Left Atrial Appendage Thrombus Resolution with Clopidogrel after Apixaban Failure: A Case Series
Abstract
This hypothesis-generating, case series reviews the evidence available for managing left atrial appendage thrombus in patients already on therapeutic anticoagulation with apixaban. Our six patient cases highlight the first documented evidence of complete, accelerated clot resolution upon the addition of P2Y12 inhibitor, clopidogrel, to current therapeutic doses of apixaban.
Keywords
Clopidogrel, apixaban, LAA thrombus
Abbreviations
LAA: Left atrial appendage; LAAT: Left atrial appendage thrombus; DOAC: Direct oral anticoagulant; TEE: Transesophageal echocardiography; ASCVD: Atherosclerotic cardiovascular disease; TAVR: Transcatheter aortic valve replacement; CVA: Cerebrovascular accident; Scr: Serum creatinine
Introduction
Nonvalvular atrial fibrillation increases the risk of atrial thrombi formation, particularly in the left atrial appendage (LAA), which predisposespatients toischemic stroke [1-3]. Oral anticoagulation, with a vitamin K antagonist (VKA) or direct oral anticoagulant (DOAC), is effective at decreasing ischemic stroke and systemic embolism, however treatment of a LAA thrombus shows resolution rates ranging from 50-90% despite therapeutic anticoagulation [4-10]. Strategies to treat a LAA thrombus while on therapeutic anticoagulation are limited. Case reports are documented showing LAA thrombi present in patients on warfarin with subtherapeutic INRs that subsequently resolve upon improving the time in therapeutic range or switching to a DOAC [11-13]. DOACs, which are being used more widespread for stroke prevention in atrial fibrillation, are documented to be as effective as warfarin in resolving LAA thrombi [9,10,14,15]. However, there is limited evidence describing