Routine Intraoperative Cholecysto-Cholangiogram: A Retrospective Study
Abstract
Background: Laparoscopic cholecystectomy remains the gold standard treatment for symptomatic cholelithiasis, acute and chronic cholecystitis. Intraoperative cholangiogram is performed during the procedure in order to visualize the biliary tree and detect filling defects and/or aberrant anatomy. Routine use of cholangiogram remains controversial. The objective of this study was to analyze the success rate at obtaining a routine cholangiogram via an intraoperative cholecystic (IOCC) approach and analyzing its outcomes.
Methods: We studied retrospectively all laparoscopic cholecystectomy cases done by Steward Surgical Specialist Group at Mountain Vista Medical Center during 3 years from November 2017 to November 2020. Laparoscopic cholecystectomy was performed in 304 patients, 219 female and 85 male patients. The mean age was 49.4 years old (range 18-89 years old). The pre-operative diagnoses included symptomatic cholelithiasis, acute and chronic cholecystitis and biliary dyskinesia. The success rate at obtaining an IOCC during surgery was calculated. The reasons for an incomplete/failed and/or aborted IOCC were also recorded. Findings and complications including cystic duct leaks and common bile duct injuries were recorded as well.
Results: A total of 304 cases were reviewed. Of the 277 attempted IOCC cases, 268 were successfully performed and completed (96.8% success rate). The nine incomplete IOC were due to technical difficulties. In 24 cases IOCC was not performed due to severe gallbladder inflammation. Two patients had a contrast allergy and one was not done due to pregnancy. Incidental CBD stones and aberrant anatomy were found in 7 patients. None of the laparoscopic cases had to be converted to open. A total of 3 cystic duct leaks were reported and treated conservatively with ERCP stent placement and drains, however, no major common bile duct injuries were reported.
Conclusions: According to our data, IOCC was successfully completed in 96.8% of all cases attempted. The average time exposed to radiation was minimal. We were able to find aberrant anatomy and common bile duct stones in 7 patients. Bile duct injury rate was reported below the average nationally reported. Therefore, the use of IOCC proved to be a relatively fast, reliable and helpful study to use routinely in laparoscopic cholecystectomy cases.
Introduction
Different methods of performing laparoscopic cholangiography, either through the gallbladder or via cannulation of the cystic duct, have been described [1-11]. Most surgeons use a variation of cystic duct cholangiography, which can be time-consuming, especially when experience is limited, and bile duct injury may be caused during attempts to cannulate the cystic duct [2,5,7,8,11]. The aim of this study was to analyze the success rate at obtaining a routine cholangiogram via an intraoperative cholecystic (IOCC) approach and analyzing its outcomes.
Patients and Methods
This is a 3 year retrospective study of laparoscopic cholecystectomy with intraoperative cholecysto cholangiography performed by Steward Surgical Specialist Group at Mountain Vista Medical Center between November 2017 and November 2020. Laparoscopic cholecystectomy was completed in 304 patients with preoperative diagnosis of symptomatic cholelithiasis, acute and chronic cholecystitis and biliary dyskinesia. There were 219 women and 85 men aged between 18 and 89 years, with a mean age of 49.4 years. The risks and benefits were discussed with each patient and surgical informed consent was obtained. Of the 304 patients, there were 277 attempted IOCC cases and 268 were successfully performed.
Surgical Technique
We access the abdomen via a modified has son technique. We start by making a 12 mm incision in the supraumbilical area. Using the bovie electrocautery, we dissect down to the anterior abdominal wall fascia. A small incision is made in the fascia. The fascia is grasped with two Kocher clamps. An 11 mm trocar is placed using the laparoscopic camera and opt view under direct visualization. Once inside the abdomen, pneumoperitoneum is achieved with carbon dioxide to 12-14 mm Hg. A second 11 mm trocar is placed in the subxiphoid region and two 5 mm trocars in the right flank. All trocars are placed under direct visualization. At this point, a cholangiocatheter or laparoscopic aspiration needle is used to perform the intraoperative cholangiogram.
The operating room technician prepares the cholangiocatheter with a way 3-way stopcock connected to the open lumen of the cholangiocatheter. A 40-mL syringe filled with saline connected to the straight end of the stopcock and a 40-mL syringe filled with dilute iodinated contrast is connected to the 90-degree side of the stopcock. The catheter was pre-flushed with saline to eliminate any air bubbles, and the stopcock is turned off toward the open lumen to prevent any air bubbles from entering the cholangiocatheter. A 5 mm grasper is passed through the midaxillary port under direct visualization, to hold the gallbladder fundus near the anterior abdominal wall. The cholangiocatheter/needle aspirator is passed through the midclavicular port under direct vision, then placed into the lumen of the gallbladder at the fundus.
