Tuberculosis Meningitis in Immunocompromised Patient on Rituximab
Abstract
A 66-year-old patient of asian background from the US was admitted with confusion and behavioral changes for the last 10 days. The patient was on rituximab for RA (Rheumatoid arthritis). He had a normal computed tomography (CT) head and blood tests showed hyponatremia and acute kidney injury. Cerebrospinal fluid (CSF) showed raised CSF pressure 30 cmH20, raised protein and considerably high lymphocyte count. Mycobacteria tuberculous was isolated from one of her sputum cultures after having several negative sputum cultures, and consequently, the patient was treated for tuberculous meningitis. During admission, he had worsening of GCS (Glasgow coma scale), and he was admitted to ITU (intensive care unit) where he developed acute ischaemic stroke. He was treated for acute infarct and TBM (tuberculous meningitis), and was discharged on anti-tuberculous medications. It was a unique presentation in an immunocompromised patient with sudden deterioration and confusion, however, without neck stiffness or typical meningitis features. His condition improved with the commencement of the anti-tuberculosis therapy and was discharged from the hospital, and the patient traveled back to the US (United States) following discharge. During his stay, he was started on anti-tuberculous therapy early on due to high suspicion of Tb. The positive sputum culture was reported only after he had traveled back to the US and the same was conveyed to the patient’s GP (general practitioner) in the US.
Background
Tuberculosis meningitis is an uncommon presentation and can vary from changes in behavior to neurological symptoms, including photophobia, headache, neck stiffness, limb weakness. It is relatively more common in patients who are immunocompromised, HIV (human immunodeficiency virus) patients, and patients from high risk such as TB [1,2]. One-third of the world’s population is infected with latent Tb, and these individuals carry only a 10% risk of developing the active disease in their lifetime [3]. TB is a leading cause of death in HIV patients with resulting mortality of about 15% to 40% or 1-2 in 5 cases [4].
Tuberculosis meningitis patients usually present with typical symptoms, including headache, neck stiffness, and fever, with onset weeks to months, before the onset, although typical meningeal signs may be absent initially. Some patients may present with very low GCS < 10, while other patients may have neurological features such as cranial nerve palsies, hemiparesis, paraparesis, and seizure [5,6].
Early diagnosis is crucial, and in case of highly suspicion of tuberculosis meningitis, the treatment need to be commenced on anti TB therapy immediately as the outcomes are significantly influenced by the stage of tuberculosis meningitis when treatment was commenced [7].
Case Presentation
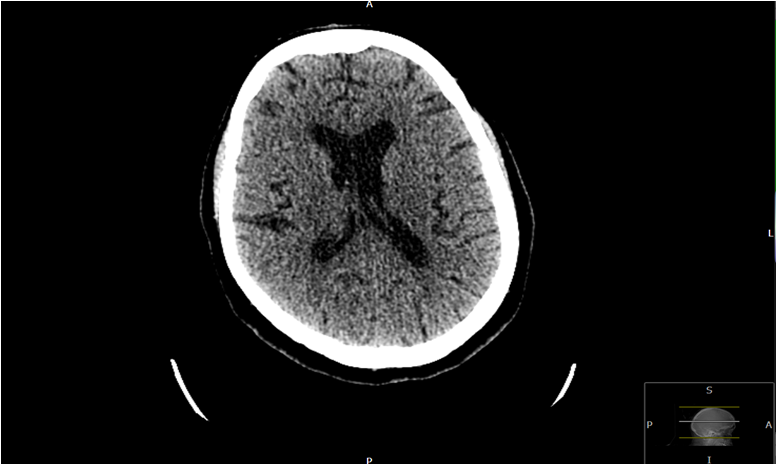
A 66-year-old patient of Asian origin who has been living in the US traveled to the UK to see her family. The patient was on Rituximab for Rheumatoid Arthritis and also has had type 2 diabetes, ischaemic heart disease, and hypothyroidism. She presented with confusion and behavioral changes for the last 10 days and on day 21 since arriving in the United Kingdom (UK). Physical examination was unremarkable besides a low GCS of 14/15. Additionally, the blood results were normal except slightly elevated CRP (C-reactive protein) 7, Creatinine 113, urea 9.4 and notably low Na level of 115 (Table 1). The CRP increased to 71 on day 5 of admission. A CT head on first day of presentation was normal, (Figure 1) but his lumbar puncture on day 2 showed Protein > 2.0, glucose 1.4, WCC 22.3 with 80% lymphocytes and 20% polymorphs (Table 2).