how to treat LAA thrombi in the setting of therapeutic DOAC therapy. Limited reports suggest effective options include switching the patient to another DOAC or warfarin, or increasing an inappropriately low DOAC dose [11,16,17]. Nevertheless, resolution takes time, up to 13-16 weeks, and several thrombi remain unresolved [10,18].
To our knowledge, this is the first documented case series of complete, accelerated LAA thrombi resolution with the addition of P2Y12 inhibitor therapy in patients on therapeutic doses of a DOAC, specifically, apixaban.
Case 1
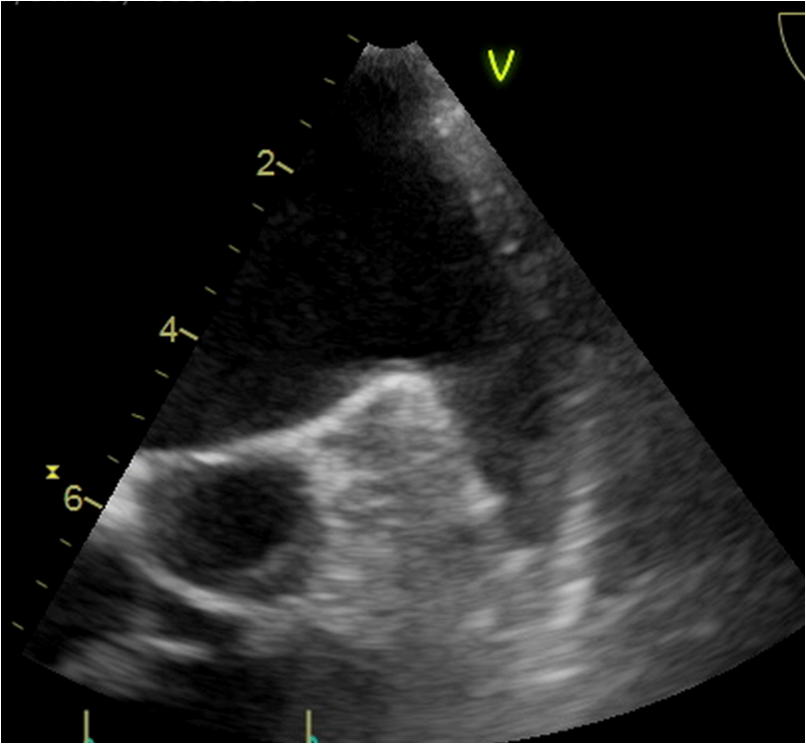
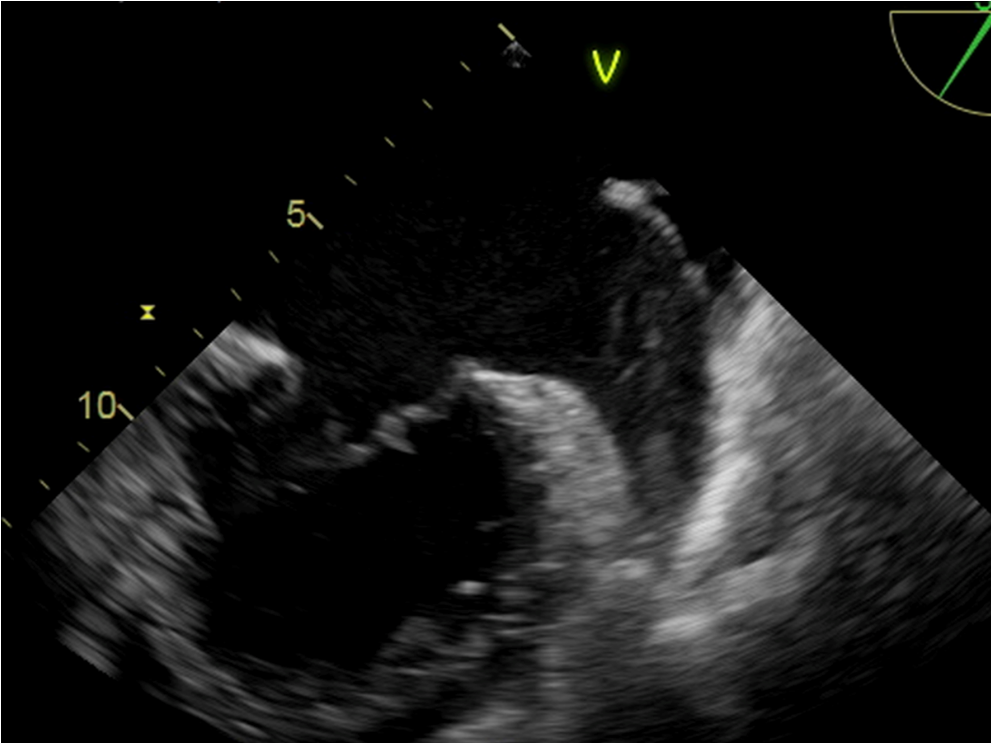
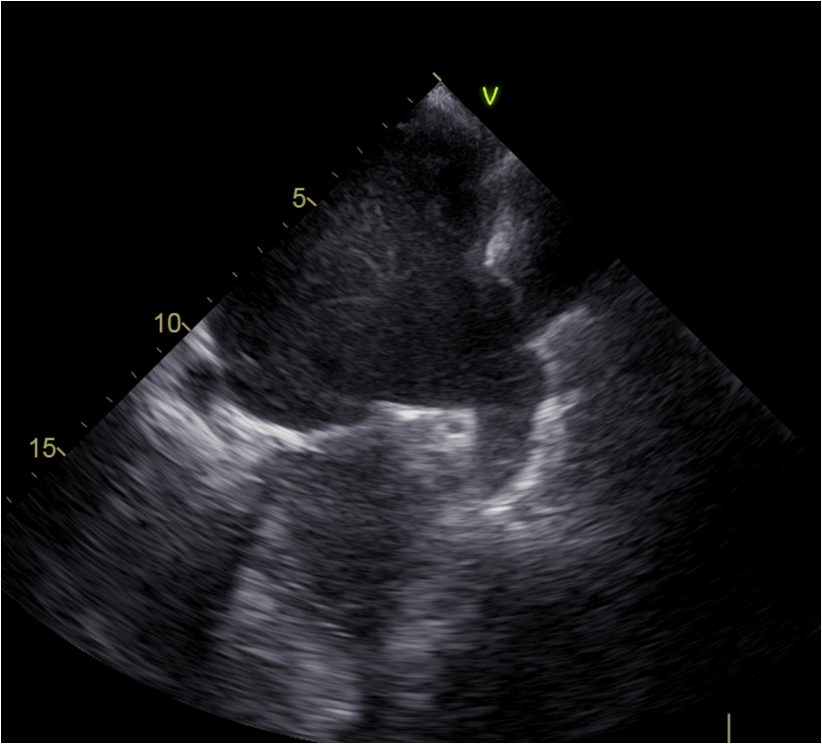
An 89-year-old male, 81.9 kg with persistent atrial fibrillation (CHA2DS2VASc score 4), heart failure with preserved ejection fraction, severe aortic stenosis, ASCVD, hypertension and hyperlipidemia presented to the hospital for a transfemoral transcatheter aortic valve replacement (TAVR). Echocardiography showed the patient had a LAA thrombus despite adherence to warfarin therapy. Patient's INR two weeks prior was reported as subtherapeutic at 1.8. After his TAVR, prior to discharge, he was switched to apixaban 2.5 mg twice daily, dosed accordingly based on his age, weight and serum creatinine (Scr) of 2.3 mg/dL. He was also discharged on aspirin 81 mg, lisinopril, furosemide, lovastatin, fenofibrate, amlodipine, tamsulosin, omeprazole, and finasteride. The patient presented 6 weeks post-TAVR for a TEE for evaluation of a Watchman device. TEE showed the presence of a LAA thrombus, despite being adherent to apixaban therapy for 41 days. The patient was started on clopidogrel 75 mg daily, in addition to apixaban. A follow up TEE 15 days after clopidogrel initiation revealed the resolution of the LAA thrombus.
