Outpatient Robotic-Assisted Simple Prostatectomy (O-RASP): A New Era for Large BPH Surgery?
Surgical treatment of large benign prostatic hyperplasia (BPH) is applied worldwide. Contemporary options include open simple prostatectomy (OSP) (either by transvesical or retropubic route), bipolar TURP, laser enucleation with HoLEP, or ThuLEP, robotic-assisted simple prostatectomy (RASP) and laparoscopic simple prostatectomy (LSP) [1-4].
The transurethral enucleation technique provides some advantages-mainly related to the endoscopic approach. Significant limitations though, are the availability of this technology and the relatively long learning curve for having proficiency [5].
Both RASP and LSP (labeled as minimally invasive simple prostatectomy-MISP) reproduce the open technique while offering less morbidity: Lower estimated blood loss (EBL) and shorter hospital stay length and length of catheter use [6]. Besides, technology and surgical expertise required to MISP are largely available in the U.S and Europe, and comparable functional outcomes (Qmax and IPSS), were described when comparing with OSP. Despite this, the MISP approach still being classified in the EUA guidelines as: "Techniques under investigation" [7]. Some reasons would be the relative lack of studies demonstrating its safety, efficacy, and reproducibility. However, when considering other urologic procedures in which robotic procedure also reproduces the open technique, a strong trend favoring the use can be noted. Further, the benefits of robot use among these last procedures remain uncertain in some cases. The usual adenoma's large volume often brings some troubles to manipulate and remove it from the abdomen, which could partially explain these differences.
When comparing MISP and OSP, the intrinsic benefits of the minimally invasive procedures arise as lower rates of incision pain, infection, and incisional hernia. However, even in the MISP technique, the EBL stills representing a concern ranging from 60-800 cc in some series [4]. Some studies also report a transfusion rate of 6.4% [8]. In addition, postoperative hematuria with clot retention is described in 6.5% of cases, with some requiring reoperation, which in turn increases the morbidity and the need for bladder irrigation [9].
Considering that this perioperative blood loss represents the Achilles' heel of simple prostatectomy, we developed a modified RASP (TST-RASP) as an attempt to improve this limitation [10]. Preliminary results of TST-RASP were presented at AUA 2019 when we compared 10 cases of conventional RASP versus TST-RASP. In this pilot study, we observed significant advantages favoring TST-RASP as a shorter need for continuous bladder irrigation (mean: 1.1 vs. 0.5 days; p < 0.001) and hospital stay length (mean: 2.2 vs. 1.7 days; p = 0.03). The overall EBL was 480 cc, and no patients required transfusion or clot evacuation in this study.
Now, going forward, considering prostate irrigation, the blood loss described during enucleation procedures and evidence coming from prostate embolization studies, we introduce the concept of maximum hemostatic control during TST-RASP. In other words, to achieve an excellent visualization and minimum blood loss, we have included the bilateral hypogastric artery clamping during enucleation. After performing ten initial cases, the results obtained are encouraging. We have noted a better visualization during adenoma enucleation and a time reduction during this step. The mean blood loss was 200 cc, and the mean hospital stay was 1.5 days.
The observed benefits could allow us to propose a fast track model for this surgery (as an outpatient l or one-day stays surgery: "O-RASP"). The TST-RASP can be performed using pure laparoscopy as well, but the robotic platform makes the reconstructive surgical steps easier.
The proposed models for TST-RASP are the following steps: (Specific surgical modifications in black bold)
1. 5-6 trocar approach for da Vinci Xi docking.