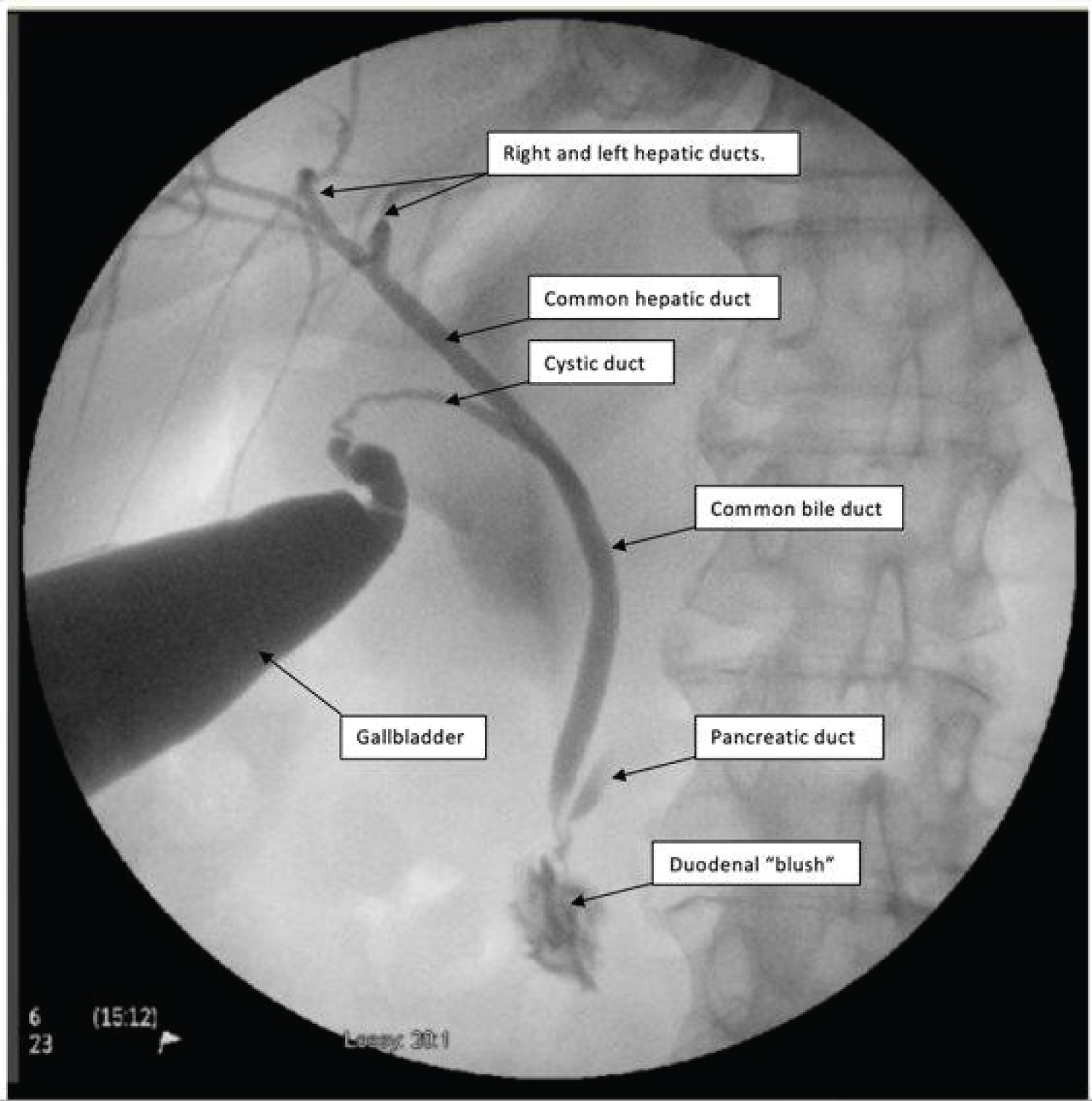
A few milliliters of bile is withdrawn to establish satisfactory position of the needle. About 20 ml of contrast medium is injected as X-ray images are taken using C-arm radiographic system (Figure 1). If the common bile duct is not opacified after 40 mL of contrast, 20 mL of saline is also injected to encourage emptying into the common duct. After visualization of the cholangiogram, the gallbladder is partly decompressed by aspirating through the catheter prior to its removal. Cholecystectomy then proceeded in a routine fashion. Each cholangiogram was analyzed for good filling of contrast through the cystic duct, common bile duct and hepatic radicles, with flow into the duodenum.
Results
A total of 304 patients underwent laparoscopic cholecystectomy. Of those, 27 cases did not undergo an IOCC. Of the 277 attempted IOCC cases, successful visualization was obtained in 268 (96.8%) and 9 cases reported an incomplete IOCC. The results are summarized in (Table 1). The main reason for failure to perform an intraoperative cholangiogram was increased inflammation and adhesions in the setting of acute and chronic cholecystitis. One patient suffered from gallstone pancreatitis, and one patient had a gangrenous gallbladder. One patient was pregnant, and two patients had contrast allergy. In 9 cases, the cholangiography was aborted due to technical difficulties during the operation. Of the 268 successful IOCC, there were 7 patients who demonstrated aberrant biliary anatomy and choledocholithiasis.