Case 2
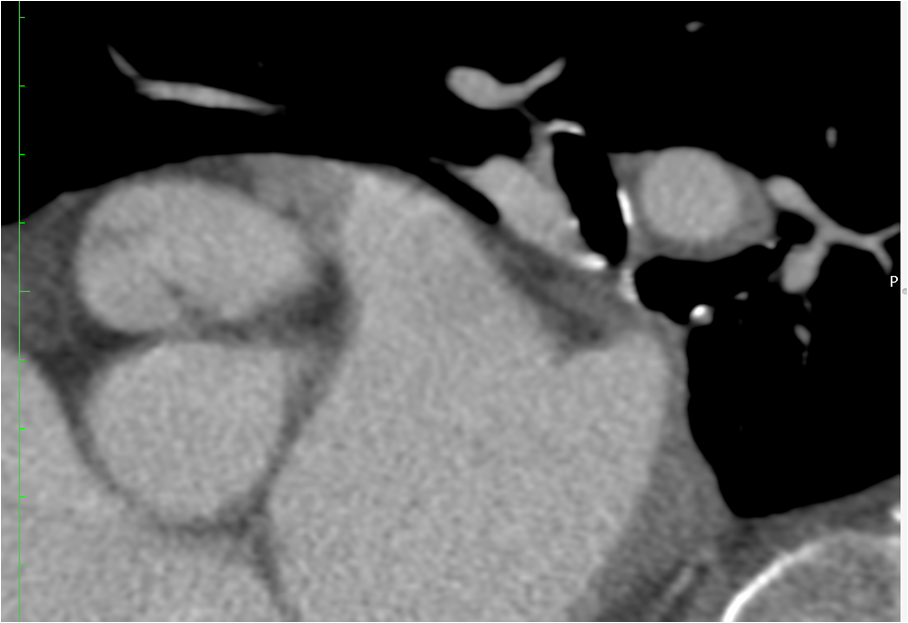
An 88-year-old male, 97.2 kg, with persistent atrial fibrillation (CHA2DS2VASc 5), hypertension, hyperlipidemia, ASCVD and history of stroke presented for evaluation of a Watchman device. A CT with contrast showed a LAA thrombus, subsequently confirmed by TEE, despite being on warfarin therapy. INR was subtherapeutic at 1.8, although the patient reported that his INR is typically between 2 and 2.5. With the discovery of the LAA thrombus, the patient was transitioned to apixaban 5 mg twice daily, dosed appropriately based on his age, weight and Scr of 1.33 mg/dL. In addition, he was on carvedilol, furosemide, hydralazine, KCl, atorvastatin, carbamazepine and levothyroxine. The patient was adherent to the apixaban 5 mg twice daily regimen and presented 10 days later for a TEE. The LAA clot was still present, therefore, clopidogrel 75 mg po daily was added to the regimen in efforts to dissolve the LAA thrombus. A follow up TEE 21 days after clopidogrel initiation revealed complete resolution of the thrombus.
Case 3
An 89-year-old male, 81.8 kg, with persistent atrial fibrillation (CHA2DS2VASc 5), heart failure with preserved ejection fraction, significant lung disease requiring home oxygen, hypertension, history of transient cerebral ischemic attack, bradycardia with pacemaker placement and chronic kidney disease presented for evaluation of a Watchman device. CT scan showed a LAA thrombus, which was later confirmed by TEE, despite apixaban therapy. The patient had been taking apixaban 2.5 mg po twice daily for 4 years, which was appropriate based on his age, weight and Scr of 2.0 mg/dL. Additional medications included furosemide, sacubitril/valsartan, metoprolol succinate, atorvastatin, tramadol, omeprazole, duloxetine and ropinirole. When the LAA thrombus was seen on CT, the apixaban dose was increased to 5 mg twice daily. One week later, the LAA thrombus was still present and unchanged on repeat TEE and therefore the patient was started on aspirin 81 mg and clopidogrel 75 mg daily in addition to the apixaban 5 mg twice daily. A follow up TEE 17 days later revealed resolution of the thrombus.