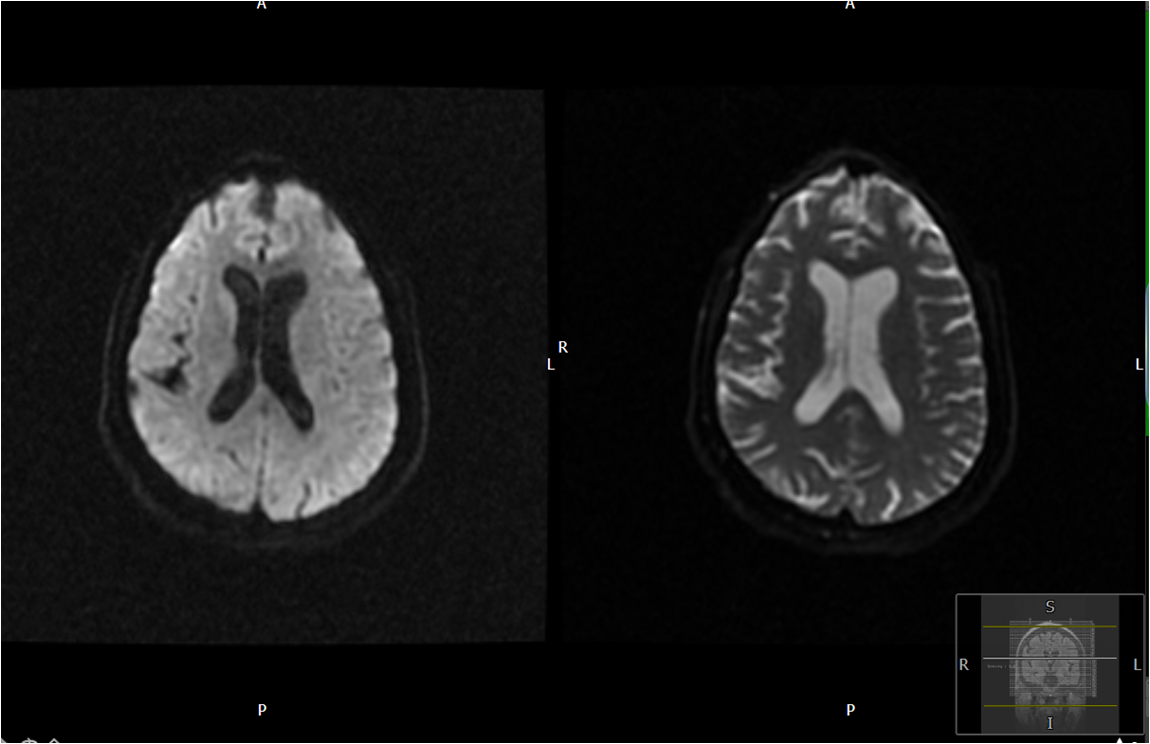
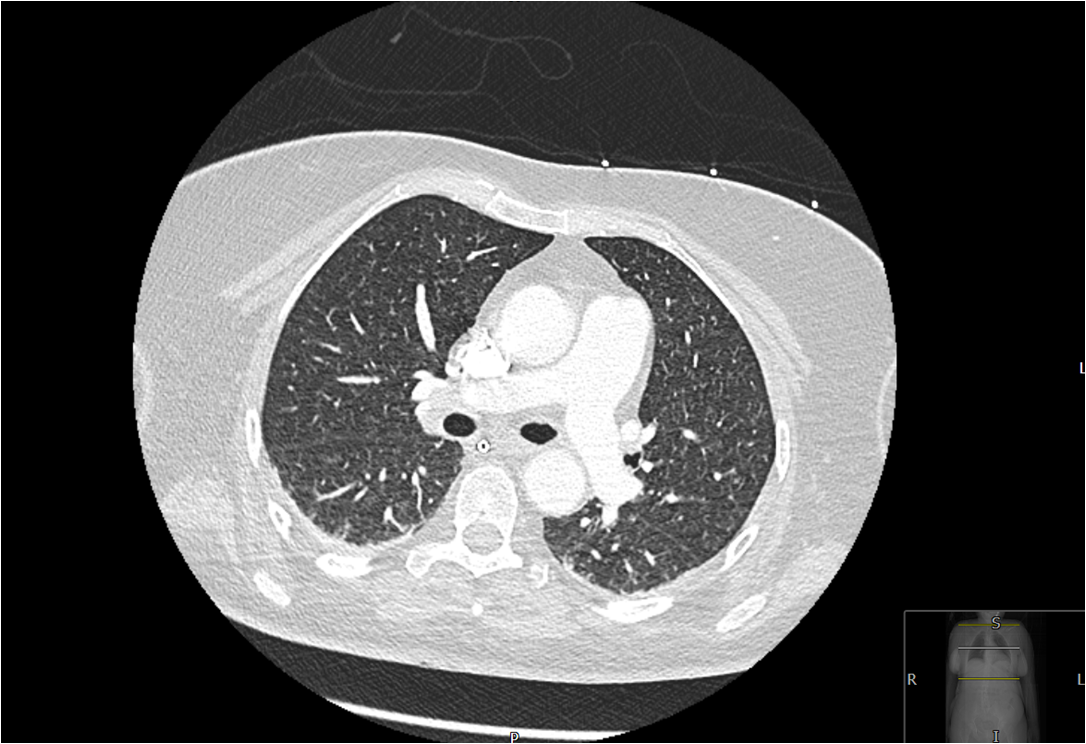
Consequently, he was started on IV antibiotics as per microbiology advice. An MRI (Magnetic resonance imaging) head on day 2 of admission showed a small vessels disease and mild brain atrophy (Figure 2). On 3rd day of his admission, he developed left-sided weakness, and a repeat CT head showed an ischaemic infarct of the right basal ganglia (Figure 3), and accordingly, he was transferred to ITU due to further deterioration of GCS. He was intubated and an NG tube was inserted. A CT thorax (Figure 4) on day 3 illustrated tree bud appearance in lungs consistent with bronchiolitis or TB and a CT venogram showed a small area of established infarct involving right periventricular coronal radiate. An echocardiogram on day 5 was unremarkable.
The sputum cultures revealed candida Albicans, however, the blood cultures were negative. As a result, he was commenced on the anti-tuberculosis therapy and Dexamethasone with regards to her high risk of Tb meningitis on day 4 and was also commenced on high dose aspirin for ischaemic infarct. Patient was given high doses of anti tuberculous therapy for pulmonary Tb in view of the CT findings and later on, the patient also had a positive sputum culture for mycobacterium tuberculosis. He also developed swallowing issues initially because of stroke and initially patient had NG feeding. Patient showed some early recovery and was discharged home and patient flew back to US after few weeks.
Differential Diagnosis
The first differential diagnosis in this case is tuberculosis meningitis and this was supported by the positive sputum culture and CSF findings. Additionally, the CT thorax also showed tree bud appearance and this patient was immunocompromised.
Another possible differential diagnosis in this case is viral meningitis and/or encephalitis however the CSF culture was negative for this patient.
The third possible differential diagnosis in this patient is Confusion secondary to hyponatraemia as this patient had low sodium of 115. Her symptoms however did not improve despite correction of her sodium level and patient had further complications.
Another possibility is malignancy that could also include intracranial malignancy however both CT scan of the chest and brain did not show any evidence of malignancy. Intracranial or lung malignancy can also cause hyponatraemia through syndrome of inappropriate antidiuretic hormone secretion (SIADH) however this was ruled out through imaging. Hyponatremia due to SIADH is seen in 40 to 50% of patients with TBM and the other common reason for low sodium in TBM is cerebral salt wasting.