One patient received 1 mg of glucagon due to suspected stone impaction in the distal common bile duct, and another patient had a dilated common bile duct without evidence of gallstone or obvious mass lesions. Some of the aberrance in the biliary anatomy were a small common bile duct measuring between 2-3 mm, a short cystic duct, a small and long cystic duct with a low insertion into the common bile duct. Another case showed a cystic duct which coursed posteriorly to the gallbladder, and one more case demonstrated a cystic duct which entered the common bile duct anteriorly. None of the laparoscopic cholecystectomy cases were converted to an open procedure. A total of three cystic duct leaks were reported and treated with ERCP stent placement and drains. Furthermore, no major common bile duct injuries were reported (Table 2).
Discussion
Intraoperative cholangiography during laparoscopic cholecystectomy is a valuable procedure that provides visualization of the biliary tree, recognizes stones in the common bile duct and other pathology or anatomical variations that might be missed. IOC is commonly performed by cannulating the cystic duct, which often requires surgical up skilling. In the setting of increased inflammation or when the duct is narrow and short, cystic duct cholangiography can become challenging because of the difficulties involved in cannulating the cystic duct, which can result in complications, such as bile duct injuries [3]. In light of this fact, routine intra-operative cholangiography (IOC) is often declined by surgeons and a policy of selective cholangiography is adopted [1,2]. An alternative to performing cholangiography is cholecysto-cholangiography. It is a simple technique that requires puncture of the gallbladder compared with cannulation of the cystic duct [3,4]. This procedure takes place at the beginning of the operation and therefore, unlike cystic duct cholangiography, anatomical variations such as a short cystic duct or a thin common bile duct can be seen prior to dissection, whereby possible iatrogenic injury to the hepatic or common bile duct can be avoided. In our present study, 7 patients demonstrated aberrant anatomy and choledocholithiasis.
We observed short cystic ducts, a low inserting duct, and a posteriorly coursing duct. In some cases, a small common bile duct measuring between 2-3 mm was noted and other cases demonstrated a dilated common bile duct without evidence of gallstone or obvious mass lesions. According to our data, IOCC was successfully completed in 96.8% of all attempted cases and no bile duct injuries were reported. The advantage of IOCC is that it shows the length of the cystic duct and the presence or absence of anatomical variants before Calot’s triangle is even approached [7]. Additionally, unsuccessful cholecysto-cholangiography does not preclude the use of cystic duct cholangiography later in the operation [3,6-7].
In a randomized controlled trial comparing cholecysto-cholangiography and cystic duct cholangiography, Wills, et al. demonstrated that the CCC group had 2.3 times the radiation exposure of those undergoing CDC [6]. In contrast, this study showed that the average exposure time to radiation was minimal and the amount of radiation did not exceed the threshold of 2 Gy for skin damage [11]. One case had an IOCC fluoroscopic time of 1 minute and 24 seconds due to possible distal choledocholithiasis and glucagon administration. This study demonstrates that cholecysto-cholangiography is a safe, simple, and effective method of intra-operative cholangiography and the acceptance of this procedure may encourage more surgeons to perform cholangiography during laparoscopic cholecystectomy.
References
- Horwood J, Akbar F, Davis K, et al. (2010) Prospective evaluation of a selective approach to cholangiography for suspected common bile duct stones. Ann R Coll Surg Engl 92: 206-210.
- Livingston EH, Miller JA, Coan B, et al. (2005) Indications for selective intraoperative cholangiography. J Gastrointest Surg 9: 1371-1377.
- Köksal E (2001) Cholecystocholangiography during laparoscopic cholecystectomy. Surg Today 31: 877-880.
- Glättli A, Metzger A, Klaiber C, et al. (1994) Cholecystocholangiography vs. cystic duct cholangiography during laparoscopic cholecystectomy. A prospective controlled trial. Surg Endosc 8: 299-301.
- Fox AD, Baigrie RJ, Cobb RA, et al. (1996) Peroperative cholangiography through the gallbladder (cholecystocholangiography) during laparoscopic cholecystectomy. Surg Laparosc Endosc 6: 22-25.
- Wills VL, Jorgensen JO, Hunt DR (2000) A randomized controlled trial comparing cholecystocholangiography with cystic duct cholangiography during laparoscopic cholecystectomy. Aust N Z J Surg 70: 573-577.
- Daoud M, McCallum MJ (1999) An easy and effective method of cholangiography in laparoscopic cholecystectomy: laparoscopic cholecystocholangiography. Aust N Z J Surg 69: 138-140.
- Karthikesalingam Alan, Markar Sheraz, Weerakkody Ruwan, et al. (2009) Radiation exposure during laparoscopic cholecystectomy with routine intraoperative cholangiography. Surgical endoscopy 23: 1845-1848.
- Shailesh Mohandas, Ajo Kureekattu John (2010) Role of intra operative cholangiogram in current day practice. International Journal of Surgery 8: 602-605.
- Mirizzi PL (1937) Operative cholangiography. Surg Gynecol Obstet 65: 702-710.
- Jaschke, Werner, et al. (2017) Radiation-induced skin injuries to patients: What the interventional radiologist needs to know. Cardiovasc Intervent Radiol 40: 1131-1140.
Corresponding Author
Peter Zajac P, DO, General Surgery Department, Midwestern University, USA.
Copyright
© 2022 Lino HA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.