Case 4
An 84-year-old female, 64.5 kg, with paroxysmal atrial fibrillation (CHA2DS2VASc 4), hypertension and pulmonary hypertension presented for evaluation of a Watchman device. She reported adherence to apixaban 2.5 mg twice daily for two years, which was a subtherapeutic dose given her age, weight and Scr of 1.1 mg/dL. She was also on pravastatin, bumetanide, lisinopril, metoprolol succinate, oxybutynin, quetiapine, and levothyroxine. On presentation to the office, CT scan showed a LAA thrombus. The patient was started on clopidogrel 75 mg daily in addition to apixaban. Follow up TEE 32 days later revealed complete resolution of the LAA thrombus.
Case 5
A 68-year-old male, 75 kg, with persistent atrial fibrillation (CHA2DS2VASc 5), history of CVA, hypertension, hyperlipidemia, heart failure with preserved ejection fraction, ASCVD, and tricuspid valve regurgitation presented for evaluation for a Watchman device. The patient was anticoagulated with apixaban 5 mg twice daily for two years, which was appropriate based on his age, weight and Scr of 0.81 mg/dL. He was also on atenolol, atorvastatin, esomeprazole, allopurinol, gabapentin, dutasteride, alfuzosin and milk thistle. A CT scan showed a potential LAA thrombus which was subsequently confirmed by TEE. At that point, clopidogrel 75 mg daily was added to the patient's medication regimen. A TEE 25 days later showed resolution of the LAA thrombus.
Case 6
A 72-year-old male, 105 kg, with permanent atrial fibrillation (CHA2DS2VASc 4), nonrheumatic mitral valve insufficiency with mitral tissue valve replacement, cardiomyopathy, hypertension, hyperlipidemia, ASCVD and pacemaker placement presented for evaluation of a Watchman device. The patient was switched from warfarin to apixaban 5 mg twice daily 9 months prior, which was an appropriate dose based on his age, weight and Scr 1.49 mg/dL. In addition to apixaban, he was also on aspirin 81 mg, bumetanide, clonidine, lisinopril, metoprolol succinate, pravastatin, finasteride, tamsulosin, sertraline, famotidine and ferrous sulfate. A CT showed LAA thrombus which was confirmed with a TEE. The patient stopped the aspirin and started clopidogrel 75 mg daily in addition to apixaban. A repeat TEE 18 days later revealed resolution of LAA thrombus.
Discussion
The presence of LAA thrombi in patients with atrial fibrillation is concerning as this is where over 90% of cardiac emboli originate in nonvalvular atrial fibrillation [1-3]. Treatment for the resolution of LAA thrombi is imperative in reducing the risk of ischemic stroke. Studies have observed 10-30% of atrial fibrillation patients not on anticoagulation have LAA thrombi present by TEE [19-23]. Oral anticoagulation with either warfarin or a DOAC is considered standard of care for ischemic stroke prevention in atrial fibrillation, however LAA thrombus may still exist despite therapeutic anticoagulation. In addition, when identified, LAA thrombus resolution rates range from 50-90% despite therapeutic anticoagulation with warfarin [4-6]. Studies of patients with atrial fibrillation detected LAA thrombi by TEE in 7-9% despite being on therapeutic warfarin with an INR 2-3 [13,24]. Those rates of LAA thrombi further increase, in fact almost double, when patients have subtherapeutic INRs of < 2.0.(13,25)
DOAC therapy for LAA thrombi resolution has been supported by several case reports in the past couple of years [12,25-27]. Scarano M, et al. and Li Y, et al. both describe case reports of rivaroxaban utilized for resolution of LAA thrombus, showing complete resolution by 3 months and 5 weeks, respectively, after transitioning therapy to rivaroxaban [12,28]. In 2016, the X-TRA trial was the first prospective, multicenter study looking at the efficacy of rivaroxaban in resolving LAA thrombi in warfarin naïve or subtherapeutic warfarin patients [9]. The study looked at the resolution of LAA thrombi on TEE in patients after rivaroxaban therapy. From the 53 patients with LAA thrombi on initial TEE, 95% were Eastern European and the median CHA2DS2VASc score was 4. 