2. Bladder drop and Retzius space exposure.
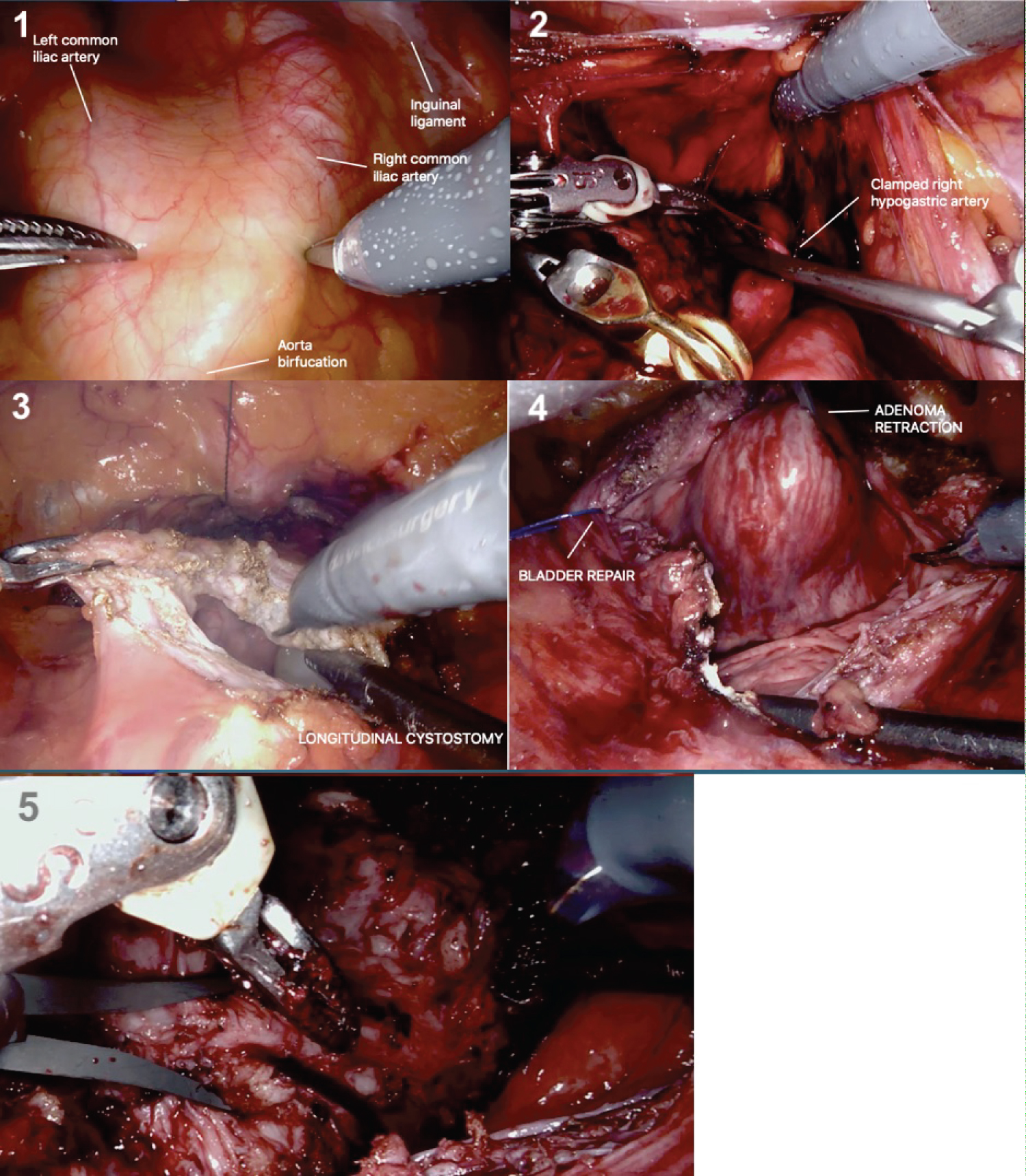
3. Dissection, repair and clamping the bilateral hypogastric artery using bulldogs in order to achieve a maximal control of prostate perfusion during enucleation (Figure 1).
4. Incision opening the bladder wall and prostate capsule until the apex (Transvesical capsular approach as described by Mariano, et al. [11]).
