregnancy, most of which were performed in the second or early third trimester, which was done due to ITP or splenic aneurysm, while this case was done in the 35th week of pregnancy due to ITP, which is unique in terms of gestational age.
References
- Cunningham F, MacDonald P, Gant N, et al. (1997) Endocrine disorders. Williams Obstetrics (20th edn), Stamford, CT: Appleton & Lange 1223-1238.
- Burrow GN, Duffy TP, Copel JA (2004) Medical complications during pregnancy: Saunders.
- Cines DB, Bussel JB (2005) How i treat idiopathic thrombocytopenic purpura (ITP). Blood 106: 2244-2251.
- George JN, Woolf SH, Raskob GE, et al. (1996) Idiopathic thrombocytopenic purpura: A practice guideline developed by explicit methods for the American Society of Hematology. Blood 88: 3-40.
- Stasi R, Evangelista ML, Stipa E, et al. (2008) Idiopathic thrombocytopenic purpura: Current concepts in pathophysiology and management. Thromb Haemost 99: 4-13.
- Kojouri K, Vesely SK, Terrell DR, et al. (2004) Splenectomy for adult patients with idiopathic thrombocytopenic purpura: A systematic review to assess long-term platelet count responses, prediction of response, and surgical complications. Blood 104: 2623-2634.
- Doan CA, Bouroncle BA, Wiseman BK (1960) Idiopathic and secondary thrombocytopenic purpura: Clinical study and evaluation of 381 cases over a period of 28 years. Ann Intern Med 53: 861-876.
- Delaitre B, Maignien B (1991) Splenectomy by the laparoscopic approach. Report of a case. Presse Med 20: 2263.
- Mahon D, Rhodes M (2003) Laparoscopic splenectomy: Size matters. Ann R Coll Surg Engl 85: 248-251.
- Eslick R, McLintock C (2020) Managing ITP and thrombocytopenia in pregnancy. Platelets 31: 300-306.
- Griffiths J, Sia W, Shapiro AJ, et al. (2005) Laparoscopic splenectomy for the treatment of refractory immune thrombocytopenia in pregnancy. J Obstet Gynaecol Can 27: 771-714.
- Hunter J, Swanstrom L, Thornburg K (1995) Carbon dioxide pneumoperitoneum induces fetal acidosis in a pregnant ewe model. Surg Endosc 9: 272-279.
- Rudowski WJ (1985) Accessory spleens: Clinical significance with particular reference to the recurrence of idiopathic thrombocytopenic purpura. World J Surg 9: 422-430.
Corresponding Author
Siavashmasoumi, Department of Surgery, Semnan University of Medical Sciences, Semnan, Iran
Copyright
© 2023 Siavashmasoumi, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.