81.7% of patients received the 20 mg dose and 18.3% received the 15 mg dose based on renal function. Adherence was accounted for and shown to be 100%. After 6-8 weeks of rivaroxaban therapy, follow up TEE showed thrombus resolution was 41.5% (95% CI 28.1%-55.9%) and the rate of resolved or reduced thrombus was 60.4% (95% CI 46.0% - 73.6%). Thrombus resolution tended to be observed in older patients and those with a lower CHA2DS2VASc. The retrospective, observational registry, CLOT-AF, indicated resolution rates in patients on rivaroxaban to be 62.5% [9]. This number suggests that a proportion of patients will have thrombus resolution or reduction with factor Xa inhibitor, rivaroxaban. Yet as documented with warfarin, a significant number of patients will not have thrombus resolution despite being adherent to DOAC therapy. In fact, studies are indicating that the DOAC resolution rates are similar to those seen with warfarin. A real world observational study reported a 60% LAA thrombus resolution rate in atrial fibrillation patients who were deemed to be appropriately anticoagulated [10]. Authors found no difference in the type of oral anticoagulant that was selected. Additionally, a recent retrospective study of 388 atrial fibrillation patients found that after 4 weeks of DOAC therapy, there was no difference in the prevalence of LAA thrombi between DOAC and warfarin therapy (4.4% vs. 2.9%, p = 0.45) [15]. This was similar to findings from another trial assessing the prevalence of LAA thrombi in 559 Japanese patients with nonvalvular atrial fibrillation, which found no difference in LAA thrombi present on TEE after 3 weeks of therapy with a DOAC or warfarin (2.6% vs. 2.8%, p = 0.86) [14].
In this report, we describe 6 cases of patients with LAA thrombi despite oral therapeutic anticoagulation with factor Xa inhibitor, apixaban. Several case reports document successful LAA thrombus resolution in 2-8 weeks after initiating apixaban therapy [7,26,27]. However, all of our patients had LAA thrombus found by TEE or CT after adherence to apixaban. A multivariate analysis showed that an elevated BNP ≥ 173 pg/mL was the only independent predictor of LAA thrombi.(!4) Other predictors of LAA thrombi described in the literature includes a higher CHA2DS2VASc score, decreased left atrial volume changes and the presence of spontaneous echocardiographic contrast. (!3) Previous studies suggest that a larger left atrial dimension, lower LVEF and LV hypertrophy are also associated with the formation of LAA thrombi [29,30]. All six of our patients had elevated CHA2DS2VASc scores of 4 or 5, perhaps predisposing these patients to a higher risk of developing a LAA thrombus, despite therapeutic anticoagulation.
In determining reasons for apixaban failure in preventing LAA thrombus in our 6 patients, we would be remiss if we did not consider the medication dose, medication adherence and medication interactions.
Three of our six patients were on apixaban 2.5 mg twice daily, whereas three patients were on the 5 mg twice daily dose. All doses were appropriate based on FDA approved package labelling, with the exception of one patient (case #5) that was put on the lower dose despite not meeting the 2 out of 3 criteria. Evidence has demonstrated that empirically reducing the dose of apixaban without meeting the labelled criteria leads to a significant increased risk of stroke [31]. In this one case, it does raise the question of overall efficacy and safety with the use of a reduced dose of apixaban that was not clinically studied.
Medication adherence is a huge determinant of efficacy, particularly since the DOAC half-lives are much shorter than warfarin. One in five patients in the stroke prevention in nonvalvular atrial fibrillation randomized controlled trials discontinued the DOAC therapy during follow up, leaving them unprotected from events [32]. Recent real-world registries demonstrate that nearly 40% of patients at risk of ischemic stroke do not receive any oral anticoagulation due to contraindications, bleeding or patient/provider preferences [32,33]. In this case series, all 6 of our patients reported adherence to the medications and refill schedules confirmed this.
Medication interactions can affect the serum drug concentration of the DOACs. In particular, with factor Xa inhibitors, such as apixaban, stimulation or inhibition of P-glycoprotein or CYP3A4 enzymes, can increase or decrease apixaban plasma levels. Apixaban plasma levels may be reduced by up to 50% when given in combination with strong P-gp or CYP3A4 inducers, such as carbamazepine, phenytoin, rifampin or St. John's wort. Patient case #2 was on concomitant carbamazepine therapy, which may have resulted in a subtherapeutic concentration of apixaban, potentially leading to inefficacy in preventing LAA thrombus. However, none of the other patients had medication interactions present that would result in a subtherapeutic serum apixaban concentration. Apixaban drug levels to confirm were not received based on limited availability. Only 2 of the 6 patients were on concomitant low dose aspirin therapy at baseline.
