Sterile Water Test Can Shows Signs of Fertilisation and Further Growth of Embryo- A Case Report
Introduction
Structural integrity and function of the plasma membrane of the cell defines the viability of spermatozoa. HOS (Hypo-Osmotic Swelling) test is considered as Benchmark test for checking the vitality of spermatozoa. The constituents of HOS test are 0.735g of sodium citrate dihydrate and 1.351g of D-fructose in 100 ml of purified water has an osmolarity of 150 mOsm. The basic principle of HOS test is spermatozoa when subjected to HOS solution, Sperm tails expand and coils based on plasma membrane integrity. Coiled tails are considered as vital spermatozoa. Spermatozoa which do not show any coiling due to loss of plasma membrane integrity are considered as dead spermatozoa [1,2].
Sterile water test is a novel test for checking the vitality of spermatozoa [2]. HOS test and sterile water test works on the analogous basic principle. Sterile water is easily available, cost-effective, and inexpensive. A Study conducted by the Author revealed mean average of live spermatozoa of HOS test, sterile water test, and Eosin nigrosin test (EN) test are 55.83%, 58.10%, and 59% respectively [2]. p = 0.567 of all three tests is statistically insignificant thereby indicating that all tests have similar outcome [2]. The above study has revealed that Sterile water works as a vitality test for diagnostic purposes to check the vitality of spermatozoa. However, the therapeutic value of sterile water test is yet to be proved i.e. Spermatozoa subjected to sterile water test can fertilize the oocyte. Till now, there is no study reported yet that Spermatozoa subjected to sterile water test can fertilize the oocyte.
Materials and Methods
A couple has visited our clinic with primary infertility. The female patient’s age was 30-years-old and the male patient's age is 42-years-old and semen analysis was done. Semen analysis revealed Occasional immotile spermatozoa. Spermatozoa were subjected to sperm Mobil (GM 501 spermMobil) and checked for motility [3]. No motility was seen when checked under the microscope thoroughly. Testicular sperm extraction (TESE) was done for the patient and checked for motile spermatozoa. However, we couldn't see any motile spermatozoa when checked under a microscope thoroughly. Lack of motility has made us go for vitality tests (HOS test and sterile water test). Spermatozoa were subjected to HOS test and sterile water test for checking vitality of spermatozoa and could see some spermatozoa which have coiled tails and selected for ICSI (Intra Cytoplasmic Sperm Injection).
Ovarian stimulation was done with the Antagonist protocol. Ovum pickup (OPU) was done 34 hrs after HCG trigger. 9 oocytes with cumulus complex were obtained after egg retrieval. All 9 oocytes have poor oocyte quality with peri-vitelline debris. Denudation was done 2 hrs after egg retrieval. 9 mature oocytes were collected and incubated in a single-step medium (origio). The male patient collected semen by ejaculation and washed with sperm wash medium at 1500 rpm for 7 minutes. Supernatant was removed and sperm with pellet was incubated at 37 °C. Sperm pellet was divided into two halves and subjected into HOS test and sterile water test.
HOS test protocol: Sperm pellet was suspended into 100 ul of HOS test at 37 °C for 10 minutes. Coiled tails are considered viable spermatozoa and straight tails are considered dead spermatozoa. Coiled tail spermatozoa are selected and washed in a sperm wash medium and subjected to ICSI.
Sterile water test protocol: Sperm pellet was suspended into 100 ul of sterile water test at 37 °C for 10 minutes. Coiled tails are considered vital spermatozoa and uncoiled tails are considered dead spermatozoa. Coiled tail spermatozoa are selected and washed in a sperm wash medium and subjected to ICSI. Ethical clearance for the study was taken from the Institutional Ethics Committee (ECR/1301/Inst/TG/2019) and informed consent has been taken from the couple.