Treatment
Initially, the Patient was treated for suspected bacterial meningitis/viral encephalitis with the antibiotics, including Ceftriaxone, Acyclovir and Amoxicillin as advised by microbiology. Despite the treatment, he had a sudden onset left sided weakness on day 3 and his GCS dropped to 9/15. A CT head revealed right basal ganglia infarct despite a normal CT head on admission and was started on Aspirin 300 mg OD accordingly. All blood cultures and sputum cultures were negative except two sputum samples which demonstrated candida albicans and mycobacterium tuberculosis respectively. He was also commenced on Dexamethasone 8 mg OD (once daily) on tapering dose along with Rifater (Rifampicin, Isoniazid, and Pyrazinamide) and Ethambutol on day 4. He was commenced early on anti tuberculous therapy in view of high risk along with dexamethasone. Patient had a 21 day course of anti- tuberculosis therapy at time of discharge and was advised to continue the treatment. His GCS improved to 15/15 and showed good physical recovery at the time of discharge although still required further rehabilitation.
In conclusion, this 66-year-old patient presented with low GCS and confusion, had significant hyponatraemia on admission with acute kidney injury and CSF samples were suggestive of tuberculosis meningitis and had a positive sputum culture after several negative cultures.
Outcome and Follow-Up
Unfortunately, it was not possible to follow up this patient due to his overseas residence, however, it was confirmed from family members and next of kin that patient was doing well and was getting better.
Discussion
The vast majority of TB meningitis cases are noted in Southeast Asia, Western pacific and African regions. The most common presenting features include headache, fever, neck stiffness, and the duration of symptoms onset can vary from days to months. TBM Patients usually present with low GCS in areas with poor resources and symptoms such as cranial nerve palsies, hemiparesis, paraparesis and seizures should raise the possibility of TBM in patients, whereas some patients present with multiple cranial nerve palsies with the most commonly involved cranial nerves being cranial nerves 3, 6 and 7 [8-10].
We were not able to find any reported cases of tuberculosis meningitis in patients on rituximab despite extensive search. There are few cases of Tb meningitis however, reported in patients on adalimumab and infliximab. Patient should have screening tests including screening for Tb prior to initiation of rituximab and according to the information available, our patient had screening test prior to commencement on rituximab although we cannot confirm this [11].
Vasculitis and stroke occur in 15 to 57% of patient with TBM depending on the modality of imaging. These patients are also at risk of hydrocephalus due to CSF outflow obstruction as a result of raised intracranial pressure. Use of glucocorticoids is recommended early in the disease onset and these patients are at high risk of strokes due to Vasculitis. Patient with tuberculous meningitis can also present with psychosis sometimes [12]. Youn Ho Kim, et al., 2007 reported a case of TBM in patient on infliximab for crohn disease however the article unfortunately is not accessible.
Another case report by Zumrut Sahbudak Bal, et al., 2017 of a 13 year old patient with idiopathic arthritis on methotrexate and steroids initially who was then commenced on adalimumab due to non-responsiveness to initial treatment. He presented with abdominal pain and became agitated on day 2 of admission. CSF samples showed high protein, glucose and lymphocyte count although both CSF and sputum samples were negative for Tb. This patient was admitted to ITU and was commenced on anti tuberculous therapy however did not survive. His sputum cultures initially were negative and another sample in week 6 was positive for mycobacterium tuberculosis that was responsive to anti-tuberculous therapy [13].
In conclusion, Tuberculosis meningitis is rare; however, it can present in high risk patients and in patients with immigrant background from certain regions and early initiation of treatment is of paramount importance in these patients as the disease can prove fatal.
Learning Points
➢ Tuberculous meningitis should be considered as a possible differential in any patient presenting with confusion and low GCS, particularly immunocompromised.
➢ Mortality is significantly high in tuberculosis meningitis with rates between 15% to 40% and very high in HIV positive patients
➢ Steroids and anti-tuberculosis therapy should be commenced early in these patients and leads to better outcome.