5. Stay sutures to retracted bladder laterally allowing better visualization of the prostate adenoma.
6. Enucleation should start at an avascular median plane (usually at 12 h) dissecting then to the lateral, posterior, and distal direction. We propose the tenaculum use in order to grip and retract the adenoma during the surgery. Monopolar scissors and bipolar Maryland complete the set installation.
7. Just after the adenoma resection, some hemostatic agents can be applied over the surface of the capsule, and bulldogs clamps are removed off.
8. At this point, some additional hemostatic sutures may be needed to achieve the hemostasis.
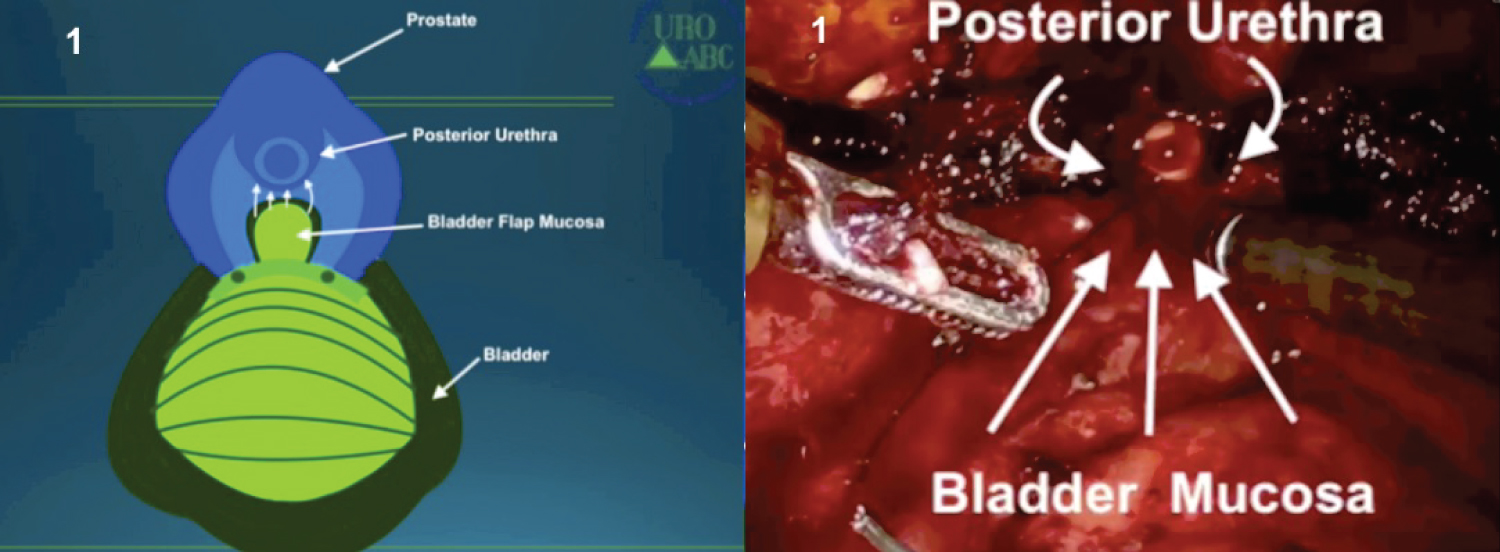
9. The step now is the advancement of a bladder mucosa flap until the posterior part of the prostatic urethra. A Van Velthoven anastomose is performed, achieving the link between the posterior bladder neck and the posterior urethra (Figure 2).
10. Passage of indwelling urethral catheter 22F with slow continuous bladder irrigation (usually during only the first 6 hours).