In evaluating our case series, we also wanted to ensure that our patients were receiving therapeutic anticoagulation with apixaban for an adequate amount of time before determining that it was not effective in preventing the LAA thrombus. Typically, the resolution of LAA thrombi is expected to occur within 3 to 4 weeks of therapeutic anticoagulation therapy, as current guidelines recommend VKA therapy or DOAC for 3 weeks upon detection of a LAA thrombus in atrial fibrillation patients [34]. Many of the studies discussed here re-image patients for LAA thrombi after 3 to 4 weeks of anticoagulation. A study by Collins et al. showed 89% resolution of LAA thrombi in 18 patients with atrial fibrillation after 4 weeks of warfarin therapy [4]. One case report described a patient with atrial fibrillation and a large LAA thrombus on TEE who was started on rivaroxaban 20 mg daily and showed relevantly decreased thrombus size at 3 weeks and complete resolution after 5 weeks of rivaroxaban therapy [28]. In addition, other reports note the resolution of LAA thrombi prior to 3 to 4 weeks of therapy. A case report by Kawakami et al. demonstrated resolution after only 16 days of apixaban therapy [26]. In our series, patient case 1 was on apixaban therapy for about 6 weeks (41 days), patient case 6 for 9 months and patient cases 3, 4 and 5 were on apixaban for several years, which suggests adequate time for thrombi resolution. However, patient case 2, was on apixaban therapy for just 10 days prior to repeat TEE, which showed that the LAA thrombus remained present. It is unknown if a longer duration of therapy would have resulted in thrombus resolution, however, in this case it was not clinically feasible to wait for an extended period of time.
Understanding that LAA thrombi still exists despite adequate oral anticoagulation, the question remains on how to optimally treat patients with a LAA thrombi despite being adherent to an oral anticoagulant regimen, particularly a DOAC. We describe here 6 patient cases of LAA thrombi present despite oral anticoagulation with factor Xa inhibitor, apixaban, that resolved within 2 to 4 weeks after adding a P2Y12 inhibitor, clopidogrel, to the regimen. To our knowledge, this is the first report to demonstrate efficacy of this anticoagulant- antiplatelet combination in resolving a LAA thrombi observed while a patient was therapeutically anticoagulated with a direct oral anticoagulant. Documented strategies to treat LAA thrombi described from a real world study, included increasing the DOAC dose from an inappropriately low dose, maintaining the same DOAC and dose, or switching to warfarin [11]. Another option is to change the DOAC agent to one of an opposite mechanism. In a case report described by Koyama, et al., a 78-year-old male with atrial fibrillation, CHA2DS2VASc 3, was on dabigatran 110 mg po BID for stroke prevention [17]. The patient suffered a cerebral infarction and a TEE showed a large LAA thrombus. The patient was switched from dabigatran to apixaban 5 mg twice daily. Follow up TEE on day 7, showed no change in the size of LAA thrombus. On day 24, a reduction in thrombus size was shown on TEE and on day 56 of apixaban therapy, TEE showed complete resolution. A report by Watanabe, et al. described 2 cases in Japan that demonstrated the efficacy of dabigatran in resolving pre-existing LAA thrombi refractory to rivaroxaban [16]. Two patients, both on rivaroxaban for more than 2 years, were switched to dabigatran therapy after TEE discovered LAA thrombi. Resolution of the LAA thrombi was observed by TEE after 6 weeks in one patient and after 12 months for the second patient. The author supports the direct thrombin inhibitor, dabigatran, use for LAA thrombi as it not only inhibits both clot bound thrombin and soluble thrombin, but it also reduces thrombin-mediated activation of platelets. Its antiplatelet effects may also be associated with the authors findings that dabigatran is more effective in reduction of left atrial spontaneous echo contrast than warfarin. Perhaps targeting antiplatelet activity in LAA thrombi is a reasonable approach in those patients that fail anticoagulant therapy.
In this case series, we added antiplatelet effects to the factor Xa inhibitor using P2Y12 inhibitor, clopidogrel. To our knowledge, this is the first study that demonstrates effective LAA thrombus resolution with the addition of a P2Y12 inhibitor (Table 1). There is no published evidence of clopidogrel exhibiting a role in clot resolution. A study by Reiner et al. examined the use of direct P2Y12 inhibitor ticagrelor in reducing the expression and activity of tissue factor and plasminogen activator inhibitor-a (PAI-1), which may lead to the a lower level of thrombogenicity in the left atrial appendage [35]. The data found that ticagrelor, but not the active metabolite of clopidogrel, did in fact reduce the expression and activity of tumor necrosis factor-alpha (TNF-alpha) and PAI-1 in endocardial cells, suggesting a possible local antithrombotic effect of ticagrelor at a cellular level.