➢ Tuberculosis meningitis patients may present differently, and presentation varies from patients to patients and time of onset of symptoms may vary from days to weeks to months.
➢ Treatment should be continued for at least 7 to 10 months in tuberculosis meningitis and up to 18 months in presence of intracerebral tuberculoma.
Patient’s Perspective
I am so grateful to God for my mom's miracles recovery. My mom had received an excellent care in southend hospital when she fell ill during her visit to UK. The Southend Hospital staff kept us informed throughout her recovery process and provided her undivided attention along with support throughout her stay in ICU and then general ward. The only concerning issue I felt that could have been addressed in a better was her initial visit to the ER with the symptoms of vomiting and unconsciousness, where the amount of time it took to establish her diagnosis could be shorten, if only the procedures expedited because off her age and history of health. Nevertheless, I am also very thankful to doctors especially Dr. Zahid Khan and many others in ICU including the nursing staff for their support.
Intellectual Property Rights Assignment or Licence Statement
I, Dr Zahid Ullah Khan, the Author has the right to grant and does grant on behalf of all authors, an exclusive licence and/or a non-exclusive licence for contributions from authors who are: i) UK Crown employees; ii) where BMJ has agreed a CC-BY licence shall apply, and/or iii) In accordance with the relevant stated licence terms for US Federal Government Employees acting in the course of the their employment, on a worldwide basis to the BMJ Publishing Group Ltd ("BMJ") and its licensees, to permit this Work (as defined in the below licence), if accepted, to be published in BMJ Case Reports and any other BMJ products and to exploit all rights, as set out in our licence author licence.
References
- World Health Organization (2019) Global tuberculosis report.
- Zumla A, Raviglione M, Hafner R, et al. (2013) Current concepts: Tuberculosis. N Engl J Med 368: 745-755.
- Komolafe MA, Sunmonu TA, Esan OA (2008) Tuberculous meningitis presenting with unusual clinical features in Nigerians: Two case reports. Cases J 1: 180.
- Kennedy D (1979) Tuberculous Meningitis. JAMA 241: 264.
- Vinnard C, King L, Munsiff S, et al. (2016) Long-term mortality of patients with tuberculous meningitis in New York City: A cohort study. Clin Infect Dis 64: 401-407.
- Thwaites G, Bang N, Dung N, et al. (2004) Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults. N Engl J Med 351: 1741-1751.
- Schoeman J, Van Zyl L, Laubscher J, et al. (1997) Effect of corticosteroids on intracranial pressure, computed tomographic findings, and clinical outcome in young children with tuberculous meningitis. Pediatrics 99: 226-231.
- Girgis N, Farid Z, Kilpatrick M, et al. (1991) Dexamethasone adjunctive treatment for tuberculous meningitis. Pediatr Infect Dis J 10: 179-182.
- Prasad K, Singh M, Ryan H (2016) Corticosteroids for managing tuberculous meningitis. Cochrane Database of Systematic Reviews.
- Shankar S, Mangalore S, Desai S, et al. (2014) Cerebral tubercular thrombophlebitis presenting as venous infarct: Magnetic resonance imaging and pathologic correlation. Ann Indian Acad Neurol 17: 130-134.
- Lewinsohn D, Leonard M, LoBue P, et al. (2017) Official American thoracic society/infectious diseases society of America/centers for disease control and prevention clinical practice guidelines: Diagnosis of tuberculosis in adults and children. Clinical Infectious Diseases 64: 111-115.
- Márquez C, Laria L, Arias F, et al. (2011) Residual hydrocephalus after tuberculous meningitis in a patient with biological therapy. Inflamm Bowel Dis 17: E33-E34.
- Bal Z, Yazici P, Sen S, et al. (2017) A fatal case of tuberculous meningitis in a child with juvenile idiopathic arthritis: A diagnostic challenge. Rev Soc Bras Med Trop 50: 709-711.
Corresponding Author
Dr. Zahid Khan, Southend University Hospital NHS Trust, UK
Copyright
© 2022 Khan Z. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.