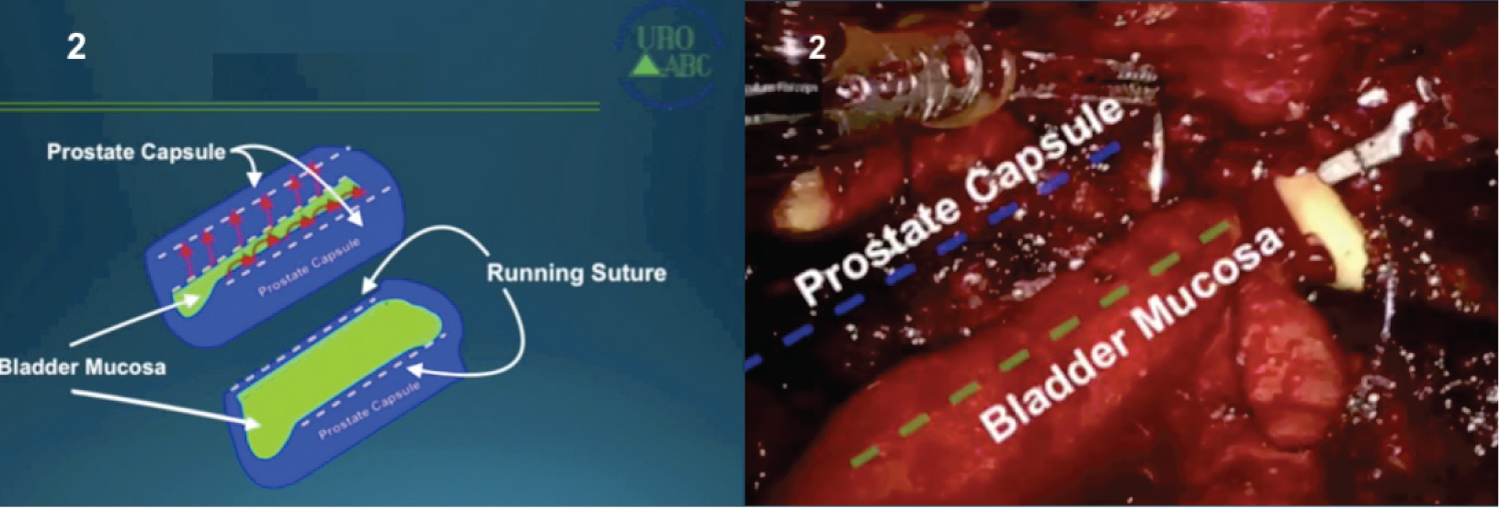
11. Running suture between the advanced mucosa and the prostatic capsule bilaterally (Figure 3). The prostate capsule should be isolated from the rest of the urinary tract and reconstruction obtained resembles a tunnel-Tunnel Shaped Trigonization (TST).