Conclusion
The presence of LAA thrombi in patients with nonvalvular atrial fibrillation may predispose patients to ischemic stroke, therefore resolution is imperative. DOACs appear to be an option to resolve LAA thrombi, however, often many LAA thrombi go unresolved despite appropriate anticoagulation. There are no clear guidelines on how to treat a patient on a therapeutic DOAC that has the presence of a LAA thrombus. This report describes 6 patients that presented with LAA thrombus while on therapeutic anticoagulation with apixaban. We provide evidence that the addition of clopidogrel to the apixaban regimen led to quick thrombus resolution. Although further studies are needed, this evidence provides a new potential treatment option when a LAA thrombus is discovered despite adherence to DOAC therapy.
Learning Objectives
Describe the incidence and management of patients with LAA thrombi despite anticoagulation.
To examine P2Y12 inhibitors as potential treatment options for patients with LAA thrombi despite anticoagulation with a DOAC.
Funding
NA.
Conflict of Interest Disclosure
None for authors.
References
- Blackshear JL, Odell JA (1996) Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg 61: 755-759.
- Mahajan R, Brooks AG, Sullivan T, et al. (2012) Importance of the underlying substrate in determining thrombus location in atrial fibrillation: Implications for left atrial appendage closure. Heart 98: 1120-1126.
- Scherr D, Dalal D, Chilukuri K, et al. (2009) Incidence and predictors of left atrial thrombus prior to catheter ablation of atrial fibrillation. J Cardiovas Electrophysiol 20: 379-384.
- Collins LJ, Silverman DI, Douglas PS, et al. (1995) Cardioversion of nonrheumatic atrial fibrillation: Reduced thromboembolic complications with 4 weeks of precardioversion anticoagulation are related to atrial thrombus resolution. Circulation 92: 160-163.
- Corrado G, Tadeo G, Beretta S, et al. (1999) Atrial thrombi resolution after prolonged anticoagulation in patients with atrial fibrillation: A transesophageal echocardiographic study. Chest 115: 140-143.
- Jaber WA, Prior DL, Thamilarasan M, et al. (2000) Efficacy of anticoagulation in resolving left atrial and left atrial appendage thrombi: A transesophageal echocardiographic study. Am Heart J 140: 150-156.
- Yaghi S, Chang D, Hung P, et al. (2018) Left atrial appendage morphology and embolic stroke of undetermined source: A cross-sectional multicenter pilot study. J Stroke Cerebrovasc Dis 27: 1497-1501.
- Saeed M, Rahman A, Afzal A, et al. (2006) Role of transesophageal echocardiography guided cardioversion in patients with atrial fibrillation, previous left atrial thrombus and effective anticoagulation. Int J Cardiol 113: 401-405.
- Lip GYH, Hammerstingl C, Marin F, et al. (2016) Left atrial thrombus resolution in atrial fibrillation or flutter: Results of a prospective study with rivaroxaban (X-TRA) and a retrospective observational registry providing baseline data (CLOT-AF). Am Heart J 178: 126-134.
- Niku AD, Shiota T, Siegel RJ, et al. (2019) Prevalence and resolution of left atrial thrombus in patients with nonvalvular atrial fibrillation and flutter with oral anticoagulation. Am J Cardiol 123: 63-68.
- Lee WC, Fang CY, Chen YL, et al. (2019) Left atrial or left atrial appendage thrombus resolution after adjustment of oral anticoagulant treatment. J Stroke Cerebrovasc Dis 28: 90-96.
- Scarano M, Casale M, Mantini C, et al. (2017) Rivaroxaban as an effective alternative to warfarin in a patient with atrial fibrillation, thrombophilia and left atrial appendage thrombus: A case report. J Med Case Rep 11: 97.
- Fukuda S, Watanabe H, Shimada K, et al. (2011) Left atrial thrombus and prognosis after anticoagulation therapy in patients with atrial fibrillation. J of Cardiology 58: 266-277.
- Kawabata M, Goya M, Saski T, et al. (2017) Left atrial appendage thrombi formation in japanese non-valvular atrial fibrillation patients during anticoagulation therapy: Warfarin vs. Direct Oral Anticoagulants. Circ J 81: 645-651.
- Frenkel D, D'Amato SA, Al-Kazaz MA, et al. (2016) Prevalence of left atrial thrombus detection by transesophageal echocardiography: A comparison of continuous non-vitamin K antagonist oral anticoagulant versus warfarin therapy in patients undergoing catheter ablation for atrial fibrillation. JACC Clin Electrophysiol 2: 295-303.