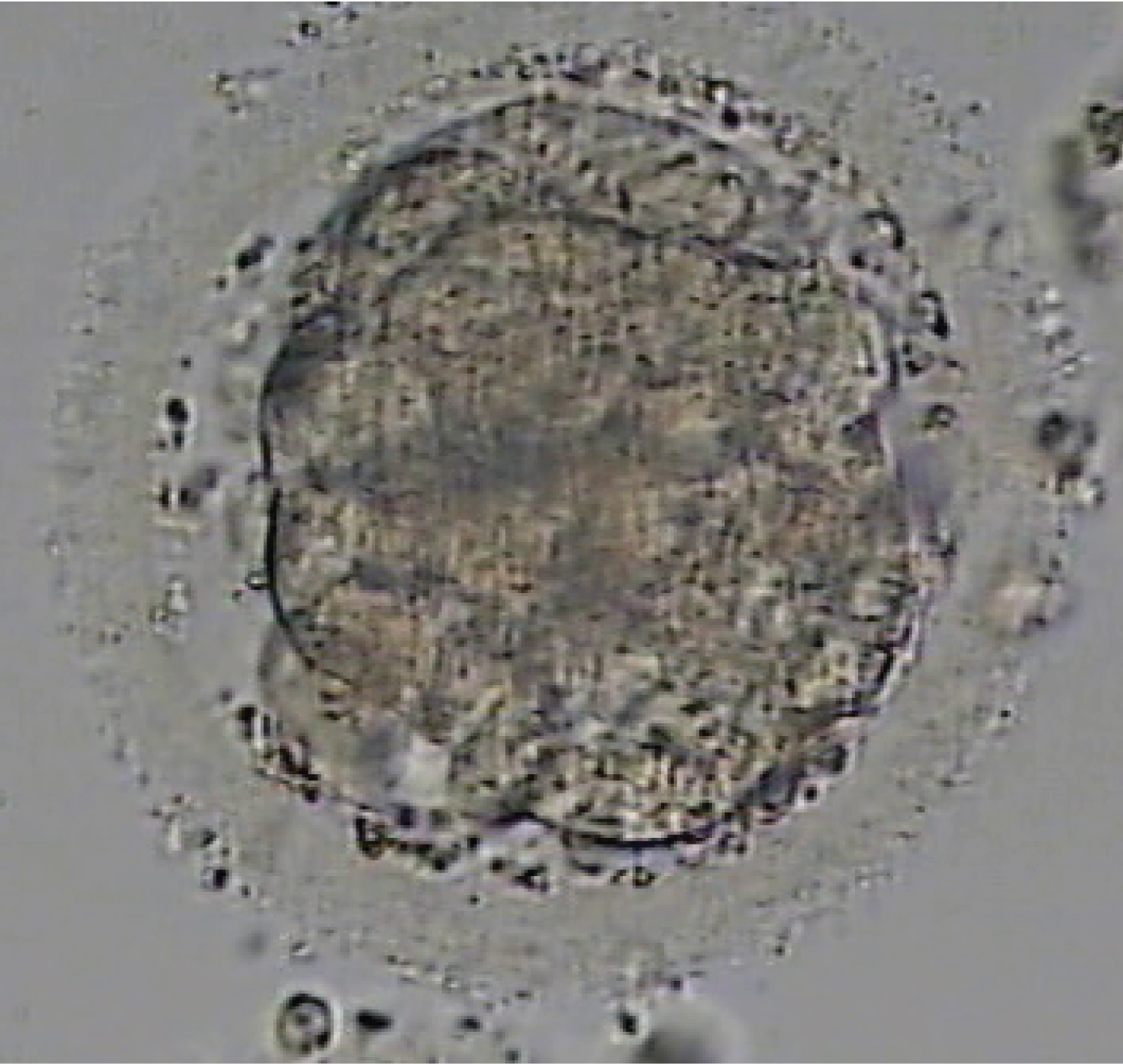
5 oocytes were injected with vital spermatozoa obtained through HOS test and 4 oocytes were injected with spermatozoa selected with sterile water test. The fertilization check was done 17-19 hours after ICSI. One oocyte has 2PN, One oocyte has 1PN, and the other 2 oocytes are unfertilized in oocytes injected with sterile water test protocol whereas Oocytes injected with HOS test protocol have two 1PN oocytes and the other 3 oocytes didn’t show any sign of fertilization. 2PN zygote which is Obtained by sterile water test injected spermatozoa has further cleaved into 5 cell stage on Day 2 and reached the compaction stage on Day 4. 1PN zygotes from both the groups have been arrested. Vitrification of embryo was done on day 4 at compacting stage (Figure 1, Figure 2, Figure 3 and Figure 4).
Discussion
Selection of vital spermatozoa is a big challenge in cases reported with complete immotile spermatozoa. Sperm Mobil might help in some of the cases and Testicular sperm extraction (TESE) will rarely give motile spermatozoa in cases of absence of motile spermatozoa but in our case both of them couldn’t help us to select motile spermatozoa [3]. LASER has been used for selection of immotile vital spermatozoa in some cases but it is very expensive as many IVF centers couldn’t afford it [4]. HOS test has been considered as standard test for selection of vital spermatozoa and can be used for ICSI but it is quite expensive and not available as soon as you need it. Sterile water test is easily available, cost-effective and easy to use. This is the first study reported where vital spermatozoa selected from sterile water test has shown signs of 2PN fertilization and reached morula stage on Day 4.
Declaration
Authors declare no conflict of interest.
References
- Jeyendran RS, Van der Ven HH, Perez-Pelaez M, et al. (1984) Development of an assay to assess the functional integrity of the human sperm membrane and its relationship to other semen characteristics. J Reprod Fertil 70: 219-228.
- Shiva Krishna G, Pandiyan N (2015) A New Simple test for checking vitality of spermatozoa. Chettinad Health City Medical Journal 4: 24-27.
- Sandi-Monroyetal NL, Musanovic S, Zhu D, et al. (2019) Use of dimethylxanthine theophylline (SpermMobil®) does not affect clinical, obstetric or perinatal outcomes. Arch Gynecol Obstet 300: 1435-1443.
- Aktan TM, Montag M, Duman S, et al. (2004) Use of a laser to detect viable but immotile spermatozoa. Andrologia 36: 366-369.
Corresponding Author
G. Shiva Krishna, Junior Embryologist, Gunasheela Maternity and Surgical Hospital, Bangalore, India.
Copyright
© 2024 Krishna GS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.