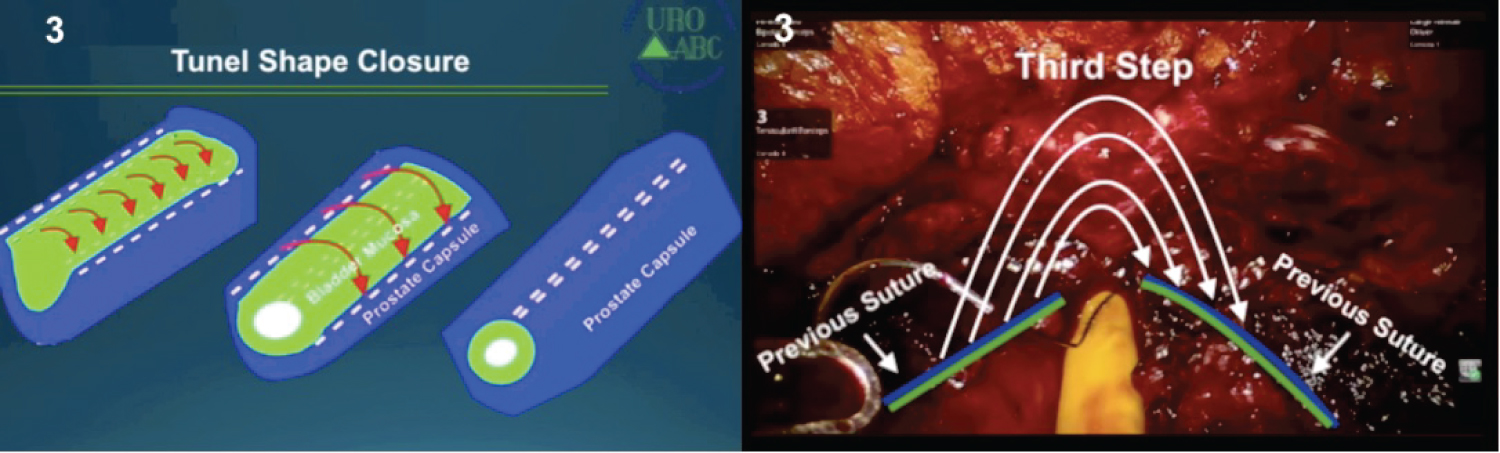
12. Finally, we close with 3-0 v-lok both sides of the capsule and bladder mucosa interiorly (Figure 4).
Usually, the hospital discharge is scheduled after 24 h of hospital stay with a bladder catheter but without irrigation or additional care. The catheter removal is scheduled for the postoperative day 7-10.
In conclusion, modified RASP seems an up-and-coming option to treat large adenomas, probably offering reduced morbidity and hospital stay when considering previous reports from classical OSP and MISP. Further studies, including those recent technical modifications, will elucidate the rule of RASP in this setting.
References
- Carneiro A, Sakuramoto P, Wroclawski ML, et al. (2016) Open suprapubic versus retropubic prostatectomy in the treatment of benign prostatic hyperplasia during resident’s learning curve: A randomized controlled trial. Int Braz J Urol 42: 284-292.
- Xie J, Tan Y, Wang F, et al. (2014) Extraperitoneal laparoscopic adenomectomy (Madigan) versus bipolar transurethral resection of the prostate for benign prostatic hyperplasia greater than 80 ml: Complications and functional outcomes after 3-year follow-up. J Endourol 28: 353-359.
- Sotelo R, Spaliviero M, Garcia-Segui A, et al. (2005) Laparoscopic retropubic simple prostatectomy. J Urol 173: 757-760.
- Sotelo R, Clavijo R, Carmona O, et al. (2008) Robotic simple prostatectomy. J Urol 179: 513-515.
- Kampantais S, Dimopoulos P, Tasleem A, et al. (2018) Assessing the learning curve of holmium laser enucleation of prostate (HoLEP). A systematic review. Urology 120: 9-22.
- Sorokin I, Sundaram V, Singla N, et al. (2017) Robot-assisted versus open simple prostatectomy for benign prostatic hyperplasia in large glands: A propensity score-matched comparison of perioperative and short-term outcomes. J Endourol 31: 1164-1169.
- EAU Guidelines: Management of Non-neurogenic Male LUTS.
- Lucca I, Shariat SF, Hofbauer SL, et al. (2015) Outcomes of minimally invasive simple prostatectomy for benign prostatic hyperplasia: A systematic review and meta-analysis. World J Urol 33: 563-570.
- Autorino R, Zargar H, Mariano MB, et al. (2015) Perioperative outcomes of robotic and laparoscopic simple prostatectomy: A European-American multi-institutional analysis. Eur Urol 68: 86-94.
- Tobias-Machado M, Pazeto CL, Faria EF, et al. (2019) Robot-assisted simple prostatectomy with tunnel-shaped trigonization (RASP-TST) - A novel technique. Int Braz J Urol 45: 858.
- Mariano MB, Graziottin TM, Tefilli MV (2002) Laparoscopic prostatectomy with vascular control for benign prostatic hyperplasia. J Urol 167: 2528-2529.
Corresponding Author
Marcos Tobias-Machado, Department of Urology, Faculdade de Medicina do ABC, Santo André, Brasil
Copyright
© 2021 Machado MT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.