- Watanabe T, Shinoda Y, Ikeoka K, et al. (2017) Dabigatran therapy resulting in the resolution of rivaroxaban-resistant left atrial appendage thrombi in patients with atrial fibrillation. Intern Med 56: 1977-1980.
- Koyama T, Otsuka Y, Kawahara M, et al. (2017) A left atrial appendage thrombus that developed during prophylactic low-dose dabigatran treatment resolved after switching to apixaban. Clinical Case Rep 5: 711-713.
- Fleddermann A, Eckert R, Muskala P, et al. (2019) Efficacy of direct acting oral anticoagulant drugs in treatment of left atrial appendage thrombus in patients with atrial fibrillation. Am J Cardiol 123: 57-62.
- Aschenberg W, Schulter M, Kremer P, et al. (1986) Transesophageal two-dimensional echocardiography for the detection of left atrial appendage thrombus. J Am Coll Cardiol 7: 163-166.
- Lee RJ, Bartzokis T, Yeoh TK, et al. (1991) Enhanced detection of intracardiac sources of cerebral emboli by transesophageal echocardiography. Stroke 22: 734-739.
- Stoddard MF, Dawkins PR, Prince CR, et al. (1995) Left atrial appendage thrombus is not uncommon in patients with acute atrial fibrillation and a recent embolic event: A transesophageal echocardiographic study. J Am Coll Cardiol 25: 452-459.
- de Bruijn SF, Agema WR, Lammers GJ, et al. (2006) Transesophageal echocardiography is superior to transthoracic echocardiography in management of patients of any age with transient ischemic attack of stroke. Stroke 37: 2531-2534.
- Maehama T, Okura H, Imai K, et al. (2010) Systemic inflammation and left atrial thrombus in patients with non-rheumatic atrial fibrillation. J Cardiol 56: 118-124.
- Seidl K, Rameken M, Drogemuller A, et al. (2002) Embolic events in patients with atrial fibrillation and effective anticoagulation: Value of transesophageal echocardiography to guide direct-current cardioversion. Final results of the Ludwigshafen Observational Cardioversion Study. J Am Coll Cardiol 39: 1436-1442
- Shen X, Li H, Rovang K, et al. (2002) Prevalence of intra-atrial thrombi in atrial fibrillation patients with subtherapeutic international normalized ratios while taking conventional anticoagulation. Am J Cardiol 90: 660-662.
- Kawakami T, Kobayakawa H, Ohno H, et al. (2013) Resolution of left atrial appendage thrombus with apixaban. Thrombosis Journal 11: 26.
- Okada T, Takaekou Y, Idei N, et al. (2017) Resolution of left atrial appendage thrombus with apixaban in a patient with heart failure. Intern Med 56: 2891-2894.
- Li Y, Lin J, Peng C (2016) Resolution of massive left atrial appendage thrombi with rivaroxaban before balloon mitral commissurotomy in severe mitral stenosis. Medicine 95: e5577.
- Kimura M, Wasaki Y, Ogawa H, et al. (2001) Effect of low-intensity warfarin therapy on left atrial thrombus resolution in patients with nonvalvular atrial fibrillation: A transesophageal echocardiographic study. Jpn Circ J 65: 271-274.
- Watanabe T, Shinoda Y, Ikeoka K, et al. (2017) Dabigatran exhibits low intensity of let atrial spontaneous echo contrast in patients with nonvalvular atrial fibrillation as compared with warfarin. Heart Vessels 32: 326-332.
- Yao X, Shah ND, Sangaralingham LR, et al. (2017) Non-Vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. J Am Coll Cardiol 69: 2779-2790.
- Kakkar AJ, Mueller I, Bassand JP, et al. (2012) International longitudinal registry of patients with atrial fibrillation at risk of stroke: Global Anticoagulant Registry in the FIELD (GARFIELD). Am Heart J 163: 13-19.
- O'Brien EC, Simon DN, Allen LA, et al. (2014) Reasons for warfarin discontinuation in the outcomes registry for better informed treatment of atrial fibrillation (ORBIT-AF). Am Heart J 168: 487-494.
- January CT, Wann LS, Calkins H, et al. (2019) 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation, 139.
- Reiner MF, Alexander Breitenstein, Erik W Holy, et al. (2017) Ticagrelor, but not clopidogrel active metabolite, displays antithrombotic properties in the left atrial endocardium. Eur Heart J 38: 916-919.
Corresponding Author
Katherine Cabral, PharmD, BCPS, BCCP, Capital Cardiology Associates, 106 New Scotland Ave, Albany NY 12208, USA, Tel: 518-694-7187.
Copyright
© 2022 Cabral KP. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.